-
PDF
- Split View
-
Views
-
Cite
Cite
Philip Bruggmann, Jean-Luc Richard, on behalf of the Swiss Hepatitis C Cohort Study Group, Birth year distribution in reported hepatitis C cases in Switzerland, European Journal of Public Health, Volume 25, Issue 1, February 2015, Pages 141–143, https://doi.org/10.1093/eurpub/cku095
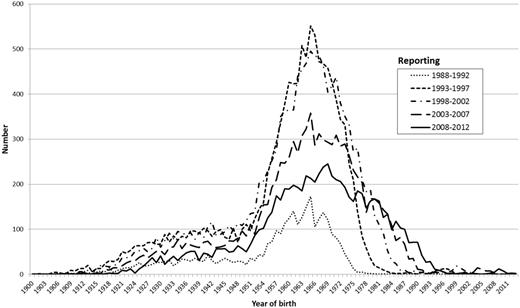
Close - Share Icon Share
Data of the national hepatitis C virus (HCV) notification system and the Swiss hepatitis C cohort study have been analysed for birth year distribution. Persons born between 1955 and 1974 are disproportionally affected by HCV, accounting for 61% of all reported infections. Over the course of the reporting period from 1988 to 2012, the majority of affected persons were born in the mid-60s and a sharply increasing proportion between 1975 and 1984 (from 0.6 to 19.5%). To enhance the so far insufficient HCV detection rates in Switzerland, additional testing strategies such as birth cohort screening must be further evaluated and discussed.
Introduction
Hepatitis C is a contagious liver disease caused by the hepatitis C virus (HCV). Chronic hepatitis C is a major cause of morbidity and mortality.1 In Switzerland, the estimated prevalence of hepatitis C is 0.8–1.8%.2 Although hepatitis C is a curable disease, treatment uptake rates are low (8%).3 In view of these factors and potentially fatal consequences of the disease, Switzerland faces a major public health threat: an epidemic of chronic hepatitis infections.4
New better tolerated HCV medication have the potential to cure the majority of those infected. To use this potential and to address the public health problem, one of the first steps is improving on detection rates. Detecting an infection early, followed by assessing and treating it if needed, has the potential to significantly improve secondary prevention of chronic hepatitis and to reduce HCV transmission.5 According to estimations in Switzerland, around 50% of those affected are not being tested and therefore not being aware of their infection.6 Until 2012 the official detection strategy in Switzerland has only covered a screening for blood donations.7
According to estimates by the US Centers for Disease Control and Prevention (CDC), persons born between 1945 and 1965 make up 27% of the American population, and account for 75% of HCV infections.8 Based on these insights, the CDC recommended in 2012 that in addition to risk-based and provider-initiated testing, every person born between 1945 and 1965 should be tested, irrespective of any risk behaviour.
The aim of this study is to analyse the birth year distribution among hepatitis C positive cases notified to the Swiss Federal Office of Public Health (FOPH).
Methods
Swiss Federal HCV notification system
Hepatitis C has been a notifiable disease in Switzerland since 1988. Every confirmed hepatitis C infection has to be reported to the FOPH, together with personal data of the affected person. A test is notified by a laboratory as confirmed positive if there is a positive antibody (confirmed by an immunoblot test), antigen or HCV RNA test.
Swiss hepatitis C cohort
The Swiss hepatitis C cohort study (SCCS) collects prospective data on adults aged >18 years with confirmed HCV infections through standardized questionnaires, clinical examinations and laboratory investigations.9 From 1 September 2000 to 17 October 2012, a total of 3882 people have been enrolled into the cohort.
Analysis
All cases reported by the mandatory hepatitis C notification system of the FOPH since its introduction in 1988 until the end of 2012 were analysed. Only reports from persons living in Switzerland were included in the analysis. Further on, we evaluated the distribution of birth year among the different periods of reporting (at 5-year intervals).
To validate the results of this analysis, we compared them with the participants in the SCCS on 17 October 2012.
Results
Between 1988 and 2012, 45 037 cases of hepatitis C have been reported to the FOPH. A total of 60.6% of all infections affected persons born between 1955 and 1974 (1955–1964: 30.4%; 1965–1974: 30.3%). Individuals born between 1945 and 1954 made up 10.7% of the HCV reported cases in Switzerland, whereas those born between 1975 and 1984 made up 10.4%, and 15.8% of the hepatitis C cases were born before 1945.
Number of reported hepatitis C cases by year of birth (1900–2012 cohorts) and period of reporting of the mandatory notification system in Switzerland, 1988–2012 (n = 45 037)
In the SCCS, of all included 3882 patients, 65% were born between 1955 and 1974 (1955–1964: 36%; n = 1124, 29%). In all, 25% of the cohort population were born before 1955, 9% after 1974.
Discussion
In Switzerland, individuals born between 1955 and 1974 make up 30% of the current (2011) population. Over the reporting periodfrom 1988 to 2012, the population with these birth years accounts for >60% of all reported hepatitis C cases. In comparison with the birth year distribution in the USA, the most affected birth year cohorts are on average 10 years younger in Switzerland. One reason for this discrepancy could be a later peak of intravenous drug use in Switzerland as a major mode of transmission. For Europe, there are no comparable data published.
Hepatitis C does not only seem to affect mainly one specific generation in Switzerland (people born between 1955 and 1974). In more recent reporting periods, there seems to also to be an increasing number of persons affected who were born between 1975 and 1984. This could point towards a correlation between the age of 20–40 years and an increased risk of infection, possibly due to increased risk of IV drug use behaviour in that age.
Owing to insufficient detection rates, the strategy of health-care provider–initiated identification of HCV infection among defined risk groups has been implemented recently.7 Year of birth is not included as a risk in this strategy.
If the recently implemented strategy of provider-initiated risk-stratified testing fails to substantially enhance HCV detection rates in Switzerland, birth year cohort screening could be a valuable add-on strategy. Birth year cohort screening has the advantage of being easier to talk about to the patient and has, therefore, the potential to be more readily accepted by both, physician and patient.
Looking at the birth year structure of the reported hepatitis C cases during the past 25 years, birth year cohort screening in addition to current detection strategies could be a way to enhance testing rates in a high-risk population in Switzerland. Cost-effectiveness studies are required to decide whether such a measure should be implemented and to determine how it should be orientated to achieve optimal success.10
Acknowledgements
The authors wish to thank the Swiss hepatitis C cohort study for providing the data evaluated in this study and the physicians and laboratories for reporting the data to the notification system.
Conflict of interest: The authors did not receive any funding in relation with this manuscript. P.B. has received project grants from and has served as advisory board member and speaker for Abbott, Janssen, Gilead, Merck and Roche. J.L.R. has no conflict of interests to declare.
61% of all reported hepatitis C cases in Switzerland are persons born between 1955 and 1974.
This most affected cohort is 10 years younger than the one in the USA.
Birth year cohort screening in addition to current detection strategies could enhance detection rates of HCV-infected people in Switzerland.




Comments