-
PDF
- Split View
-
Views
-
Cite
Cite
Deirdre MacManus, Roberto Rona, Hannah Dickson, Greta Somaini, Nicola Fear, Simon Wessely, Aggressive and Violent Behavior Among Military Personnel Deployed to Iraq and Afghanistan: Prevalence and Link With Deployment and Combat Exposure, Epidemiologic Reviews, Volume 37, Issue 1, 2015, Pages 196–212, https://doi.org/10.1093/epirev/mxu006
Close - Share Icon Share
Abstract
A systematic review and meta-analyses were conducted on studies of the prevalence of aggressive and violent behavior, as well as of violent offenses and convictions, among military personnel following deployment to Iraq and/or Afghanistan; the relationship with deployment and combat exposure; and the role that mental health problems, such as post-traumatic stress disorder (PTSD), have on the pathway between deployment and combat to violence. Seventeen studies published between January 1, 2001, and February 12, 2014, in the United States and the United Kingdom met the inclusion criteria. Despite methodological differences across studies, aggressive behavior was found to be prevalent among serving and formerly serving personnel, with pooled estimates of 10% (95% confidence interval (CI): 1, 20) for physical assault and 29% (95% CI: 25, 36) for all types of physical aggression in the last month, and worthy of further exploration. In both countries, rates were increased among combat-exposed, formerly serving personnel. The majority of studies suggested a small-to-moderate association between combat exposure and postdeployment physical aggression and violence, with a pooled estimate of the weighted odds ratio = 3.24 (95% CI: 2.75, 3.82), with several studies finding that violence increased with intensity and frequency of exposure to combat traumas. The review's findings support the mediating role of PTSD between combat and postdeployment violence and the importance of alcohol, especially if comorbid with PTSD.
INTRODUCTION
History tells us that concern about violent offenses among military personnel returned from deployment is not a new phenomenon. The idea that war veterans could be so brutalized by their experience of combat as to become predisposed toward violent behavior on return from deployment was proposed in the immediate aftermath of World War I (1). An outbreak of serious crime in the United Kingdom in 1919 was attributed to the return of “callous” and “battle-hardened” former servicemen. Crime statistics showing a rise in violent crime following the end of World War II reinforced the connection between combat veterans and violence in the minds of the public, press, and policy makers (2). However, the kind of epidemiologic longitudinal data necessary to establish any causal connection was largely not available at the time.
Fast forward to the last 10 years, when the United States, United Kingdom, and other coalition partners have been engaged in combat in 2 operational theaters, Iraq and Afghanistan. These conflicts have triggered renewed media, political, and public scrutiny of the impact of deployment on the physical and mental health of military personnel involved in these operations (3, 4). There have been media claims of increased rates of aggression and violent offenses postdeployment (5–8). Both the United States and the United Kingdom have published comprehensive government statistics on incarceration, and both report, perhaps to some people's surprise, that, overall, formerly serving personnel tend to be less likely than the general population to be in prison. However, in both the United States and the United Kingdom, they are overrepresented among those imprisoned for violent and sexual offences (9–14). However, incarcerations are only a small percentage of total convictions, and total convictions are likewise only a small percentage of all violent and/or antisocial behaviors. We must, therefore, look for empirical evidence to support or refute these claims that military personnel who have been deployed to Iraq and Afghanistan are at increased risk for not just incarceration for violent offenses but also for convictions for violence and engaging in aggressive and violent behavior.
There are multiple potential factors that may contribute to the relationship between combat and subsequent violence. It may be explained by preexisting tendencies to aggressive or risk-taking behavior such that, irrespective of experiences in the military or on deployment, an individual would have been on a trajectory toward violence. Military training and culture, as well as difficulty readjusting following exposure to threatening and violent operational environments, may also play important roles (15). Research evidence has accumulated suggesting adverse effects of deployment and combat during these conflicts on the mental health of military personnel (16–19), especially post-traumatic stress disorder (PTSD) (18, 20, 21) and alcohol misuse (22, 23). Another objective is therefore to look at the links between offending behaviors and such mental health problems in those who have returned from deployment.
What do we know from pre-Iraq and Afghanistan studies into postdeployment violence?
A substantial amount of research into violence among combat veterans has been carried out in the United States, much of which has utilized data from past conflicts, such as the Vietnam War or the 1991 Gulf War. The results have been mixed. A number of these studies found an association between combat exposure (rather than deployment) and physical aggression, intimate partner violence, and incarceration postdeployment (24–30). Other studies did not find that combat exposure predicted violence postdeployment (31), and some found premilitary characteristics to be the strongest risk factor for postdeployment violence (32, 33). Most studies from the pre-Iraq/Afghanistan eras proposed that PTSD was the most important mediator in the association between combat (trauma) and violent behavior (34–37). Angry reactions and irritability have long been recognized features of PTSD so much so that the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-V), now explicitly includes “irritable behavior and angry outbursts” as well as “reckless or self-destructive behavior,” thus formally acknowledging the evidence for the link between PTSD and aggression (38). Other psychopathologies can, however, also be linked with postdeployment violence, in particular alcohol misuse (39, 40).
Weaknesses in past research
A major problem inherent in many of these pre-Iraq/Afghanistan era studies is that they were carried out many years after the deployment in question and, given that they often used self-report measures, this delay increased the potential for recall bias regarding deployment experiences and the violence outcome. The association with deployment becomes increasingly blurred over time, and the reporting of past experiences can be affected by more recent influences, such as current health status. Additionally, it should not be assumed that previous conflicts provide a blueprint for the recent conflicts (41). Each conflict has its own particular characteristics and, hence, consequences. Different enlistment methods (the US military during the Vietnam War was a mixture of a conscript and volunteer force; now it is all volunteer, as in the United Kingdom) would suggest that different military cohorts are not comparable with respect to predeployment and sociodemographic characteristics, possibly leading to variations in postdeployment adjustment problems (42).
Terminology
Research in this area has explored a range of interrelated outcomes of “violence” and “aggression” and related phenomena. Some studies ask about concerns about aggressive or violent behavior, and others focus on actual aggressive behavior, although that ranges from verbal and property aggression to threats of violence and actual physical violence. The term “violence” has been used to refer to anything from hitting and slapping to use of a weapon, grievous bodily harm, and homicide. Some studies distinguish between the levels of severity and others do not. Violence may be further divided into general interpersonal violence or violence toward a family member or partner (intimate partner violence). Finally, more recent studies have looked at criminal convictions and incarceration for violence as objective outcome measures. The outcome measurement period also varies from study to study. We must be aware of these differences when trying to compare or to contrast the findings from different studies.
