-
PDF
- Split View
-
Views
-
Cite
Cite
Shiau-Fang Chao, Meng-Hsuan Yu, COVID-19-Related Worries, Social Disruptions, and Depressive Symptoms Among Community-Dwelling Older Adults With Disabilities: What Makes the Difference?, The Journals of Gerontology: Series B, Volume 79, Issue 4, April 2024, gbab157, https://doi.org/10.1093/geronb/gbab157
Close - Share Icon Share
Abstract
This study explores how home- and community-based services use, coronavirus disease 2019 (COVID-19)-related worries, and social disruptions are related to the depressive symptoms of community-dwelling older adults with disabilities, and whether the associations differ by month of interview.
Data on a sample of 593 older individuals in Taiwan were collected between April and July 2020. Multiple regression analyses were performed to test the hypothesized relationships.
As the number of confirmed cases of COVID-19 in Taiwan continuously declined from April 2020, participants who were interviewed in May, June, and July experienced significantly fewer COVID-19-related worries and social disruptions than those interviewed in April. The month interviewed, representing the pandemic development phase of COVID-19, moderated the relationships between home-based service (HBS) use and COVID-19 worries. The month interviewed also moderated the association between COVID-19-related social disruptions and depressive symptoms.
Differences in the level of COVID-19-related worries between HBS users and nonusers were greatest in April, followed by May, and least in June and July, suggesting that the disparities between HBS users and nonusers attenuated over time. Perceived high COVID-19-related social disruptions were weakly and negatively correlated with depressive symptoms in April, but the relationship became moderately positive in May and strongly positive in June and July. These results supported the claim that the associations between COVID-19-related social disruptions and depressive symptoms can vary over time. Professionals who serve disabled older individuals in communities should be aware of their unstated needs and adopt strategies that are appropriate for the current stage of the COVID-19 pandemic to respond better to their needs and emotional state.
While coronavirus disease 2019 (COVID-19) continues to ravage around the world and causes millions of deaths, Taiwan has had remarkable success in combating the virus with only 685 confirmed cases (630 imported, 55 indigenous) and seven deaths as of December 2, 2020 (Taiwan Centers for Disease Control [TCDC], 2020). TCDC activated prompt border control and quarantine measures as early as December 31, 2019 (Central Epidemic Command Center [CECC], 2020a). As of March 12, when COVID-19 was finally characterized as a pandemic by the World Health Organization, the Taiwanese government implemented stricter regulations (Ministry of Health and Welfare [MOHW], 2020a), such as banning public gatherings of over 100 people indoors and 500 people outdoors and requiring the public to wear masks on public transportation. On February 4, 2020, MOHW issued guidelines for home-based and community-based programs in response to the COVID-19 pandemic (CECC, 2020b). Programs for older adults in community care centers, such as health promotion programs, were banned in 10 of 22 cities or counties in Taiwan from mid-March 2020. Congregate meal services were replaced by meal delivery services in order to minimize the risk of infection.
All of the above efforts have contributed to the successful control of the pandemic throughout the country. Although the government of Taiwan has done a remarkable job in controlling the COVID-19 pandemic, older adults in Taiwan still suffer from a higher infection fatality rate than their younger counterparts. Because over 90% of the confirmed cases were imported by younger or middle-aged business travelers, international students, or immigrant workers, only approximately 10% of confirmed cases involved people aged 60 and older. However, that latter group has accounted for over 50% of total mortalities in Taiwan (four out of seven deaths; TCDC, 2020). In addition to the high infection fatality rate, the COVID-19 pandemic exacerbates the existing health, social, and financial disparities of older people by unequal access to health care, disruption to their usual services, strengthened internal and external ageism, and the reduction of opportunities to acquire essential housing, income, and savings, on which they depend, making them particularly vulnerable to COVID-19 (Miller, 2020; Morrow-Howell et al., 2020).
Older individuals are highly heterogeneous and may be variously affected by the COVID-19 pandemic. Among the aging population, disabled older persons who live in communities and rely on formal services may suffer from additional challenges to those suffered by institutionalized older individuals as they try to meet their basic needs or maintain their daily routine during the pandemic (Abrashkin et al., 2020; Ebor et al., 2020). Disability in older people generally refers to an inability to carry out everyday activities that are necessary to live independently (Millán-Calenti et al., 2010). Activities of daily living (ADL) or instrumental activities of daily living (IADL) are the two most widely used measures of late-life disability in the gerontology literature. ADL comprises basic daily self-care activities such as bathing, dressing, or toileting, and IADL includes more complex sets of independent living activities, such as shopping, food preparation, or housekeeping (Millán-Calenti et al., 2010). By mid-2020, 153,878 home-based service (HBS) recipients, over 80% of whom were aged 65 or older, were served by 28,317 front-line workers in Taiwan. At the same time, approximately 14,000 older adults were served in 355 day care centers, and more than 120,000 community-dwelling older adults received congregate or home-delivered meals that were by community care centers (MOHW, 2020b, 2021). HBS users may experience particular stress under COVID-19. They are being cared by front-line home care professionals who are also at high risk of infection, but they have no way to evade the risk because they depend on hands-on care to support them at home (Cohen & Tavares, 2020). For community-based service (CBS) users, the suspension of congregate meal programs can impede older adults with functional limitations from receiving the nutritious food that they need, worsening their physical deficits. The closure of community care centers may limit disabled older persons’ access to regular programs and preferred activities, contributing to social isolation (Ameis et al., 2020).
As a large-scale infectious disease, the COVID-19 pandemic has a significant and persistent impact on daily life and the social interaction of individuals, making it unique among stressors in late life, which include natural disasters and negative life events (such as bereavement; Birditt et al., 2021). Therefore, findings concerning stressors that link negative events, emotional responses, and corresponding depressive symptoms may not be applicable to this epidemic. Studies of the adult population suggest that functional impairment may exacerbate an individual’s depressive symptoms during the COVID-19 pandemic by increasing stress (Gallagher et al., 2020). However, the empirical evidence on the influence of COVID-19 on the depressive symptoms of older adults is inconsistent. For instance, research of a Spanish sample indicated that older adults experienced fewer depressive symptoms than younger adults during the COVID-19 (García-Portilla et al., 2020). According to a U.S. study, older persons are less likely to report increased depression after the onset of the pandemic (Krendl & Perry, 2020). In contrast, researchers in China have found that older adults express greater psychological distress during COVID-19 than middle-aged adults (Qiu et al., 2020). As relevant studies have largely focused on the general older population, how disabled older residents in communities experience COVID-19-related stress and the effect of the pandemic on their depressive symptoms have been understudied. Moreover, whether the COVID-19 has a short-term or long-term effect on the depressive symptoms of disabled older individuals remains unknown (Krendl & Perry, 2020).
Basevitz et al. (2008) defined worry as the cognitive component and disruptions as the behavioral element of anxiety concerning uncertainty associated with current or future negative events. Based on this definition, this work conceptualizes the emotional response to COVID-19 as having two components—COVID-19-related worries and COVID-19-related social disruptions. The manifestation of some worry is regarded as normal. However, unremitting and excessive worry can be pathological and is associated with various mental or emotional disorders, such as depression (Basevitz et al., 2008). With respect to COVID-19-related worries, older adults in the United States experienced increasing pandemic-related worries from March 2020 to July 2020 (Panchal et al., 2020). However, they were less worried than their younger counterparts about COVID-19, and their mental health was less likely to be affected by such worries (Barber & Kim, 2020; Panchal et al., 2020). Similarly, community-dwelling older persons experience fewer COVID-19-related disruptions than younger adults and report lower levels of stress and negative affect in relation to those disruptions (Carney et al., 2020).
Theoretical Framework
The model of strength and vulnerability integration (SAVI) that was proposed by Charles (2010) suggests that old age is associated with strengths and vulnerabilities in the emotional well-being of an individual when facing a stressful situation, which depends on the type and the time course of stressors and the resources available to execute coping strategies. When the situation allows older adults to employ age-related improvements in attentional strategies, appraisals, or behaviors to avoid stressors, the impact of a negative event on emotional well-being can be minimized or diminished. However, when a stressor is unavoidable, the reduced physiological flexibility that comes with age can exacerbate the detrimental effect of continuous exposure to it (Birditt et al., 2021). Additionally, the varying time course of the adverse event can elicit different emotional intensity and affective arousal in older individuals. Older adults may exhibit high levels of physiological reactivity in the midst of a stressful event, inhibiting their implementation of emotional regulation strategies or behaviors, eliminating the age-related advantages in subjective emotional experience. After a stressful event has passed, the reduced psychological reactivity enables older individuals effectively to implement relevant strategies or behaviors, causing them to exhibit better emotional well-being than younger adults (Birditt et al., 2021; Young et al., 2021). Lastly, physical health status can condition an older person’s capacity to exercise emotional regulation mechanism. Thus, older persons with limited physical functioning may experience higher levels of stress upon encountering a negative event than their healthier counterparts, worsening their preexisting vulnerabilities (Charles, 2010).