Aims and objectives
This paper aims to systematically review studies of the prevalence of aggressive and violent behavior, as well as of violent offenses and convictions, among military personnel following deployment to Iraq and Afghanistan; its relationship with deployment and combat exposure; and the role that postdeployment mental health problems, such as PTSD, have on the pathway between deployment and combat to violence.
METHODS
We used MEDLINE, PsycINFO, Web of Science, and Embase to search peer-reviewed journals (from January 1, 2001, to February 12, 2014) for articles describing the prevalence of or empirical relationships between risk factors and postdeployment violence among military populations. Boolean operators (e.g., AND, OR) and wildcard symbols (e.g., *) were used in the following key search terms: violen*, aggressi*, conviction, arrest, incarceration, intimate partner violence, domestic violence, spousal abuse OR antisocial AND veteran, military, army, armed forces, navy, marine*, air force, soldier, reserve* OR national guard AND combat, deploy*, conflict, war OR operation. We also utilized references from articles to identify studies. Review articles were also used to identify literature. Duplicate papers were removed, and the reference lists of all eligible studies were checked for additional studies (refer to Figure 1 for detailed results of the search strategy).
Flow diagram illustrating the retrieval, selection, and exclusion of articles.
Included were quantitative studies that 1) operationalized violence and/or aggression as actual physical harm caused by one person against another, a range of aggressive behaviors (property and physical aggression and threat of violence), offending behavior classified as violent, or incarceration for the latter and 2) explored such behaviors among serving or formerly serving military personnel who had been in Iraq or Afghanistan post-2001. Excluded from the current review were book chapters, dissertations, case studies, papers published before 2001, qualitative or nonempirical studies, intervention studies, studies reporting a sample size less than 100, and articles not in English. Studies concerning conflicts other than Iraq and Afghanistan post-2001, such as Vietnam, the first Gulf War, or the interventions in the former Yugoslavia were not considered.
This process yielded 17 papers that specifically described the prevalence of aggressive or violent behavior and/or statistical relationships between aggressive or violent behavior and risk factors (Figure 1). Data extraction was conducted by one researcher (D. M.) and checked by a second data reviewer (G. S.). The data collected from each study included study location, study design, number of service members evaluated, main variables of interest (deployment, combat role, specific combat exposure, PTSD or other postdeployment mental health or behavior problem), outcome measure of aggression or violence, and measures of effect (Table 1).
Summary of Methodology and Results From Studies Published Between January 1, 2001, and February 12, 2014, in the United States and United Kingdom
| First Author, Year (Reference No.) . | Study Population . | Exposures . | Types of Violence and Timing . | Findings . | |||
|---|---|---|---|---|---|---|---|
| Sample Size, No. . | Location . | Data Type . | Population . | ||||
| Longitudinal studies | |||||||
| Elbogen, 2014 (59)a | 1,388 | United States | Postal survey | National sample from Department of Veteran Affairs | Combat exposure, violence prior to military service, PTSD, and alcohol misuse | “Severe violence” or “other physical aggression” in past year | 9% severe violence; 26% other physical aggression in last year. Severe violence/aggression associated with violence prior to military (OR = 3.95, 95% CI: 2.05, 7.62, P = 0.0001; OR = 2.51, 95% CI: 1.44, 4.37, P = 0.0011); combat exposure (OR = 1.03, 95% CI: 1.01, 1.05, P = 0.0066; OR = 1.04, 95% CI: 1.02, 1.05, P = 0.0001); and comorbid diagnosis of PTSD and alcohol use (OR = 4.09, 95% CI: 1.91, 8.77, P = 0.0003; OR = 3.45, 95% CI: 1.83, 6.50, P = 0.0001). |
| Sullivan, 2014 (64)a | 1,388 | United States | Postal survey | National sample from Department of Veteran Affairs | Combat exposure, history of violence prior to military service, PTSD, and alcohol misuse | “Severe violence” or “other physical aggression” toward family or toward stranger in past year | Family-directed acts in last year: 12.8% other physical aggression and 3.1% severe violence. Stranger directed acts: 9.5% aggression and 4.8% severe violence. High combat associated with severe family violence (OR = 3.96, 95% CI: 1.30, 12.02, P = 0.0153), stranger aggression (OR = 2.47, 95% CI: 1.39, 4.37, P = 0.002), and severe stranger violence (OR = 2.58, 95% CI: 1.14, 5.85, P = 0.0234). |
| MacManus, 2013 (60)b | 13,856 | United Kingdom | Questionnaire survey | United Kingdom military population | Self-reported deployment, role on deployment, combat exposures, postdeployment mental health (PTSD, alcohol misuse, aggressive behavior) | Offending records from United Kingdom Ministry of Justice Police National Computer database | 11% lifetime record of violent offense and 7% violent offenses postdeployment. Preservice violent offending strongest predictor of violent offending (aOR = 1.79, 95% CI: 1.34, 2.39, P < 0.0001). Deployment not associated with violent offending. Combat role associated with violent offending (aHR = 1.53, 95% CI: 1.15, 2.03; P = 0.003). Increased exposure to traumatic events during deployment associated with risk of violent offending (aHR = 1.65, 95% CI: 1.12, 2.40, P = 0.01; test for trend, P = 0.032). |
| Killgore, 2008 (56) | 1,252 | Questionnaire survey | US Army members returned from active duty | Combat experiences | Risk-taking propensity and aggressive behaviors in the last month | 2.2% got into a fight and hit a person, and 27% reported physical aggression. Violent combat exposure a predictor of risk-taking propensity (r = 0.30, F = 23.71, P < 0.001). No. of combat exposures correlated with verbal aggression and threats of violence. Killing the enemy and killing of nonhostiles were correlated with actual physical aggression toward others (r = 0.06, P < 0.05; r = 0.11, P < 0.0005, respectively). | |
| Wright, 2012 (57) | 1,397 | United States | Questionnaire survey | US Cavalry regiment | Combat exposure and internalizing symptoms (depression and anxiety) | Aggressive behavior in past month | 67.3% endorsed aggressive behavior. Combat exposure had small direct association with externalizing behaviors at follow-up (standardized path estimate = 0.14, P < 0.007) after accounting for internalizing symptoms and social environment. |
| Rabenhorst, 2012 (63) | 4,874 couples (6,063 individuals) | United States | Military records | National US military sample | Deployment | Rates of spousal abuse according to pre- and postdeployment official military records | Among abusive couples, the overall spousal abuse rate was 12.6% lower postdeployment. In couples where only one spouse abused and alcohol was involved, the abuse rate was significantly higher postdeployment. In couples where only the husband abused, the moderate or severe abuse rate was 24.0% higher postdeployment (RR = 1.24, 95% CI: 1.084, 1.444, P < 0.001), and when alcohol was used the abuse rate was 36.8% higher postdeployment (RR = 1.368, 95% CI: 1.055, 1.775, P < 0.05). |
| Schmaling, 2011 (65) | 546 | United States | Questionnaire survey | Nonrandom married or cohabiting personnel deployed to OIF | Rank, duty status, years in the service, previous deployments, and area of the most recent deployment | IPV and relationship dissolution in past year | At demobilization, 13.5% of participants reported IPV in the prior year. Deployment was not associated with IPV. |
| Cross-sectional studies | |||||||
| MacManus, 2012 (54)b | 10,272 | United Kingdom | Questionnaire survey | Random United Kingdom military population sample | Role on deployment, combat exposures, postdeployment mental health (PTSD, symptoms of common mental disorder, alcohol misuse) | Aggressive behavior in the weeks following homecoming | 12.6% were physically violent to either a member of their family and/or someone outside of their family. Violence associated with combat role (aOR = 2.0, 95% CI: 1.6, 2.5) and increased exposure to traumatic events (aOR for ≥4 traumatic events = 3.7, 95% CI: 2.5, 5.5). |
| Tsai, 2013 (61) | 30,968 | United States | Record based | US Department of Veteran Affairs records | Service in OEF/OIF/OND, combat exposure, and records of mental health diagnoses | Percentage of OEF/OIF/OND veterans incarcerated and incarcerated for a violent offense. Risk of incarceration among OEF/OIF/OND veterans compared with veterans of other eras and risk of incarceration for a violent offense | OEF/OIF/OND veterans less than half as likely as other veterans to be incarcerated and constituted only 3.9% of the incarcerated veterans; 37.5% of OEF/OIF/OND incarcerated veterans committed violent offense. The prevalence of violent offenders was similar among veterans of all eras. OEF/OIF/OND veterans were more likely to report combat exposure and were 3 times more likely to have combat-related PTSD. |
| Booth-Kewley, 2010 (49) | 1,543 | United States | Questionnaire survey | US Marines combat units | Combat exposure score, PTSD symptoms, and deployment-related stressors | ASB scale in past year | 22.9% scored high on ASB scale. The intensity of combat exposure was positively associated with ASB (very high combat: aOR = 1.81, 95% CI: 1.20, 2.73, P < 0.001). |
| Elbogen, 2012 (53)a | 1,388 | United States | Postal survey | National sample from Department of Veteran Affairs | Combat exposure, PTSD, and alcohol misuse | Severe violence or other physical aggression in past year | 33% committed ≥1 act of noncombat-related violence/aggression, and 11% committed ≥1 act of severe noncombat-related violence. Severe violence associated with combat exposure (aOR = 3.0, 95% CI: 1.85, 3.46, P < 0.001), alcohol misuse (aOR = 2.0, 95% CI: 1.28, 3.11, P = 0.0023), previous criminal arrests (aOR = 1.70, 95% CI: 1.07, 2.71, P = 0.0259), PTSD (aOR = 1.93, 95% CI: 1.21, 3.07, P = 0.0054), and homelessness (OR = 2.05, 95% CI: 1.0, 4.19, P = 0.0488). |
| Gallaway, 2012 (50)c | 6,128 | United States | Questionnaire survey | US Army combat units | Combat exposure in previous deployment, PTSD, depression, and alcohol misuse | Major and minor physical aggression in last year | 8% physical altercation with someone, 22% punching or hitting someone, 39% pushing or shoving someone, 4% using a knife or gun on someone. Minor aggression was associated with lifetime history of physical altercations with significant other (exp(β)d = 2.6, SE, 0.2, P < 0.01) and high combat intensity (exp(β) = 1.6, SE, 0.1, P < 0.01). Severe physical aggression was associated with lifetime history of physical altercations with significant other (exp(β) = 2.5, SE, 0.1, P < 0.01) and high combat intensity (exp(β) =1.5, SE, 0.1, P < 0.01). |
| Gallaway, 2013 (52)c | 6,002 | United States | Questionnaire survey | US Army combat units | Combat exposure, PTSD, depression, alcohol misuse, and self-reported criminal history (conviction) since joining military | Major and minor physical aggression in last year | 25.8% minor aggression, 21.0% major aggression, and 8% having a physical altercation with a significant other in the last year. Intensity of combat exposure was associated with severe aggression (aOR = 2.93, 95% CI: 2.4, 3.6), minor aggression (aOR = 3.52, 95% CI: 2.9, 4.3), reporting a physical altercation with a significant other (OR = 1.78, 95% CI: 1.3, 1.6), and a criminal conviction since joining the army (OR = 2.69, 95% CI: 1.8, 4.0). |
| Hellmuth, 2012 (48) | 653 | United States | Clinical assessment questionnaire | Clinical sample from Department of Veteran Affairs clinic | Trait anger, PTSD symptoms, and alcohol misuse | Aggression in the last 4 months | 31.8% with at least one act of physically aggressive behavior in the past 4 months, 27.7% with less severe physical aggression (i.e., threatening without a weapon), and 18.9% with more severe physical aggression (i.e., physical fight and threatening with a weapon). |
| Sayers, 2009 (62) | 199 | United States | Clinical assessment questionnaire | Clinical sample from Department of Veteran Affairs clinic | Combat exposure, PTSD, and alcohol misuse screening | Family reintegration problems, including self-reported domestic aggression in the past year | Over 75% of married or cohabiting veterans reported some type of family problem in the past week; 53.7% of veterans with current or recently separated partners reported conflicts involving shouting, pushing, or shoving. |