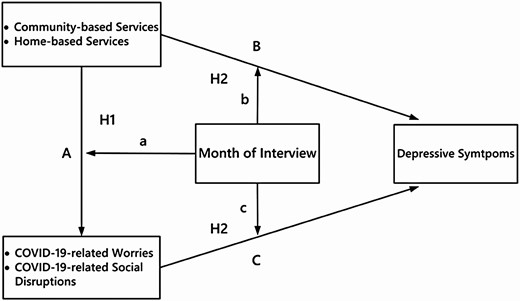
To the best of our knowledge, no study has investigated the effects of COVID-19 on community-dwelling older adults with disabilities and especially on those who rely on home- and community-based service (HCBS). Also, none of the gerontological literature addresses the intervening role of time, represented by different pandemic development phases of COVID-19, in determining the relationship between the emotional response to the pandemic and depressive symptoms. Guided by the SAVI model, this investigation proposes a conceptual framework as illustrated in Figure 1. Based on Figure 1, this study addresses the following aims: First, the extent to which the use of HCBS is related to COVID-19-related worries or social disruptions, and whether the associations vary over time (A × a); and second, how HCBS, COVID-19-related worries, and COVID-19-related social disruptions are associated with the symptoms of depression of disabled older adults, and whether these associations vary over time (B × b and C × c). We hypothesize the following: (a) HCBS users are more vulnerable to the pandemic than nonusers because they depend on formal services and the reduction or closure of those services can extensively disrupt their lives in their community. Thus, we expect that HCBS users will express more COVID-19-related worries and social disruptions during the outbreak stage of the pandemic, but the differences between users and nonusers are hypothesized to diminish thereafter. (b) The relationships of HCBS use, COVID-19-related worries, and social disruptions with depressive symptoms change with the development phase of the pandemic. The relationships are expected to be stronger at the outbreak stage of the pandemic and to weaken thereafter.
Method
Sample
Data on a sample of community-dwelling older adults in Taiwan were collected between April and July 2020. Inclusion criteria were an age of 60 years or older, more than 3 months of residence in the current community, ability to comprehend and respond to survey questions, and an inability to perform at least one of the six ADLs (bathing, grooming, dressing, toileting, functional mobility, and self-feeding) or one of the eight IADLs (shopping, food preparation, housekeeping, managing medications, using the phone, doing laundry, using public transportation, and managing finances). Quota sampling was used so the distribution of the study sample resembles that of the population of interest. Following the sampling procedures for national representative surveys that were developed by the Academic Sinica in Taiwan, a total of 358 townships in six municipalities, 16 counties, and six cities were stratified into 19 geographical strata using eight indicators, which were geographic location, percentages of the workforce employed in agriculture or manufacturing-related industries and at different occupational levels, age distribution within the population, education level, population density, and population growth rate over 5 years (Academic Sinica, Institute of Sociology, 2016). The older population in each geographical stratum and each municipality, county, or city was calculated. Researchers firstly contacted HCBS providers, local public servants, and volunteers who served disabled older persons in each geographical stratum and municipality, county, or city to ask them to assist with data collection. Those services providers, public servants, and volunteers who agreed to help then invited older individuals in their programs or communities to participate. The recruitment continued until the distribution of participants in each geographical stratum and municipality, county, or city was consistent with the population.
ADL and IADL disabilities are more common in individuals aged 75 years and older than in those younger. Over 75% of the population older than 75 years in Taiwan have no formal education and almost 40% of them suffer from some hearing loss (MOHW, 2019). Also, life in Taiwan gradually returned to normal after April 2020, so face-to-face interviews with members of the studied population were feasible. Data were collected by trained interviewers using questionnaires through face-to-face interviews. The study was approved by the institutional review board at the authors’ affiliation. Participation in this study was completely voluntary. Informed consent was obtained from all participants, who were given detailed information regarding the study process. Respondents were given New Taiwan dollars (NTD) 100 (near $3.5) after they completed the survey. The final study sample comprised 593 older adults—276 in April, 135 in May, and 182 in June and July. Table 1 presents the participant characteristics by month interviewed. Power analysis was conducted in G*Power 3.1 with 12 predictors, an alpha of 0.05, a power of 0.80, and, following Carney et al. (2020), a Pearson’s correlation coefficient between COVID-19 disruption and negative affect of 0.26. The results of the power analysis suggested that a sample size of over 482 yielded a power level of 0.99 (Faul et al., 2007). Therefore, the sample size in this investigation was considered to be sufficient.
Means, Standardized Deviations, and Percentages of Participant Characteristics by Month of Interview
| Variables . | April (N = 276) . | May (N = 135) . | June and July (N = 182) . | Total (N = 593) . | Group differences by month . |
|---|---|---|---|---|---|
| Age (61–100) | 79.67 (8.24) | 80.52 (7.08) | 81.62 (7.80) | 80.47 (7.88) | April < June and July* |
| Gender | |||||
| Female | 66.7% | 69.6% | 72.0% | 69.0% | n.s. |
| Education | |||||
| No formal education | 42.4% | 51.9% | 51.0% | 47.3% | = 11.397* |
| Elementary school | 31.2% | 23.7% | 33.5% | 30.1% | |
| Junior high school or above | 26.4% | 24.4% | 15.4% | 22.6% | |
| Marital status | |||||
| With a spouse | 39.1% | 37.0% | 27.5% | 35.0% | n.s. |
| Monthly income (NTD) | |||||
| Less than 5,999 | 22.5% | 18.5% | 27.5% | 23.2% | n.s. |
| 6,000–11,999 | 44.6% | 47.4% | 42.9% | 44.6% | |
| 12,000–17,999 | 16.7% | 18.5% | 17.6% | 17.3% | |
| 18,000 or above | 16.3% | 15.6% | 12.1% | 14.8% | |
| Cognitive functioning (0–10) | 8.13 (2.49) | 7.87 (2.28) | 7.81 (2.30) | 7.97 (2.39) | |
| ADL functioning (0–18) | 13.80 (4.28) | 13.91 (4.32) | 15.05 (4.10) | 14.19 (4.28) | April < June and July** |
| HBS user | 62.3% | 56.3% | 41.8% | 54.7% | = 18.901*** |
| CBS user | 42.4% | 51.1% | 64.3% | 51.0% | = 21.040*** |
| COVID-19-related worries (0–20) | 8.42 (6.33) | 6.46 (5.97) | 5.15 (6.43) | 5.53 (5.54) | April > May* April > June and July*** |
| COVID-19-related social disruptions (0–20) | 6.02 (5.71) | 4.93 (4.88) | 3.73 (5.08) | 4.44 (4.73) | April > June and July*** |
| Depressive symptoms (0–29) | 9.94 (6.55) | 10.29 (6.21) | 8.59 (7.14) | 9.63 (6.68) | n.s. |
| Variables . | April (N = 276) . | May (N = 135) . | June and July (N = 182) . | Total (N = 593) . | Group differences by month . |
|---|---|---|---|---|---|
| Age (61–100) | 79.67 (8.24) | 80.52 (7.08) | 81.62 (7.80) | 80.47 (7.88) | April < June and July* |
| Gender | |||||
| Female | 66.7% | 69.6% | 72.0% | 69.0% | n.s. |
| Education | |||||
| No formal education | 42.4% | 51.9% | 51.0% | 47.3% | = 11.397* |
| Elementary school | 31.2% | 23.7% | 33.5% | 30.1% | |
| Junior high school or above | 26.4% | 24.4% | 15.4% | 22.6% | |
| Marital status | |||||
| With a spouse | 39.1% | 37.0% | 27.5% | 35.0% | n.s. |
| Monthly income (NTD) | |||||
| Less than 5,999 | 22.5% | 18.5% | 27.5% | 23.2% | n.s. |
| 6,000–11,999 | 44.6% | 47.4% | 42.9% | 44.6% | |
| 12,000–17,999 | 16.7% | 18.5% | 17.6% | 17.3% | |
| 18,000 or above | 16.3% | 15.6% | 12.1% | 14.8% | |
| Cognitive functioning (0–10) | 8.13 (2.49) | 7.87 (2.28) | 7.81 (2.30) | 7.97 (2.39) | |
| ADL functioning (0–18) | 13.80 (4.28) | 13.91 (4.32) | 15.05 (4.10) | 14.19 (4.28) | April < June and July** |
| HBS user | 62.3% | 56.3% | 41.8% | 54.7% | = 18.901*** |
| CBS user | 42.4% | 51.1% | 64.3% | 51.0% | = 21.040*** |
| COVID-19-related worries (0–20) | 8.42 (6.33) | 6.46 (5.97) | 5.15 (6.43) | 5.53 (5.54) | April > May* April > June and July*** |
| COVID-19-related social disruptions (0–20) | 6.02 (5.71) | 4.93 (4.88) | 3.73 (5.08) | 4.44 (4.73) | April > June and July*** |
| Depressive symptoms (0–29) | 9.94 (6.55) | 10.29 (6.21) | 8.59 (7.14) | 9.63 (6.68) | n.s. |
Note: COVID-19 = coronavirus disease 2019; ADL = activities of daily living; NTD = New Taiwan dollars; HBS = home-based services; CBS = community-based services; n.s. = not significant.