| Other study types | |||||||
| Jakupcak, 2007 (66) | 117 | United States | Clinical assessment questionnaire | Clinical series sample | Combat exposure and PTSD | Aggression (time period not specified) | 53.2% in PTSD group and subthreshold PTSD group endorsed at least one act of aggression compared with 20.4% in non-PTSD group. Combat exposure was positively associated with trait anger and hostility but not with aggression. Veterans who screened positive for PTSD reported greater recent aggression than did veterans who screened negative for PTSD (exp(β) = 4.17, 95% CI: 1.6, 10.7, P < 0.001) (after controlling for age and problem drinking). |
| Thomas, 2010 (19) | 13,226 | United States | Questionnaire survey | US combat brigade team | N/A | Aggressive behavior in the past month | Prevalence of aggression stable between 3 months and 12 months postdeployment: 35%–43% of soldiers threatened someone with physical violence or got angry enough with someone to kick, smash, or punch something, and 18% had gotten into a fight with someone and hit the person. |
| First Author, Year (Reference No.) . | Study Population . | Exposures . | Types of Violence and Timing . | Findings . | |||
|---|---|---|---|---|---|---|---|
| Sample Size, No. . | Location . | Data Type . | Population . | ||||
| Longitudinal studies | |||||||
| Elbogen, 2014 (59)a | 1,388 | United States | Postal survey | National sample from Department of Veteran Affairs | Combat exposure, violence prior to military service, PTSD, and alcohol misuse | “Severe violence” or “other physical aggression” in past year | 9% severe violence; 26% other physical aggression in last year. Severe violence/aggression associated with violence prior to military (OR = 3.95, 95% CI: 2.05, 7.62, P = 0.0001; OR = 2.51, 95% CI: 1.44, 4.37, P = 0.0011); combat exposure (OR = 1.03, 95% CI: 1.01, 1.05, P = 0.0066; OR = 1.04, 95% CI: 1.02, 1.05, P = 0.0001); and comorbid diagnosis of PTSD and alcohol use (OR = 4.09, 95% CI: 1.91, 8.77, P = 0.0003; OR = 3.45, 95% CI: 1.83, 6.50, P = 0.0001). |
| Sullivan, 2014 (64)a | 1,388 | United States | Postal survey | National sample from Department of Veteran Affairs | Combat exposure, history of violence prior to military service, PTSD, and alcohol misuse | “Severe violence” or “other physical aggression” toward family or toward stranger in past year | Family-directed acts in last year: 12.8% other physical aggression and 3.1% severe violence. Stranger directed acts: 9.5% aggression and 4.8% severe violence. High combat associated with severe family violence (OR = 3.96, 95% CI: 1.30, 12.02, P = 0.0153), stranger aggression (OR = 2.47, 95% CI: 1.39, 4.37, P = 0.002), and severe stranger violence (OR = 2.58, 95% CI: 1.14, 5.85, P = 0.0234). |
| MacManus, 2013 (60)b | 13,856 | United Kingdom | Questionnaire survey | United Kingdom military population | Self-reported deployment, role on deployment, combat exposures, postdeployment mental health (PTSD, alcohol misuse, aggressive behavior) | Offending records from United Kingdom Ministry of Justice Police National Computer database | 11% lifetime record of violent offense and 7% violent offenses postdeployment. Preservice violent offending strongest predictor of violent offending (aOR = 1.79, 95% CI: 1.34, 2.39, P < 0.0001). Deployment not associated with violent offending. Combat role associated with violent offending (aHR = 1.53, 95% CI: 1.15, 2.03; P = 0.003). Increased exposure to traumatic events during deployment associated with risk of violent offending (aHR = 1.65, 95% CI: 1.12, 2.40, P = 0.01; test for trend, P = 0.032). |
| Killgore, 2008 (56) | 1,252 | Questionnaire survey | US Army members returned from active duty | Combat experiences | Risk-taking propensity and aggressive behaviors in the last month | 2.2% got into a fight and hit a person, and 27% reported physical aggression. Violent combat exposure a predictor of risk-taking propensity (r = 0.30, F = 23.71, P < 0.001). No. of combat exposures correlated with verbal aggression and threats of violence. Killing the enemy and killing of nonhostiles were correlated with actual physical aggression toward others (r = 0.06, P < 0.05; r = 0.11, P < 0.0005, respectively). | |
| Wright, 2012 (57) | 1,397 | United States | Questionnaire survey | US Cavalry regiment | Combat exposure and internalizing symptoms (depression and anxiety) | Aggressive behavior in past month | 67.3% endorsed aggressive behavior. Combat exposure had small direct association with externalizing behaviors at follow-up (standardized path estimate = 0.14, P < 0.007) after accounting for internalizing symptoms and social environment. |
| Rabenhorst, 2012 (63) | 4,874 couples (6,063 individuals) | United States | Military records | National US military sample | Deployment | Rates of spousal abuse according to pre- and postdeployment official military records | Among abusive couples, the overall spousal abuse rate was 12.6% lower postdeployment. In couples where only one spouse abused and alcohol was involved, the abuse rate was significantly higher postdeployment. In couples where only the husband abused, the moderate or severe abuse rate was 24.0% higher postdeployment (RR = 1.24, 95% CI: 1.084, 1.444, P < 0.001), and when alcohol was used the abuse rate was 36.8% higher postdeployment (RR = 1.368, 95% CI: 1.055, 1.775, P < 0.05). |
| Schmaling, 2011 (65) | 546 | United States | Questionnaire survey | Nonrandom married or cohabiting personnel deployed to OIF | Rank, duty status, years in the service, previous deployments, and area of the most recent deployment | IPV and relationship dissolution in past year | At demobilization, 13.5% of participants reported IPV in the prior year. Deployment was not associated with IPV. |
| Cross-sectional studies | |||||||
| MacManus, 2012 (54)b | 10,272 | United Kingdom | Questionnaire survey | Random United Kingdom military population sample | Role on deployment, combat exposures, postdeployment mental health (PTSD, symptoms of common mental disorder, alcohol misuse) | Aggressive behavior in the weeks following homecoming | 12.6% were physically violent to either a member of their family and/or someone outside of their family. Violence associated with combat role (aOR = 2.0, 95% CI: 1.6, 2.5) and increased exposure to traumatic events (aOR for ≥4 traumatic events = 3.7, 95% CI: 2.5, 5.5). |
| Tsai, 2013 (61) | 30,968 | United States | Record based | US Department of Veteran Affairs records | Service in OEF/OIF/OND, combat exposure, and records of mental health diagnoses | Percentage of OEF/OIF/OND veterans incarcerated and incarcerated for a violent offense. Risk of incarceration among OEF/OIF/OND veterans compared with veterans of other eras and risk of incarceration for a violent offense | OEF/OIF/OND veterans less than half as likely as other veterans to be incarcerated and constituted only 3.9% of the incarcerated veterans; 37.5% of OEF/OIF/OND incarcerated veterans committed violent offense. The prevalence of violent offenders was similar among veterans of all eras. OEF/OIF/OND veterans were more likely to report combat exposure and were 3 times more likely to have combat-related PTSD. |
| Booth-Kewley, 2010 (49) | 1,543 | United States | Questionnaire survey | US Marines combat units | Combat exposure score, PTSD symptoms, and deployment-related stressors | ASB scale in past year | 22.9% scored high on ASB scale. The intensity of combat exposure was positively associated with ASB (very high combat: aOR = 1.81, 95% CI: 1.20, 2.73, P < 0.001). |
| Elbogen, 2012 (53)a | 1,388 | United States | Postal survey | National sample from Department of Veteran Affairs | Combat exposure, PTSD, and alcohol misuse | Severe violence or other physical aggression in past year | 33% committed ≥1 act of noncombat-related violence/aggression, and 11% committed ≥1 act of severe noncombat-related violence. Severe violence associated with combat exposure (aOR = 3.0, 95% CI: 1.85, 3.46, P < 0.001), alcohol misuse (aOR = 2.0, 95% CI: 1.28, 3.11, P = 0.0023), previous criminal arrests (aOR = 1.70, 95% CI: 1.07, 2.71, P = 0.0259), PTSD (aOR = 1.93, 95% CI: 1.21, 3.07, P = 0.0054), and homelessness (OR = 2.05, 95% CI: 1.0, 4.19, P = 0.0488). |
| Gallaway, 2012 (50)c | 6,128 | United States | Questionnaire survey | US Army combat units | Combat exposure in previous deployment, PTSD, depression, and alcohol misuse | Major and minor physical aggression in last year | 8% physical altercation with someone, 22% punching or hitting someone, 39% pushing or shoving someone, 4% using a knife or gun on someone. Minor aggression was associated with lifetime history of physical altercations with significant other (exp(β)d = 2.6, SE, 0.2, P < 0.01) and high combat intensity (exp(β) = 1.6, SE, 0.1, P < 0.01). Severe physical aggression was associated with lifetime history of physical altercations with significant other (exp(β) = 2.5, SE, 0.1, P < 0.01) and high combat intensity (exp(β) =1.5, SE, 0.1, P < 0.01). |
| Gallaway, 2013 (52)c | 6,002 | United States | Questionnaire survey | US Army combat units | Combat exposure, PTSD, depression, alcohol misuse, and self-reported criminal history (conviction) since joining military | Major and minor physical aggression in last year | 25.8% minor aggression, 21.0% major aggression, and 8% having a physical altercation with a significant other in the last year. Intensity of combat exposure was associated with severe aggression (aOR = 2.93, 95% CI: 2.4, 3.6), minor aggression (aOR = 3.52, 95% CI: 2.9, 4.3), reporting a physical altercation with a significant other (OR = 1.78, 95% CI: 1.3, 1.6), and a criminal conviction since joining the army (OR = 2.69, 95% CI: 1.8, 4.0). |
| Hellmuth, 2012 (48) | 653 | United States | Clinical assessment questionnaire | Clinical sample from Department of Veteran Affairs clinic | Trait anger, PTSD symptoms, and alcohol misuse | Aggression in the last 4 months | 31.8% with at least one act of physically aggressive behavior in the past 4 months, 27.7% with less severe physical aggression (i.e., threatening without a weapon), and 18.9% with more severe physical aggression (i.e., physical fight and threatening with a weapon). |
| Sayers, 2009 (62) | 199 | United States | Clinical assessment questionnaire | Clinical sample from Department of Veteran Affairs clinic | Combat exposure, PTSD, and alcohol misuse screening | Family reintegration problems, including self-reported domestic aggression in the past year | Over 75% of married or cohabiting veterans reported some type of family problem in the past week; 53.7% of veterans with current or recently separated partners reported conflicts involving shouting, pushing, or shoving. |
| Other study types | |||||||
| Jakupcak, 2007 (66) | 117 | United States | Clinical assessment questionnaire | Clinical series sample | Combat exposure and PTSD | Aggression (time period not specified) | 53.2% in PTSD group and subthreshold PTSD group endorsed at least one act of aggression compared with 20.4% in non-PTSD group. Combat exposure was positively associated with trait anger and hostility but not with aggression. Veterans who screened positive for PTSD reported greater recent aggression than did veterans who screened negative for PTSD (exp(β) = 4.17, 95% CI: 1.6, 10.7, P < 0.001) (after controlling for age and problem drinking). |
| Thomas, 2010 (19) | 13,226 | United States | Questionnaire survey | US combat brigade team | N/A | Aggressive behavior in the past month | Prevalence of aggression stable between 3 months and 12 months postdeployment: 35%–43% of soldiers threatened someone with physical violence or got angry enough with someone to kick, smash, or punch something, and 18% had gotten into a fight with someone and hit the person. |
Abbreviations: aOR, adjusted odds ratio; aHR, adjusted hazards ratio; ASB, antisocial behavior; CI, confidence interval; IPV, intimate partner violence; N/A, not applicable; OEF, Operation Enduring Freedom; OIF, Operation Iraqi Freedom; OND, Operation New Dawn; OR, odds ratio; PTSD, post-traumatic stress syndrome; RR, rate ratio; SE, standard error.
a Elbogen, 2012 (53),Elbogen, 2014 (59), and Sullivan, 2014 (64) are based on the same study sample.
b McManus, 2012 (54) and MacManus, 2013 (60) are based on the same study sample.
c Gallaway, 2012 (50) and Gallaway, 2013 (52) are based on the same study sample.
d Exponentiation of the β coefficient, which is an odds ratio.