*p ≤ .05, **p ≤ .01, ***p ≤ .001.
Means, Standardized Deviations, and Percentages of Participant Characteristics by Month of Interview
| Variables . | April (N = 276) . | May (N = 135) . | June and July (N = 182) . | Total (N = 593) . | Group differences by month . |
|---|---|---|---|---|---|
| Age (61–100) | 79.67 (8.24) | 80.52 (7.08) | 81.62 (7.80) | 80.47 (7.88) | April < June and July* |
| Gender | |||||
| Female | 66.7% | 69.6% | 72.0% | 69.0% | n.s. |
| Education | |||||
| No formal education | 42.4% | 51.9% | 51.0% | 47.3% | = 11.397* |
| Elementary school | 31.2% | 23.7% | 33.5% | 30.1% | |
| Junior high school or above | 26.4% | 24.4% | 15.4% | 22.6% | |
| Marital status | |||||
| With a spouse | 39.1% | 37.0% | 27.5% | 35.0% | n.s. |
| Monthly income (NTD) | |||||
| Less than 5,999 | 22.5% | 18.5% | 27.5% | 23.2% | n.s. |
| 6,000–11,999 | 44.6% | 47.4% | 42.9% | 44.6% | |
| 12,000–17,999 | 16.7% | 18.5% | 17.6% | 17.3% | |
| 18,000 or above | 16.3% | 15.6% | 12.1% | 14.8% | |
| Cognitive functioning (0–10) | 8.13 (2.49) | 7.87 (2.28) | 7.81 (2.30) | 7.97 (2.39) | |
| ADL functioning (0–18) | 13.80 (4.28) | 13.91 (4.32) | 15.05 (4.10) | 14.19 (4.28) | April < June and July** |
| HBS user | 62.3% | 56.3% | 41.8% | 54.7% | = 18.901*** |
| CBS user | 42.4% | 51.1% | 64.3% | 51.0% | = 21.040*** |
| COVID-19-related worries (0–20) | 8.42 (6.33) | 6.46 (5.97) | 5.15 (6.43) | 5.53 (5.54) | April > May* April > June and July*** |
| COVID-19-related social disruptions (0–20) | 6.02 (5.71) | 4.93 (4.88) | 3.73 (5.08) | 4.44 (4.73) | April > June and July*** |
| Depressive symptoms (0–29) | 9.94 (6.55) | 10.29 (6.21) | 8.59 (7.14) | 9.63 (6.68) | n.s. |
| Variables . | April (N = 276) . | May (N = 135) . | June and July (N = 182) . | Total (N = 593) . | Group differences by month . |
|---|---|---|---|---|---|
| Age (61–100) | 79.67 (8.24) | 80.52 (7.08) | 81.62 (7.80) | 80.47 (7.88) | April < June and July* |
| Gender | |||||
| Female | 66.7% | 69.6% | 72.0% | 69.0% | n.s. |
| Education | |||||
| No formal education | 42.4% | 51.9% | 51.0% | 47.3% | = 11.397* |
| Elementary school | 31.2% | 23.7% | 33.5% | 30.1% | |
| Junior high school or above | 26.4% | 24.4% | 15.4% | 22.6% | |
| Marital status | |||||
| With a spouse | 39.1% | 37.0% | 27.5% | 35.0% | n.s. |
| Monthly income (NTD) | |||||
| Less than 5,999 | 22.5% | 18.5% | 27.5% | 23.2% | n.s. |
| 6,000–11,999 | 44.6% | 47.4% | 42.9% | 44.6% | |
| 12,000–17,999 | 16.7% | 18.5% | 17.6% | 17.3% | |
| 18,000 or above | 16.3% | 15.6% | 12.1% | 14.8% | |
| Cognitive functioning (0–10) | 8.13 (2.49) | 7.87 (2.28) | 7.81 (2.30) | 7.97 (2.39) | |
| ADL functioning (0–18) | 13.80 (4.28) | 13.91 (4.32) | 15.05 (4.10) | 14.19 (4.28) | April < June and July** |
| HBS user | 62.3% | 56.3% | 41.8% | 54.7% | = 18.901*** |
| CBS user | 42.4% | 51.1% | 64.3% | 51.0% | = 21.040*** |
| COVID-19-related worries (0–20) | 8.42 (6.33) | 6.46 (5.97) | 5.15 (6.43) | 5.53 (5.54) | April > May* April > June and July*** |
| COVID-19-related social disruptions (0–20) | 6.02 (5.71) | 4.93 (4.88) | 3.73 (5.08) | 4.44 (4.73) | April > June and July*** |
| Depressive symptoms (0–29) | 9.94 (6.55) | 10.29 (6.21) | 8.59 (7.14) | 9.63 (6.68) | n.s. |
Note: COVID-19 = coronavirus disease 2019; ADL = activities of daily living; NTD = New Taiwan dollars; HBS = home-based services; CBS = community-based services; n.s. = not significant.
*p ≤ .05, **p ≤ .01, ***p ≤ .001.
Measures
Month of interview
As can be seen in Supplementary Figure 1 (TCDC, 2020), the number of confirmed cases in Taiwan reached a peak in March 2020. In April, the number of imported cases began to decline but a resurgence of domestic cases occurred in the middle of that month. Since early May, no domestic confirmed case has been reported and cases have only been occasionally imported and identified by COVID-19 testing at airports or during travelers’ quarantine period. Therefore, pandemic-related bans began to be loosened from May, and all daycare centers as well as community care centers reopened by the end of June. After June, life in Taiwan gradually returned to normal, so the phenomena of interest—COVID-19-related worries or social disruptions—were considered not to differ between June and July. Based on the trend of confirmed cases, April, May, and June and July 2020 are specified as the outbreak period, the control and loosening period, and the reopening period in this study, respectively, representing different pandemic development phases in Taiwan. The interview month was coded as one variable (1 = April; 2 = May; 3 = June and July) in the analyses to explore the effect of time.
Home- and community-based service use
In this study, home care, in-home respite care, and in-home rehabilitation are all regarded as HBS. Daycare, community care center, meal delivery, congregate meal services, volunteer visits, and greeting calls are regarded as CBS. Respondents were asked to report which HCBS they were using. Responses were separated into two dichotomous variables. People who used at least one of the above-listed HBS were identified as HBS users (1 = HBS users, 0 = non-HBS users); those who used at least one of the CBS were identified as CBS users (1 = CBS users, 0 = non-CBS users).
COVID-19-related worries
The perceived stress and worries of older adults that were related to the COVID-19 pandemic were measured on a five-item scale, applied to various situations that were encountered during the COVID-19 outbreak. This 5-point Likert-type scale, ranging from 0 (never) to 4 (always), was developed by researchers from the scale of perceived source of stress that was used in the 2003 SARS epidemic (Wong et al., 2007). Respondents were asked to report the levels of (a) worry about the pandemic, (b) panic about the pandemic, (c) worry about their own risk of becoming infected, (d) worry about the spread of the pandemic within the country, and (e) worry about the detrimental impact of COVID-19 infection on interpersonal relationships. A confirmatory factor analysis (CFA) was carried out to examine the construct validity of this instrument with the study sample. The results of suggested that a one-factor model yielded an acceptable fit ( = 192.8, p < .001; normed fit index [NFI] = 0.93; incremental fit index [IFI] = 0.93; comparative fit index [CFI] = 0.93) and all five items yielded factor loadings greater than 0.7. With Cronbach’s α = 0.933, the measure also had excellent reliability. After the psychometric properties have been confirmed, the scores for the five items were summed (range: 0–20). A higher total score represents greater COVID-19-related worries.
COVID-19-related social disruptions
COVID-19-related social disruptions were measured using a five-item scale that was adopted from Wong et al. (2007). Respondents were asked to report social disruptions to their daily lives, including (a) interruptions in daily routines, (b) reduced frequency of taking public transportation, (c) reduced frequency of outdoor activities, (d) reduced frequency of meeting friends, and (e) shortages in daily goods, due to COVID-19. Each item was scored from 0 (never) to 4 (always). For construct validity, results of the CFA revealed that a one-factor model yielded a satisfactory fit ( = 75.9, p < .001; NFI = 0.96; IFI = 0.96; CFI = 0.96), and the five items had factor loadings greater than 0.5. The instrument also showed good internal consistency (α = 0.894), and their scores were then summed (range: 0–20). A higher total score indicated greater disruption in the lives of older adults as a result of the pandemic.
Depressive symptoms
The 10-item Center for Epidemiologic Studies—Depression (CES-D) scale (Radloff, 1977) was used to measure depressive symptoms. The CES-D scale has been proved to be a valid and reliable instrument for measuring depressive symptoms of older Chinese adults (Cheng & Chan, 2005). Participants were asked whether or not, and how often, they have had such symptoms in the preceding week as no appetite, bad quality of sleep, or a sense of loneliness. The scores for the 10 items were summed (range: 0–30), and a higher total score indicates more depressive symptoms (α = 0.868).