Summary of Methodology and Results From Studies Published Between January 1, 2001, and February 12, 2014, in the United States and United Kingdom
| First Author, Year (Reference No.) . | Study Population . | Exposures . | Types of Violence and Timing . | Findings . | |||
|---|---|---|---|---|---|---|---|
| Sample Size, No. . | Location . | Data Type . | Population . | ||||
| Longitudinal studies | |||||||
| Elbogen, 2014 (59)a | 1,388 | United States | Postal survey | National sample from Department of Veteran Affairs | Combat exposure, violence prior to military service, PTSD, and alcohol misuse | “Severe violence” or “other physical aggression” in past year | 9% severe violence; 26% other physical aggression in last year. Severe violence/aggression associated with violence prior to military (OR = 3.95, 95% CI: 2.05, 7.62, P = 0.0001; OR = 2.51, 95% CI: 1.44, 4.37, P = 0.0011); combat exposure (OR = 1.03, 95% CI: 1.01, 1.05, P = 0.0066; OR = 1.04, 95% CI: 1.02, 1.05, P = 0.0001); and comorbid diagnosis of PTSD and alcohol use (OR = 4.09, 95% CI: 1.91, 8.77, P = 0.0003; OR = 3.45, 95% CI: 1.83, 6.50, P = 0.0001). |
| Sullivan, 2014 (64)a | 1,388 | United States | Postal survey | National sample from Department of Veteran Affairs | Combat exposure, history of violence prior to military service, PTSD, and alcohol misuse | “Severe violence” or “other physical aggression” toward family or toward stranger in past year | Family-directed acts in last year: 12.8% other physical aggression and 3.1% severe violence. Stranger directed acts: 9.5% aggression and 4.8% severe violence. High combat associated with severe family violence (OR = 3.96, 95% CI: 1.30, 12.02, P = 0.0153), stranger aggression (OR = 2.47, 95% CI: 1.39, 4.37, P = 0.002), and severe stranger violence (OR = 2.58, 95% CI: 1.14, 5.85, P = 0.0234). |
| MacManus, 2013 (60)b | 13,856 | United Kingdom | Questionnaire survey | United Kingdom military population | Self-reported deployment, role on deployment, combat exposures, postdeployment mental health (PTSD, alcohol misuse, aggressive behavior) | Offending records from United Kingdom Ministry of Justice Police National Computer database | 11% lifetime record of violent offense and 7% violent offenses postdeployment. Preservice violent offending strongest predictor of violent offending (aOR = 1.79, 95% CI: 1.34, 2.39, P < 0.0001). Deployment not associated with violent offending. Combat role associated with violent offending (aHR = 1.53, 95% CI: 1.15, 2.03; P = 0.003). Increased exposure to traumatic events during deployment associated with risk of violent offending (aHR = 1.65, 95% CI: 1.12, 2.40, P = 0.01; test for trend, P = 0.032). |
| Killgore, 2008 (56) | 1,252 | Questionnaire survey | US Army members returned from active duty | Combat experiences | Risk-taking propensity and aggressive behaviors in the last month | 2.2% got into a fight and hit a person, and 27% reported physical aggression. Violent combat exposure a predictor of risk-taking propensity (r = 0.30, F = 23.71, P < 0.001). No. of combat exposures correlated with verbal aggression and threats of violence. Killing the enemy and killing of nonhostiles were correlated with actual physical aggression toward others (r = 0.06, P < 0.05; r = 0.11, P < 0.0005, respectively). | |
| Wright, 2012 (57) | 1,397 | United States | Questionnaire survey | US Cavalry regiment | Combat exposure and internalizing symptoms (depression and anxiety) | Aggressive behavior in past month | 67.3% endorsed aggressive behavior. Combat exposure had small direct association with externalizing behaviors at follow-up (standardized path estimate = 0.14, P < 0.007) after accounting for internalizing symptoms and social environment. |
| Rabenhorst, 2012 (63) | 4,874 couples (6,063 individuals) | United States | Military records | National US military sample | Deployment | Rates of spousal abuse according to pre- and postdeployment official military records | Among abusive couples, the overall spousal abuse rate was 12.6% lower postdeployment. In couples where only one spouse abused and alcohol was involved, the abuse rate was significantly higher postdeployment. In couples where only the husband abused, the moderate or severe abuse rate was 24.0% higher postdeployment (RR = 1.24, 95% CI: 1.084, 1.444, P < 0.001), and when alcohol was used the abuse rate was 36.8% higher postdeployment (RR = 1.368, 95% CI: 1.055, 1.775, P < 0.05). |
| Schmaling, 2011 (65) | 546 | United States | Questionnaire survey | Nonrandom married or cohabiting personnel deployed to OIF | Rank, duty status, years in the service, previous deployments, and area of the most recent deployment | IPV and relationship dissolution in past year | At demobilization, 13.5% of participants reported IPV in the prior year. Deployment was not associated with IPV. |
| Cross-sectional studies | |||||||
| MacManus, 2012 (54)b | 10,272 | United Kingdom | Questionnaire survey | Random United Kingdom military population sample | Role on deployment, combat exposures, postdeployment mental health (PTSD, symptoms of common mental disorder, alcohol misuse) | Aggressive behavior in the weeks following homecoming | 12.6% were physically violent to either a member of their family and/or someone outside of their family. Violence associated with combat role (aOR = 2.0, 95% CI: 1.6, 2.5) and increased exposure to traumatic events (aOR for ≥4 traumatic events = 3.7, 95% CI: 2.5, 5.5). |
| Tsai, 2013 (61) | 30,968 | United States | Record based | US Department of Veteran Affairs records | Service in OEF/OIF/OND, combat exposure, and records of mental health diagnoses | Percentage of OEF/OIF/OND veterans incarcerated and incarcerated for a violent offense. Risk of incarceration among OEF/OIF/OND veterans compared with veterans of other eras and risk of incarceration for a violent offense | OEF/OIF/OND veterans less than half as likely as other veterans to be incarcerated and constituted only 3.9% of the incarcerated veterans; 37.5% of OEF/OIF/OND incarcerated veterans committed violent offense. The prevalence of violent offenders was similar among veterans of all eras. OEF/OIF/OND veterans were more likely to report combat exposure and were 3 times more likely to have combat-related PTSD. |
| Booth-Kewley, 2010 (49) | 1,543 | United States | Questionnaire survey | US Marines combat units | Combat exposure score, PTSD symptoms, and deployment-related stressors | ASB scale in past year | 22.9% scored high on ASB scale. The intensity of combat exposure was positively associated with ASB (very high combat: aOR = 1.81, 95% CI: 1.20, 2.73, P < 0.001). |
| Elbogen, 2012 (53)a | 1,388 | United States | Postal survey | National sample from Department of Veteran Affairs | Combat exposure, PTSD, and alcohol misuse | Severe violence or other physical aggression in past year | 33% committed ≥1 act of noncombat-related violence/aggression, and 11% committed ≥1 act of severe noncombat-related violence. Severe violence associated with combat exposure (aOR = 3.0, 95% CI: 1.85, 3.46, P < 0.001), alcohol misuse (aOR = 2.0, 95% CI: 1.28, 3.11, P = 0.0023), previous criminal arrests (aOR = 1.70, 95% CI: 1.07, 2.71, P = 0.0259), PTSD (aOR = 1.93, 95% CI: 1.21, 3.07, P = 0.0054), and homelessness (OR = 2.05, 95% CI: 1.0, 4.19, P = 0.0488). |
| Gallaway, 2012 (50)c | 6,128 | United States | Questionnaire survey | US Army combat units | Combat exposure in previous deployment, PTSD, depression, and alcohol misuse | Major and minor physical aggression in last year | 8% physical altercation with someone, 22% punching or hitting someone, 39% pushing or shoving someone, 4% using a knife or gun on someone. Minor aggression was associated with lifetime history of physical altercations with significant other (exp(β)d = 2.6, SE, 0.2, P < 0.01) and high combat intensity (exp(β) = 1.6, SE, 0.1, P < 0.01). Severe physical aggression was associated with lifetime history of physical altercations with significant other (exp(β) = 2.5, SE, 0.1, P < 0.01) and high combat intensity (exp(β) =1.5, SE, 0.1, P < 0.01). |
| Gallaway, 2013 (52)c | 6,002 | United States | Questionnaire survey | US Army combat units | Combat exposure, PTSD, depression, alcohol misuse, and self-reported criminal history (conviction) since joining military | Major and minor physical aggression in last year | 25.8% minor aggression, 21.0% major aggression, and 8% having a physical altercation with a significant other in the last year. Intensity of combat exposure was associated with severe aggression (aOR = 2.93, 95% CI: 2.4, 3.6), minor aggression (aOR = 3.52, 95% CI: 2.9, 4.3), reporting a physical altercation with a significant other (OR = 1.78, 95% CI: 1.3, 1.6), and a criminal conviction since joining the army (OR = 2.69, 95% CI: 1.8, 4.0). |
| Hellmuth, 2012 (48) | 653 | United States | Clinical assessment questionnaire | Clinical sample from Department of Veteran Affairs clinic | Trait anger, PTSD symptoms, and alcohol misuse | Aggression in the last 4 months | 31.8% with at least one act of physically aggressive behavior in the past 4 months, 27.7% with less severe physical aggression (i.e., threatening without a weapon), and 18.9% with more severe physical aggression (i.e., physical fight and threatening with a weapon). |
| Sayers, 2009 (62) | 199 | United States | Clinical assessment questionnaire | Clinical sample from Department of Veteran Affairs clinic | Combat exposure, PTSD, and alcohol misuse screening | Family reintegration problems, including self-reported domestic aggression in the past year | Over 75% of married or cohabiting veterans reported some type of family problem in the past week; 53.7% of veterans with current or recently separated partners reported conflicts involving shouting, pushing, or shoving. |
| Other study types | |||||||
| Jakupcak, 2007 (66) | 117 | United States | Clinical assessment questionnaire | Clinical series sample | Combat exposure and PTSD | Aggression (time period not specified) | 53.2% in PTSD group and subthreshold PTSD group endorsed at least one act of aggression compared with 20.4% in non-PTSD group. Combat exposure was positively associated with trait anger and hostility but not with aggression. Veterans who screened positive for PTSD reported greater recent aggression than did veterans who screened negative for PTSD (exp(β) = 4.17, 95% CI: 1.6, 10.7, P < 0.001) (after controlling for age and problem drinking). |
| Thomas, 2010 (19) | 13,226 | United States | Questionnaire survey | US combat brigade team | N/A | Aggressive behavior in the past month | Prevalence of aggression stable between 3 months and 12 months postdeployment: 35%–43% of soldiers threatened someone with physical violence or got angry enough with someone to kick, smash, or punch something, and 18% had gotten into a fight with someone and hit the person. |
| First Author, Year (Reference No.) . | Study Population . | Exposures . | Types of Violence and Timing . | Findings . | |||
|---|---|---|---|---|---|---|---|
| Sample Size, No. . | Location . | Data Type . | Population . | ||||
| Longitudinal studies | |||||||
| Elbogen, 2014 (59)a | 1,388 | United States | Postal survey | National sample from Department of Veteran Affairs | Combat exposure, violence prior to military service, PTSD, and alcohol misuse | “Severe violence” or “other physical aggression” in past year | 9% severe violence; 26% other physical aggression in last year. Severe violence/aggression associated with violence prior to military (OR = 3.95, 95% CI: 2.05, 7.62, P = 0.0001; OR = 2.51, 95% CI: 1.44, 4.37, P = 0.0011); combat exposure (OR = 1.03, 95% CI: 1.01, 1.05, P = 0.0066; OR = 1.04, 95% CI: 1.02, 1.05, P = 0.0001); and comorbid diagnosis of PTSD and alcohol use (OR = 4.09, 95% CI: 1.91, 8.77, P = 0.0003; OR = 3.45, 95% CI: 1.83, 6.50, P = 0.0001). |
| Sullivan, 2014 (64)a | 1,388 | United States | Postal survey | National sample from Department of Veteran Affairs | Combat exposure, history of violence prior to military service, PTSD, and alcohol misuse | “Severe violence” or “other physical aggression” toward family or toward stranger in past year | Family-directed acts in last year: 12.8% other physical aggression and 3.1% severe violence. Stranger directed acts: 9.5% aggression and 4.8% severe violence. High combat associated with severe family violence (OR = 3.96, 95% CI: 1.30, 12.02, P = 0.0153), stranger aggression (OR = 2.47, 95% CI: 1.39, 4.37, P = 0.002), and severe stranger violence (OR = 2.58, 95% CI: 1.14, 5.85, P = 0.0234). |
| MacManus, 2013 (60)b | 13,856 | United Kingdom | Questionnaire survey | United Kingdom military population | Self-reported deployment, role on deployment, combat exposures, postdeployment mental health (PTSD, alcohol misuse, aggressive behavior) | Offending records from United Kingdom Ministry of Justice Police National Computer database | 11% lifetime record of violent offense and 7% violent offenses postdeployment. Preservice violent offending strongest predictor of violent offending (aOR = 1.79, 95% CI: 1.34, 2.39, P < 0.0001). Deployment not associated with violent offending. Combat role associated with violent offending (aHR = 1.53, 95% CI: 1.15, 2.03; P = 0.003). Increased exposure to traumatic events during deployment associated with risk of violent offending (aHR = 1.65, 95% CI: 1.12, 2.40, P = 0.01; test for trend, P = 0.032). |