Personal factors
Seven personal factors were considered in the analyses to determine their effects on older adults’ depressive symptoms. They were age (years), gender (0 = male; 1 = female), and level of education (1 = illiterate or no formal education, reference group; 2 = elementary school; 3 = high school or above). Marital status was a dummy variable, coded 0 for without a spouse and 1 for with a spouse. Monthly income was coded using intervals (1 = below NTD 5,999; 2 = between NTD 6,000 and 11,999; 3 = between NTD 12,000 and 17,999; 4 = above NTD 18,000). ADL functioning was measured using the Barthel Index and reverse-recorded so a higher score indicated better ADL functioning (Collin et al., 1988). Cognitive status was measured using the 10-item Short Portable Mental Status Questionnaire (Pfeiffer, 1975). A higher score indicated better cognitive functioning (range: 0–10).
Analytical Approach
The first research hypothesis explores whether the month of interview moderates the relationships between CBS or HBS use and COVID-19-related worries or social disruptions (A × a in Figure 1). To test the first research hypothesis, a three-step multiple regression was performed. First, demographic characteristics and month of interview were input as predictors of COVID-19-related worries or social disruptions. Second, HBS and CBS status were incorporated into models. Third, interactions between the month of interview and HBS use and between the month of interview and CBS use were then added into models. The second research hypothesis elucidates whether the month of interview moderates the associations (a) between CBS or HBS use and depressive symptoms (B × b in Figure 1), when demographic characteristics and the degrees of COVID-19-related worries and social disruptions held constant; as well as (b) between COVID-19-related worries or social disruptions and depressive symptoms (C × c in Figure 1), controlling for demographic characteristics and CBS and HBS use status. To test the second research hypothesis, the same procedures were carried out to determine whether the month of interview moderated the relationships between HCBS use, COVID-19-related worries, COVID-19-related social disruptions, and depressive symptoms. The moderation analyses were performed using the PROCESS macro for SPSS that was developed by Hayes (2013). Key variables that were used in the moderation analyses were centered before the interaction term was generated to avoid multicollinearity (Aiken & West, 1991). In addition, the variance inflation factor (VIF) and tolerance values were examined in all models. Values greater than 10 for VIF and smaller than 0.1 for tolerance signify the potential problem of multicollinearity, which could produce large standard errors and lead to biased estimates in the related independent variables (Keith, 2019). Values for VIF in all variables and models in this study ranged between 1.104 and 2.578, and tolerances ranged between 0.397 and 0.874, suggesting that multicollinearity should not be a concern.
Results
Participant Characteristics by Month of Interview
Table 1 presents the characteristics of the study participants by month of interview. The average age of all participants was 80.47 (SD = 7.88) and 69% of the sample was female. Close to half (47.3%) of the respondents were illiterate or had no formal education, and 30.1% had elementary school education. Only 35% of the participants had a spouse, and nearly half had a monthly income of between NTD 6,000 and 11,900. The average cognitive functioning and average ADL were 7.97 and 14.19, respectively. About 46.5% of the respondents were interviewed in April, 22.8% in May, and 30.7% in June or July 2020. About 54.7% of the interviewees were HBS users and 51.0% were CBS users. The mean scores for COVID-19-related worries, COVID-19-related social disruptions, and depressive symptoms were 5.53, 4.44, and 9.63, respectively. The results of an analysis of variance and post hoc tests using the Scheffé method revealed that participants who were interviewed in April were significantly younger and had better ADL functioning than those who were interviewed in June and July. Respondents who were interviewed in April or May also expressed more COVID-19-related worries and more COVID-19-related social disruptions than their counterparts who were interviewed in June and July. Results of chi-square tests showed that the percentage of HBS users or CBS users among the interviewees varied with the month. Using a criterion of adjusted standardized residual value of ±2 (Sharpe, 2015), more HBS users and fewer CBS users were interviewed in April than in June and July.
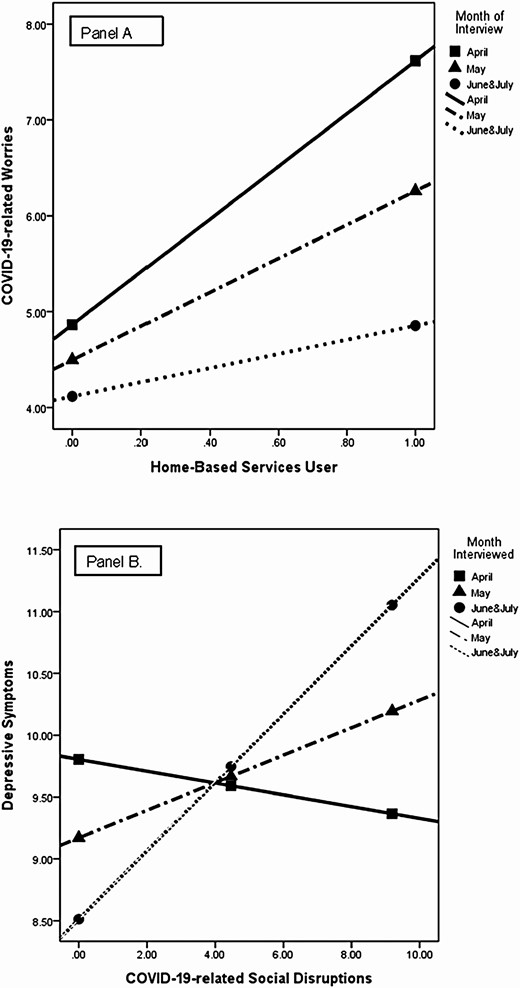
HCBS Use, COVID-19-Related Worries, and COVID-19-Related Social Disruptions: Month of Interview as a Moderator
Models 1–3 in Table 2 reveal how the month of interview and HCBS use were related to COVID-19-related worries. In Model 1, being female, having a spouse, and having better cognitive functioning were associated with more COVID-19-related worries. Older adults with a monthly income of less than NTD 5,999 had more COVID-19-related worries than those with a monthly income of NTD 6,000–11,999. Participants reported significantly fewer COVID-19-related worries over time. In Model 2, HBS users had more COVID-19-related worries than non-HBS users. In Model 3, the interaction term between HBS use and COVID-19-related worries was significant, confirming that moderation by month of interview. As shown in Figure 2 (Panel A), the differences between HBS users and non-HBS users with respect to COVID-19-related worries varied by month and attenuated over time (β = −1.189, p < .05). Specifically, the difference between the levels of COVID-19-related worry of HBS users and non-HBS users followed the order April > May > June and July 2020.
HCBS Use and COVID-19-Related Worries or Social Disruptions: Month of Interview as a Moderator
| . | COVID-19 worries . | COVID-19 social disruptions . | ||||
|---|---|---|---|---|---|---|
| . | Model 1 . | Model 2 . | Model 3 . | Model 4 . | Model 5 . | Model 6 . |
| Predictor variables . | b (SE) . | b (SE) . | b (SE) . | b (SE) . | b (SE) . | b (SE) . |
| Age | −0.055 (0.030) | −0.066 (0.030)* | −0.075 (0.030)* | −0.065 (0.026)* | −0.069 (0.026)** | −0.070 (0.027)** |
| Gender (ref. male) | 1.337 (0.494)** | 1.396 (0.496)** | 1.412 (0.494)** | 0.359 (0.433) | 0.371 (0.439) | 0.370 (0.440) |
| Education (ref. no formal education) | ||||||
| Elementary school | −0.389 (0.518) | −0.351 (0.512) | −0.363 (0.511) | −0.201 (0.454) | −0.190 (0.454) | −0.194 (0.455) |
| Junior high school or above | −0.771 (0.598) | −0.902 (0.596) | −0.820 (0.595) | 0.403 (0.524) | 0.354 (0.528) | 0.359 (0.529) |
| Marital status (ref. w/o a spouse) | 1.170 (0.481)* | 1.457 (0.492)** | 1.399 (0.492)** | 0.614 (0.422) | 0.699 (0.436) | 0.698 (0.438) |
| Monthly income (ref. less than NTD 5,999) | ||||||
| 6,000 to 11,999 | −1.311 (0.552)* | −1.282 (0.546)* | −1.217 (0.548)* | −0.786 (0.484) | −0.779 (0.484) | −0.783 (0.488) |
| 12,000 to 17,999 | −0.801 (0.687) | −0.772 (0.682) | −0.671 (0.682) | −0.259 (0.602) | −0.255 (0.605) | −0.251 (0.607) |
| 18,000 or above | −0.433 (0.728) | −0.394 (0.725) | −0.233 (0.727) | −0.352 (0.638) | −0.346 (0.642) | −0.344 (0.647) |
| Cognitive functioning | 0.379 (0.104)*** | 0.329 (0.104)** | 0.322 (0.104)** | 0.356 (0.091)*** | 0.341 (0.092)*** | 0.341 (0.093)*** |
| ADL functioning | −0.037 (0.055) | 0.042 (0.058) | 0.043 (0.058) | 0.099 (0.048)* | 0.125 (0.052)* | 0.126 (0.052)* |
| Month of interview | −1.210 (0.253)*** | −1.051 (0.256)*** | −1.095 (0.256)*** | −0.767 (0.222)*** | −0.712 (0.226)** | −0.713 (0.228)** |
| HBS user (ref. no) | 1.738 (0.478)*** | 1.753 (0.477)*** | 0.559 (0.423) | 0.557 (0.424) | ||
| CBS user (ref. no) | −0.102 (0.461) | −0.146 (0.461) | −0.076 (0.408) | −0.084 (0.410) | ||
| HBS user × Month of interview | −1.189 (0.526)* | −0.100 (0.468) | ||||
| CBS user × Month of interview | 0.096 (0.528) | −0.075 (0.470) | ||||
| F (df) | 6.592 (11, 567)*** | 6.776 (13, 565)*** | 6.303 (15, 563)*** | 7.006 (11, 567)*** | 6.076 (13, 565)*** | 5.252 (15, 563)*** |
| R2 | 0.113 | 0.135 | 0.144 | 0.120 | 0.123 | 0.123 |
| . | COVID-19 worries . | COVID-19 social disruptions . | ||||
|---|---|---|---|---|---|---|
| . | Model 1 . | Model 2 . | Model 3 . | Model 4 . | Model 5 . | Model 6 . |
| Predictor variables . | b (SE) . | b (SE) . | b (SE) . | b (SE) . | b (SE) . | b (SE) . |
| Age | −0.055 (0.030) | −0.066 (0.030)* | −0.075 (0.030)* | −0.065 (0.026)* | −0.069 (0.026)** | −0.070 (0.027)** |
| Gender (ref. male) | 1.337 (0.494)** | 1.396 (0.496)** | 1.412 (0.494)** | 0.359 (0.433) | 0.371 (0.439) | 0.370 (0.440) |
| Education (ref. no formal education) | ||||||
| Elementary school | −0.389 (0.518) | −0.351 (0.512) | −0.363 (0.511) | −0.201 (0.454) | −0.190 (0.454) | −0.194 (0.455) |
| Junior high school or above | −0.771 (0.598) | −0.902 (0.596) | −0.820 (0.595) | 0.403 (0.524) | 0.354 (0.528) | 0.359 (0.529) |
| Marital status (ref. w/o a spouse) | 1.170 (0.481)* | 1.457 (0.492)** | 1.399 (0.492)** | 0.614 (0.422) | 0.699 (0.436) | 0.698 (0.438) |
| Monthly income (ref. less than NTD 5,999) | ||||||
| 6,000 to 11,999 | −1.311 (0.552)* | −1.282 (0.546)* | −1.217 (0.548)* | −0.786 (0.484) | −0.779 (0.484) | −0.783 (0.488) |
| 12,000 to 17,999 | −0.801 (0.687) | −0.772 (0.682) | −0.671 (0.682) | −0.259 (0.602) | −0.255 (0.605) | −0.251 (0.607) |
| 18,000 or above | −0.433 (0.728) | −0.394 (0.725) | −0.233 (0.727) | −0.352 (0.638) | −0.346 (0.642) | −0.344 (0.647) |
| Cognitive functioning | 0.379 (0.104)*** | 0.329 (0.104)** | 0.322 (0.104)** | 0.356 (0.091)*** | 0.341 (0.092)*** | 0.341 (0.093)*** |
| ADL functioning | −0.037 (0.055) | 0.042 (0.058) | 0.043 (0.058) | 0.099 (0.048)* | 0.125 (0.052)* | 0.126 (0.052)* |
| Month of interview | −1.210 (0.253)*** | −1.051 (0.256)*** | −1.095 (0.256)*** | −0.767 (0.222)*** | −0.712 (0.226)** | −0.713 (0.228)** |
| HBS user (ref. no) | 1.738 (0.478)*** | 1.753 (0.477)*** | 0.559 (0.423) | 0.557 (0.424) | ||
| CBS user (ref. no) | −0.102 (0.461) | −0.146 (0.461) | −0.076 (0.408) | −0.084 (0.410) | ||
| HBS user × Month of interview | −1.189 (0.526)* | −0.100 (0.468) | ||||
| CBS user × Month of interview | 0.096 (0.528) | −0.075 (0.470) | ||||
| F (df) | 6.592 (11, 567)*** | 6.776 (13, 565)*** | 6.303 (15, 563)*** | 7.006 (11, 567)*** | 6.076 (13, 565)*** | 5.252 (15, 563)*** |
| R2 | 0.113 | 0.135 | 0.144 | 0.120 | 0.123 | 0.123 |
Note: COVID-19 = coronavirus disease 2019; ADL = activities of daily living; NTD = New Taiwan dollars; HBS = home-based services; CBS = community-based services; HCBS = home- and community-based service.
*p ≤ .05, **p ≤ .01, ***p ≤ .001.
HCBS Use and COVID-19-Related Worries or Social Disruptions: Month of Interview as a Moderator
| . | COVID-19 worries . | COVID-19 social disruptions . | ||||
|---|---|---|---|---|---|---|
| . | Model 1 . | Model 2 . | Model 3 . | Model 4 . | Model 5 . | Model 6 . |
| Predictor variables . | b (SE) . | b (SE) . | b (SE) . | b (SE) . | b (SE) . | b (SE) . |
| Age | −0.055 (0.030) | −0.066 (0.030)* | −0.075 (0.030)* | −0.065 (0.026)* | −0.069 (0.026)** | −0.070 (0.027)** |
| Gender (ref. male) | 1.337 (0.494)** | 1.396 (0.496)** | 1.412 (0.494)** | 0.359 (0.433) | 0.371 (0.439) | 0.370 (0.440) |
| Education (ref. no formal education) | ||||||
| Elementary school | −0.389 (0.518) | −0.351 (0.512) | −0.363 (0.511) | −0.201 (0.454) | −0.190 (0.454) | −0.194 (0.455) |
| Junior high school or above | −0.771 (0.598) | −0.902 (0.596) | −0.820 (0.595) | 0.403 (0.524) | 0.354 (0.528) | 0.359 (0.529) |
| Marital status (ref. w/o a spouse) | 1.170 (0.481)* | 1.457 (0.492)** | 1.399 (0.492)** | 0.614 (0.422) | 0.699 (0.436) | 0.698 (0.438) |
| Monthly income (ref. less than NTD 5,999) | ||||||
| 6,000 to 11,999 | −1.311 (0.552)* | −1.282 (0.546)* | −1.217 (0.548)* | −0.786 (0.484) | −0.779 (0.484) | −0.783 (0.488) |
| 12,000 to 17,999 | −0.801 (0.687) | −0.772 (0.682) | −0.671 (0.682) | −0.259 (0.602) | −0.255 (0.605) | −0.251 (0.607) |
| 18,000 or above | −0.433 (0.728) | −0.394 (0.725) | −0.233 (0.727) | −0.352 (0.638) | −0.346 (0.642) | −0.344 (0.647) |
| Cognitive functioning | 0.379 (0.104)*** | 0.329 (0.104)** | 0.322 (0.104)** | 0.356 (0.091)*** | 0.341 (0.092)*** | 0.341 (0.093)*** |
| ADL functioning | −0.037 (0.055) | 0.042 (0.058) | 0.043 (0.058) | 0.099 (0.048)* | 0.125 (0.052)* | 0.126 (0.052)* |
| Month of interview | −1.210 (0.253)*** | −1.051 (0.256)*** | −1.095 (0.256)*** | −0.767 (0.222)*** | −0.712 (0.226)** | −0.713 (0.228)** |
| HBS user (ref. no) | 1.738 (0.478)*** | 1.753 (0.477)*** | 0.559 (0.423) | 0.557 (0.424) | ||
| CBS user (ref. no) | −0.102 (0.461) | −0.146 (0.461) | −0.076 (0.408) | −0.084 (0.410) | ||
| HBS user × Month of interview | −1.189 (0.526)* | −0.100 (0.468) | ||||
| CBS user × Month of interview | 0.096 (0.528) | −0.075 (0.470) | ||||
| F (df) | 6.592 (11, 567)*** | 6.776 (13, 565)*** | 6.303 (15, 563)*** | 7.006 (11, 567)*** | 6.076 (13, 565)*** | 5.252 (15, 563)*** |
| R2 | 0.113 | 0.135 | 0.144 | 0.120 | 0.123 | 0.123 |
| . | COVID-19 worries . | COVID-19 social disruptions . | ||||
|---|---|---|---|---|---|---|
| . | Model 1 . | Model 2 . | Model 3 . | Model 4 . | Model 5 . | Model 6 . |
| Predictor variables . | b (SE) . | b (SE) . | b (SE) . | b (SE) . | b (SE) . | b (SE) . |
| Age | −0.055 (0.030) | −0.066 (0.030)* | −0.075 (0.030)* | −0.065 (0.026)* | −0.069 (0.026)** | −0.070 (0.027)** |
| Gender (ref. male) | 1.337 (0.494)** | 1.396 (0.496)** | 1.412 (0.494)** | 0.359 (0.433) | 0.371 (0.439) | 0.370 (0.440) |
| Education (ref. no formal education) | ||||||
| Elementary school | −0.389 (0.518) | −0.351 (0.512) | −0.363 (0.511) | −0.201 (0.454) | −0.190 (0.454) | −0.194 (0.455) |
| Junior high school or above | −0.771 (0.598) | −0.902 (0.596) | −0.820 (0.595) | 0.403 (0.524) | 0.354 (0.528) | 0.359 (0.529) |
| Marital status (ref. w/o a spouse) | 1.170 (0.481)* | 1.457 (0.492)** | 1.399 (0.492)** | 0.614 (0.422) | 0.699 (0.436) | 0.698 (0.438) |
| Monthly income (ref. less than NTD 5,999) | ||||||
| 6,000 to 11,999 | −1.311 (0.552)* | −1.282 (0.546)* | −1.217 (0.548)* | −0.786 (0.484) | −0.779 (0.484) | −0.783 (0.488) |
| 12,000 to 17,999 | −0.801 (0.687) | −0.772 (0.682) | −0.671 (0.682) | −0.259 (0.602) | −0.255 (0.605) | −0.251 (0.607) |
| 18,000 or above | −0.433 (0.728) | −0.394 (0.725) | −0.233 (0.727) | −0.352 (0.638) | −0.346 (0.642) | −0.344 (0.647) |
| Cognitive functioning | 0.379 (0.104)*** | 0.329 (0.104)** | 0.322 (0.104)** | 0.356 (0.091)*** | 0.341 (0.092)*** | 0.341 (0.093)*** |
| ADL functioning | −0.037 (0.055) | 0.042 (0.058) | 0.043 (0.058) | 0.099 (0.048)* | 0.125 (0.052)* | 0.126 (0.052)* |
| Month of interview | −1.210 (0.253)*** | −1.051 (0.256)*** | −1.095 (0.256)*** | −0.767 (0.222)*** | −0.712 (0.226)** | −0.713 (0.228)** |
| HBS user (ref. no) | 1.738 (0.478)*** | 1.753 (0.477)*** | 0.559 (0.423) | 0.557 (0.424) | ||
| CBS user (ref. no) | −0.102 (0.461) | −0.146 (0.461) | −0.076 (0.408) | −0.084 (0.410) | ||
| HBS user × Month of interview | −1.189 (0.526)* | −0.100 (0.468) | ||||
| CBS user × Month of interview | 0.096 (0.528) | −0.075 (0.470) | ||||
| F (df) | 6.592 (11, 567)*** | 6.776 (13, 565)*** | 6.303 (15, 563)*** | 7.006 (11, 567)*** | 6.076 (13, 565)*** | 5.252 (15, 563)*** |
| R2 | 0.113 | 0.135 | 0.144 | 0.120 | 0.123 | 0.123 |
Note: COVID-19 = coronavirus disease 2019; ADL = activities of daily living; NTD = New Taiwan dollars; HBS = home-based services; CBS = community-based services; HCBS = home- and community-based service.
*p ≤ .05, **p ≤ .01, ***p ≤ .001.
(Panel A) Interaction of home-based services use with the month of interview in relation to COVID-19 worries and (Panel B) interaction of COVID-19 social disruptions with the month of interview in relation to depressive symptoms. COVID-19 = coronavirus disease 2019.
Models 4–6 in Table 2 provide analytical results concerning COVID-19-related social disruptions. According to Model 4, disabled older individuals who were younger and had better cognitive functioning experienced more COVID-19-related social disruptions. Like COVID-19-related worries, perceived COVID-19-related social disruptions declined over time. In Model 5, neither HBS nor CBS users differed in their level of COVID-19-related disruption from their nonuser counterparts. In Model 6, no significant interaction between the month of interview and HBS use or between the month of interview and CBS use was found.
HCBS Use, COVID-19-Related Worries, COVID-19-Related Social Disruptions, and Depressive Symptoms: Month of Interview as a Moderator
Table 3 presents whether the effects of HCBS use, COVID-19-related worries, and COVID-19-related social disruptions on depressive symptoms were moderated by the month of interview, after adjustment for demographic characteristics. Model 1 suggests that HBS users exhibited significantly more depressive symptoms than non-HBS users. Model 2 indicates that COVID-19-related worries were associated with more depressive symptoms. In Model 3, the interaction between the month of interview and HBS use was insignificant, suggesting that the difference between the levels of depression of HBS or CBS users and nonusers did not vary over time. Nevertheless, the month of interview and the extent of COVID-19-related social disruptions had a cross-over interactive effect on depressive symptoms according to Model 4 (β = 0.192, p < .05). A cross-over interactive effect occurs when the relationship between an independent variable and a dependent variable changes direction in a manner determined by the value of a third variable. Under these conditions, such interaction effects should be considered along with the main effects in order to elucidate more fully the relationships among variables (Grace-Martin, 2020). As shown in Figure 2 (Panel B), the association between levels of COVID-19-related social disruptions and depression reversed during the study period, canceling out the main effects of COVID-19-related social disruptions and month of interview. A high level of COVID-19-related disruption was related to fewer depressive symptoms in April, but more depressive in May, June, and July. Furthermore, the corresponding slope was steeper in June and July than in May, indicating that high disruption that arose from COVID-19 in the later stage of the pandemic had a more detrimental effect on the depressive symptoms of older persons with disabilities.
HCBS Use, COVID-19-Related Worries, or Social Disruptions and Depressive Symptoms: Month of Interview as a Moderator
| . | Depressive symptoms . | |||
|---|---|---|---|---|
| . | Model 1 . | Model 2 . | Model 3 . | Model 4 . |
| Predictor variables . | b (SE) . | b (SE) . | b (SE) . | b (SE) . |
| Age | −0.049 (0.035) | −0.031 (0.035) | −0.030 (0.035) | −0.028 (0.035) |
| Gender (ref. male) | 0.316 (0.583) | 0.117 (0.579) | 0.112 (0.580) | 0.073 (0.581) |
| Education (ref. no formal education) | ||||
| Elementary school | −0.894 (0.604) | −0.723 (0.596) | −0.720 (0.597) | −0.720 (0.597) |
| Junior high school or above | −1.620 (0.702)* | −1.392 (0.694)* | −1.400 (0.696)* | −1.422 (0.695)* |
| Marital status (ref. w/o a spouse) | −1.095 (0.583) | −1.343 (0.576)* | −1.338 (0.578)* | −1.325 (0.577)* |
| Monthly income (ref. less than NTD 5,999) | ||||
| 6,000–11,999 | 0.520 (0.644) | 0.704 (0.639) | 0.700 (0.644) | 0.689 (0.643) |
| 12,000–17,999 | 0.608 (0.802) | 0.538 (0.794) | 0.527 (0.797) | 0.560 (0.796) |
| 18,000 or above | 0.494 (0.854) | 0.515 (0.841) | 0.496 (0.848) | 0.534 (0.847) |
| Cognitive functioning | −0.293 (0.124)* | −0.390 (0.123)** | −0.390 (0.124)** | −0.376 (0.124)** |
| ADL functioning | −0.485 (0.070)*** | −0.508 (0.069)*** | −0.508 (0.069)*** | −0.509 (0.069)*** |
| Month of interview | −0.163 (0.300) | 0.092 (0.301) | 0.097 (0.303) | 0.087 (0.303) |
| HBS user (ref. no) | 2.320 (0.564)*** | 2.010 (0.565)*** | 2.006 (0.567)*** | 1.914 (0.569)*** |
| CBS user (ref. no) | 0.252 (0.543) | 0.276 (0.536) | 0.286 (0.539) | 0.288 (0.538) |
| COVID-19-related worries | 0.189 (0.069)** | 0.192(0.070)** | 0.158 (0.072)* | |
| COVID-19-related social disruptions | 0.074 (0.078) | 0.072 (0.079) | 0.113 (0.081) | |
| HBS user × Month of interview | 0.174 (0.621) | 0.243 (0.622) | ||
| CBS user × Month of interview | 0.026 (0.619) | −0.002 (0.619) | ||
| COVID-19-related worries × Month of interview | −0.129 (0.082) | |||
| COVID-19-related social disruptions × Month of interview | 0.192 (0.092)* | |||
| F (df) | 12.083 (13, 568)*** | 12.497 (15, 559)*** | 10.994 (17, 557)*** | 10.105 (19, 555)*** |
| R2 | 0.217 | 0.251 | 0.251 | 0.257 |
| . | Depressive symptoms . | |||
|---|---|---|---|---|
| . | Model 1 . | Model 2 . | Model 3 . | Model 4 . |
| Predictor variables . | b (SE) . | b (SE) . | b (SE) . | b (SE) . |
| Age | −0.049 (0.035) | −0.031 (0.035) | −0.030 (0.035) | −0.028 (0.035) |
| Gender (ref. male) | 0.316 (0.583) | 0.117 (0.579) | 0.112 (0.580) | 0.073 (0.581) |
| Education (ref. no formal education) | ||||
| Elementary school | −0.894 (0.604) | −0.723 (0.596) | −0.720 (0.597) | −0.720 (0.597) |
| Junior high school or above | −1.620 (0.702)* | −1.392 (0.694)* | −1.400 (0.696)* | −1.422 (0.695)* |
| Marital status (ref. w/o a spouse) | −1.095 (0.583) | −1.343 (0.576)* | −1.338 (0.578)* | −1.325 (0.577)* |
| Monthly income (ref. less than NTD 5,999) | ||||
| 6,000–11,999 | 0.520 (0.644) | 0.704 (0.639) | 0.700 (0.644) | 0.689 (0.643) |
| 12,000–17,999 | 0.608 (0.802) | 0.538 (0.794) | 0.527 (0.797) | 0.560 (0.796) |
| 18,000 or above | 0.494 (0.854) | 0.515 (0.841) | 0.496 (0.848) | 0.534 (0.847) |
| Cognitive functioning | −0.293 (0.124)* | −0.390 (0.123)** | −0.390 (0.124)** | −0.376 (0.124)** |
| ADL functioning | −0.485 (0.070)*** | −0.508 (0.069)*** | −0.508 (0.069)*** | −0.509 (0.069)*** |
| Month of interview | −0.163 (0.300) | 0.092 (0.301) | 0.097 (0.303) | 0.087 (0.303) |
| HBS user (ref. no) | 2.320 (0.564)*** | 2.010 (0.565)*** | 2.006 (0.567)*** | 1.914 (0.569)*** |
| CBS user (ref. no) | 0.252 (0.543) | 0.276 (0.536) | 0.286 (0.539) | 0.288 (0.538) |
| COVID-19-related worries | 0.189 (0.069)** | 0.192(0.070)** | 0.158 (0.072)* | |
| COVID-19-related social disruptions | 0.074 (0.078) | 0.072 (0.079) | 0.113 (0.081) | |
| HBS user × Month of interview | 0.174 (0.621) | 0.243 (0.622) | ||
| CBS user × Month of interview | 0.026 (0.619) | −0.002 (0.619) | ||
| COVID-19-related worries × Month of interview | −0.129 (0.082) | |||
| COVID-19-related social disruptions × Month of interview | 0.192 (0.092)* | |||
| F (df) | 12.083 (13, 568)*** | 12.497 (15, 559)*** | 10.994 (17, 557)*** | 10.105 (19, 555)*** |
| R2 | 0.217 | 0.251 | 0.251 | 0.257 |
Notes: COVID-19 = coronavirus disease 2019; ADL = activities of daily living; NTD = New Taiwan dollars; HBS = home-based services; CBS = community-based services; HCBS = home- and community-based service. Age, gender, education, marital status, monthly income, cognitive functioning, and ADL functioning were controlled.
*p ≤ .05, **p ≤ .01, ***p ≤ .001.
HCBS Use, COVID-19-Related Worries, or Social Disruptions and Depressive Symptoms: Month of Interview as a Moderator
| . | Depressive symptoms . | |||
|---|---|---|---|---|
| . | Model 1 . | Model 2 . | Model 3 . | Model 4 . |
| Predictor variables . | b (SE) . | b (SE) . | b (SE) . | b (SE) . |
| Age | −0.049 (0.035) | −0.031 (0.035) | −0.030 (0.035) | −0.028 (0.035) |
| Gender (ref. male) | 0.316 (0.583) | 0.117 (0.579) | 0.112 (0.580) | 0.073 (0.581) |
| Education (ref. no formal education) | ||||
| Elementary school | −0.894 (0.604) | −0.723 (0.596) | −0.720 (0.597) | −0.720 (0.597) |
| Junior high school or above | −1.620 (0.702)* | −1.392 (0.694)* | −1.400 (0.696)* | −1.422 (0.695)* |
| Marital status (ref. w/o a spouse) | −1.095 (0.583) | −1.343 (0.576)* | −1.338 (0.578)* | −1.325 (0.577)* |
| Monthly income (ref. less than NTD 5,999) | ||||
| 6,000–11,999 | 0.520 (0.644) | 0.704 (0.639) | 0.700 (0.644) | 0.689 (0.643) |
| 12,000–17,999 | 0.608 (0.802) | 0.538 (0.794) | 0.527 (0.797) | 0.560 (0.796) |
| 18,000 or above | 0.494 (0.854) | 0.515 (0.841) | 0.496 (0.848) | 0.534 (0.847) |
| Cognitive functioning | −0.293 (0.124)* | −0.390 (0.123)** | −0.390 (0.124)** | −0.376 (0.124)** |
| ADL functioning | −0.485 (0.070)*** | −0.508 (0.069)*** | −0.508 (0.069)*** | −0.509 (0.069)*** |
| Month of interview | −0.163 (0.300) | 0.092 (0.301) | 0.097 (0.303) | 0.087 (0.303) |
| HBS user (ref. no) | 2.320 (0.564)*** | 2.010 (0.565)*** | 2.006 (0.567)*** | 1.914 (0.569)*** |
| CBS user (ref. no) | 0.252 (0.543) | 0.276 (0.536) | 0.286 (0.539) | 0.288 (0.538) |
| COVID-19-related worries | 0.189 (0.069)** | 0.192(0.070)** | 0.158 (0.072)* | |
| COVID-19-related social disruptions | 0.074 (0.078) | 0.072 (0.079) | 0.113 (0.081) | |
| HBS user × Month of interview | 0.174 (0.621) | 0.243 (0.622) | ||
| CBS user × Month of interview | 0.026 (0.619) | −0.002 (0.619) | ||
| COVID-19-related worries × Month of interview | −0.129 (0.082) | |||
| COVID-19-related social disruptions × Month of interview | 0.192 (0.092)* | |||
| F (df) | 12.083 (13, 568)*** | 12.497 (15, 559)*** | 10.994 (17, 557)*** | 10.105 (19, 555)*** |
| R2 | 0.217 | 0.251 | 0.251 | 0.257 |
| . | Depressive symptoms . | |||
|---|---|---|---|---|
| . | Model 1 . | Model 2 . | Model 3 . | Model 4 . |
| Predictor variables . | b (SE) . | b (SE) . | b (SE) . | b (SE) . |
| Age | −0.049 (0.035) | −0.031 (0.035) | −0.030 (0.035) | −0.028 (0.035) |
| Gender (ref. male) | 0.316 (0.583) | 0.117 (0.579) | 0.112 (0.580) | 0.073 (0.581) |
| Education (ref. no formal education) | ||||
| Elementary school | −0.894 (0.604) | −0.723 (0.596) | −0.720 (0.597) | −0.720 (0.597) |
| Junior high school or above | −1.620 (0.702)* | −1.392 (0.694)* | −1.400 (0.696)* | −1.422 (0.695)* |
| Marital status (ref. w/o a spouse) | −1.095 (0.583) | −1.343 (0.576)* | −1.338 (0.578)* | −1.325 (0.577)* |
| Monthly income (ref. less than NTD 5,999) | ||||
| 6,000–11,999 | 0.520 (0.644) | 0.704 (0.639) | 0.700 (0.644) | 0.689 (0.643) |
| 12,000–17,999 | 0.608 (0.802) | 0.538 (0.794) | 0.527 (0.797) | 0.560 (0.796) |
| 18,000 or above | 0.494 (0.854) | 0.515 (0.841) | 0.496 (0.848) | 0.534 (0.847) |
| Cognitive functioning | −0.293 (0.124)* | −0.390 (0.123)** | −0.390 (0.124)** | −0.376 (0.124)** |
| ADL functioning | −0.485 (0.070)*** | −0.508 (0.069)*** | −0.508 (0.069)*** | −0.509 (0.069)*** |
| Month of interview | −0.163 (0.300) | 0.092 (0.301) | 0.097 (0.303) | 0.087 (0.303) |
| HBS user (ref. no) | 2.320 (0.564)*** | 2.010 (0.565)*** | 2.006 (0.567)*** | 1.914 (0.569)*** |
| CBS user (ref. no) | 0.252 (0.543) | 0.276 (0.536) | 0.286 (0.539) | 0.288 (0.538) |
| COVID-19-related worries | 0.189 (0.069)** | 0.192(0.070)** | 0.158 (0.072)* | |
| COVID-19-related social disruptions | 0.074 (0.078) | 0.072 (0.079) | 0.113 (0.081) | |
| HBS user × Month of interview | 0.174 (0.621) | 0.243 (0.622) | ||
| CBS user × Month of interview | 0.026 (0.619) | −0.002 (0.619) | ||
| COVID-19-related worries × Month of interview | −0.129 (0.082) | |||
| COVID-19-related social disruptions × Month of interview | 0.192 (0.092)* | |||
| F (df) | 12.083 (13, 568)*** | 12.497 (15, 559)*** | 10.994 (17, 557)*** | 10.105 (19, 555)*** |
| R2 | 0.217 | 0.251 | 0.251 | 0.257 |
Notes: COVID-19 = coronavirus disease 2019; ADL = activities of daily living; NTD = New Taiwan dollars; HBS = home-based services; CBS = community-based services; HCBS = home- and community-based service. Age, gender, education, marital status, monthly income, cognitive functioning, and ADL functioning were controlled.
*p ≤ .05, **p ≤ .01, ***p ≤ .001.
Discussion
This work is the first empirical study of how the depressive symptoms of community-dwelling older adults with disabilities, especially HCBS users, are affected by COVID-19-related worries or social disruptions and the intervening role of time on these associations. This research advances current knowledge by applying the SAVI model to elucidate how community-dwelling older persons with disabilities were affected by the pandemic and how the impact change over time, offering insights that may help to improve their well-being during the COVID-19 pandemic. The information that is contained herein is critical for policymakers and professionals who serve disabled older individuals in Taiwan and internationally, including many countries that are suffering from either a peak COVID-19 caseload or a resurgence.
With respect to demographic characteristics, the analytical results herein demonstrate that older age was associated with fewer COVID-19-related worries and social disruptions. These findings are broadly consistent with prior research, which has suggested that older adults can be better at regulating their emotional reactions and adopt more effective coping strategies when confronting major life stressors, including COVID-19-related stress and changes (Barber & Kim, 2020; Carney et al., 2020). Moreover, females and older individuals with lower income reported more COVID-19-related worries than males and those with higher income. This finding may reflect anxiety toward the scourge of COVID-19 that is rooted in their longstanding disadvantages in various circumstances, including limited financial, social, and health-related resources that facilitate adjustment to unexpected changes and self-sustenance through the epidemic (Barber & Kim, 2020; Brock et al., 2011). Among all personal factors, cognitive functioning appeared consistently predicts COVID-19-related worries and social disruptions across the models in Table 2. Disabled older adults with high cognitive functioning may be more able to gather information about COVID-19 and more active in making decisions in various life domains, so they are more aware of the threat of the virus and the interruptions that it causes (Maxfield & Pituch, 2020).
Interestingly, as given in Table 2, disabled older adults who were married consistently reported more COVID-19-related worries than their unmarried counterparts. A possible explanation for this unexpected finding is that policy efforts to control the spread of COVID-19, such as home quarantine, social distancing, and reduced community programming, may reduce the provision of both formal services and informal support to disabled older adults and their caregivers, leading to increased social isolation and accumulated caregiver burden (Dong, 2015; Zegwaard et al., 2011). Accordingly, COVID-19-related worries among married community-dwelling older individuals with disabilities might have arisen from an interplay among the unresolved burden on caregivers, the worsened well-being of care dyads, and the tense relationship between coresident spousal caregivers and care recipients with limited caregiving resources and activities.
Older adults who used HBS had significantly more COVID-19-related worries than non-HBS users, but the difference declined with the development of COVID-19, partially supporting the first research hypothesis. Differences between the levels of COVID-19-related worry of HBS users and nonusers were greatest in April, followed by May, and were smallest in June and July. Hence, the disparities in the manifestation of COVID-19-related worries between HBS users and nonusers may diminish after the outbreak stage. Specifically, HBS users were more worried about becoming infected, contracting COVID-19 will ruin their interpersonal relationships, anxious about the development of COVID-19, and concerned about the loss of control. A further investigation revealed that HBS users had lower ADL and self-rated health scores than non-HBS and CBS users. Thus, once infected, their underlying health conditions may increase their risk of severe illness. Also, HBS users will be forced to distance themselves physically and socially from their formal and informal caregivers, leaving them dependent with unmet care needs (Hoffman et al., 2020). The findings in this study support the use of the SAVI model to understand how the COVID-19-related worries of HBS users can vary with the time course of the pandemic. This study extends the SAVI model by considering the heterogeneity of community-dwelling disabled older adults to illuminate their emotional responses to COVID-19. In this population, HBS users tend to exhibit lower ADL, poor physical health, and greater dependence on formal services than non-HBS and CBS users. Thus, they appear to be more vulnerable to COVID-19-related worries, especially at the outbreak stage of the epidemic.
The month of interview was found to be a key factor in determining the relationship between COVID-19-related social disruptions and depressive symptoms, but the direction opposed that in the second research hypothesis. The results in this study demonstrate that the effects of COVID-19-related social disruptions on depressive symptoms depend on the phase of the pandemic. In the outbreak stage, COVID-19-related social disruptions appear to help disabled older persons to cope with the associated stress and to protect them from developing depressive symptoms. That is, a high level of perceived COVID-19-related social disruptions was weakly associated with fewer depressive symptoms in the outbreak stage of COVID-19. However, they can become risk factors for symptoms of depression after the outbreak stage of COVID-19. As the number of confirmed cases dropped and the number of domestic transmissions fell substantially, these health-protective behaviors and changes in daily routine became positively associated with depressive symptoms, and the positive association became even stronger as the loosening and controlled stage gave way to the reopening stage. The results confirm that the time course should be considered in examining the link between COVID-19-related social disruptions and depressive symptoms. This study contributes to the literature by establishing that COVID-19-related social disruptions exert distinct impacts on depressive symptoms. In this instance, the adoption of health-protective behaviors and changes in daily routine, such as avoiding going outdoors, stopping visiting relatives and friends, and refraining from using public transportation, may mitigate the symptoms of depression in the outbreak stage of the pandemic. However, maintaining strict health-protective behaviors, rigorously complying with pandemic-related restrictions, and not returning to “normal life” harmed the mental health of disabled older adults after the outbreak period of the pandemic. Most importantly, this detrimental effect increased over time.
The results of this study support the following recommendations for sustaining the well-being of community-dwelling older individuals with disabilities during the COVID-19 crisis. First, several sociodemographic conditions that are considered to be protective against stressors or can buffer the impact of stressors on the mental health of older adults, such as younger age, better cognitive and physical functioning, and having a spouse (Chao, 2012), appear to be associated with more COVID-19-related or social disruptions. Professionals who serve disabled older individuals should be aware of the lack of visibility of the corresponding subgroups and pay special attention to their undisclosed needs and emotional responses to COVID-19. Second, the needs and distinct vulnerability of community-dwelling older adults with disabilities have not received adequate attention. Based on the results of this study, HBS users are at the highest psychological risk from COVID-19 among the community-dwelling older population. Given the high level of COVID-19-related worries and the corresponding symptoms of depression of HBS users, more actions must be taken to meet their health and other basic needs, to maintain their daily routine, to ensure their access to regular programming, and to maintain their ability to undertake preferred activities (Choi & McDougall, 2007; Ebor et al., 2020; Miller, 2020). Most importantly, alternative service modes for informal caregivers that reduce their care burden and promote social connection and social participation of care dyads during the pandemic would also be helpful (Hoffman et al., 2020; Morrow-Howell et al., 2020). Third, worries that are caused by COVID-19 only manifest in the short term, supporting an optimistic outlook on the psychological impact of COVID-19. After the outbreak stage, the difference in degrees of COVID-19-related worries attenuated over time—especially true for community-dwelling older persons who use HBS. In other words, practitioners and clinics that serve seniors should monitor the psychological states of HBS users closely during the outbreak stage of the crisis. However, we expect COVID-19-related worries and associated symptoms of depression to diminish quickly once the pandemic is under control. Finally, the analytic results indicate that the relationship between COVID-19-related social disruptions and depressive symptoms can reverse. Therefore, COVID-19-related mandates must be assessed with reference to the development of the pandemic. Both the overloosening of controls in the upsurge stage and overrestrictive prohibitions in the loosening and controlling or reopening stage can be harmful to the psychological well-being of community-dwelling disabled older individuals.
Several limitations of this study should be acknowledged. First, given the single time period of data collection, no causal relationship can be established between the variables studied. For example, although we hypothesize that HBS users suffer from a high level of COVID-19-related worry, increasing symptoms of depression, COVID-19-related worries may also arise from depressive symptoms. Second, the generalizability of this study is limited by the sample characteristics because our data were obtained using a quota sampling method. Specifically, although the distribution of participants in each geographical stratum, municipality, county, and city was consistent with the population, the recruitment of respondents can only rely on referrals from local service providers and volunteers because the list of disabled community-dwelling older people in Taiwan is not available. Third, some characteristics of the participants, such as ADL functioning and percentages of HBS and CBS users, varied among the months of interview, future research may further benefit from the inclusion of dependent samples to reexamine the hypotheses and findings herein. Fourth, because research interviews were carried out from April to July 2020, further investigation over a longer period would be helpful to determine whether the relationships between variables that are identified in this study change in earlier or later phases of the COVID-19 pandemic.
Funding
The work was supported by the authors’ institution (No. G090095.
Conflict of Interest
None declared.
Acknowledgments
We would like to thank the editor and the three anonymous reviewers for their helpful suggestions and comments.