| Killgore, 2008 (56) | 1,252 | Questionnaire survey | US Army members returned from active duty | Combat experiences | Risk-taking propensity and aggressive behaviors in the last month | 2.2% got into a fight and hit a person, and 27% reported physical aggression. Violent combat exposure a predictor of risk-taking propensity (r = 0.30, F = 23.71, P < 0.001). No. of combat exposures correlated with verbal aggression and threats of violence. Killing the enemy and killing of nonhostiles were correlated with actual physical aggression toward others (r = 0.06, P < 0.05; r = 0.11, P < 0.0005, respectively). | |
| Wright, 2012 (57) | 1,397 | United States | Questionnaire survey | US Cavalry regiment | Combat exposure and internalizing symptoms (depression and anxiety) | Aggressive behavior in past month | 67.3% endorsed aggressive behavior. Combat exposure had small direct association with externalizing behaviors at follow-up (standardized path estimate = 0.14, P < 0.007) after accounting for internalizing symptoms and social environment. |
| Rabenhorst, 2012 (63) | 4,874 couples (6,063 individuals) | United States | Military records | National US military sample | Deployment | Rates of spousal abuse according to pre- and postdeployment official military records | Among abusive couples, the overall spousal abuse rate was 12.6% lower postdeployment. In couples where only one spouse abused and alcohol was involved, the abuse rate was significantly higher postdeployment. In couples where only the husband abused, the moderate or severe abuse rate was 24.0% higher postdeployment (RR = 1.24, 95% CI: 1.084, 1.444, P < 0.001), and when alcohol was used the abuse rate was 36.8% higher postdeployment (RR = 1.368, 95% CI: 1.055, 1.775, P < 0.05). |
| Schmaling, 2011 (65) | 546 | United States | Questionnaire survey | Nonrandom married or cohabiting personnel deployed to OIF | Rank, duty status, years in the service, previous deployments, and area of the most recent deployment | IPV and relationship dissolution in past year | At demobilization, 13.5% of participants reported IPV in the prior year. Deployment was not associated with IPV. |
| Cross-sectional studies | |||||||
| MacManus, 2012 (54)b | 10,272 | United Kingdom | Questionnaire survey | Random United Kingdom military population sample | Role on deployment, combat exposures, postdeployment mental health (PTSD, symptoms of common mental disorder, alcohol misuse) | Aggressive behavior in the weeks following homecoming | 12.6% were physically violent to either a member of their family and/or someone outside of their family. Violence associated with combat role (aOR = 2.0, 95% CI: 1.6, 2.5) and increased exposure to traumatic events (aOR for ≥4 traumatic events = 3.7, 95% CI: 2.5, 5.5). |
| Tsai, 2013 (61) | 30,968 | United States | Record based | US Department of Veteran Affairs records | Service in OEF/OIF/OND, combat exposure, and records of mental health diagnoses | Percentage of OEF/OIF/OND veterans incarcerated and incarcerated for a violent offense. Risk of incarceration among OEF/OIF/OND veterans compared with veterans of other eras and risk of incarceration for a violent offense | OEF/OIF/OND veterans less than half as likely as other veterans to be incarcerated and constituted only 3.9% of the incarcerated veterans; 37.5% of OEF/OIF/OND incarcerated veterans committed violent offense. The prevalence of violent offenders was similar among veterans of all eras. OEF/OIF/OND veterans were more likely to report combat exposure and were 3 times more likely to have combat-related PTSD. |
| Booth-Kewley, 2010 (49) | 1,543 | United States | Questionnaire survey | US Marines combat units | Combat exposure score, PTSD symptoms, and deployment-related stressors | ASB scale in past year | 22.9% scored high on ASB scale. The intensity of combat exposure was positively associated with ASB (very high combat: aOR = 1.81, 95% CI: 1.20, 2.73, P < 0.001). |
| Elbogen, 2012 (53)a | 1,388 | United States | Postal survey | National sample from Department of Veteran Affairs | Combat exposure, PTSD, and alcohol misuse | Severe violence or other physical aggression in past year | 33% committed ≥1 act of noncombat-related violence/aggression, and 11% committed ≥1 act of severe noncombat-related violence. Severe violence associated with combat exposure (aOR = 3.0, 95% CI: 1.85, 3.46, P < 0.001), alcohol misuse (aOR = 2.0, 95% CI: 1.28, 3.11, P = 0.0023), previous criminal arrests (aOR = 1.70, 95% CI: 1.07, 2.71, P = 0.0259), PTSD (aOR = 1.93, 95% CI: 1.21, 3.07, P = 0.0054), and homelessness (OR = 2.05, 95% CI: 1.0, 4.19, P = 0.0488). |
| Gallaway, 2012 (50)c | 6,128 | United States | Questionnaire survey | US Army combat units | Combat exposure in previous deployment, PTSD, depression, and alcohol misuse | Major and minor physical aggression in last year | 8% physical altercation with someone, 22% punching or hitting someone, 39% pushing or shoving someone, 4% using a knife or gun on someone. Minor aggression was associated with lifetime history of physical altercations with significant other (exp(β)d = 2.6, SE, 0.2, P < 0.01) and high combat intensity (exp(β) = 1.6, SE, 0.1, P < 0.01). Severe physical aggression was associated with lifetime history of physical altercations with significant other (exp(β) = 2.5, SE, 0.1, P < 0.01) and high combat intensity (exp(β) =1.5, SE, 0.1, P < 0.01). |
| Gallaway, 2013 (52)c | 6,002 | United States | Questionnaire survey | US Army combat units | Combat exposure, PTSD, depression, alcohol misuse, and self-reported criminal history (conviction) since joining military | Major and minor physical aggression in last year | 25.8% minor aggression, 21.0% major aggression, and 8% having a physical altercation with a significant other in the last year. Intensity of combat exposure was associated with severe aggression (aOR = 2.93, 95% CI: 2.4, 3.6), minor aggression (aOR = 3.52, 95% CI: 2.9, 4.3), reporting a physical altercation with a significant other (OR = 1.78, 95% CI: 1.3, 1.6), and a criminal conviction since joining the army (OR = 2.69, 95% CI: 1.8, 4.0). |
| Hellmuth, 2012 (48) | 653 | United States | Clinical assessment questionnaire | Clinical sample from Department of Veteran Affairs clinic | Trait anger, PTSD symptoms, and alcohol misuse | Aggression in the last 4 months | 31.8% with at least one act of physically aggressive behavior in the past 4 months, 27.7% with less severe physical aggression (i.e., threatening without a weapon), and 18.9% with more severe physical aggression (i.e., physical fight and threatening with a weapon). |
| Sayers, 2009 (62) | 199 | United States | Clinical assessment questionnaire | Clinical sample from Department of Veteran Affairs clinic | Combat exposure, PTSD, and alcohol misuse screening | Family reintegration problems, including self-reported domestic aggression in the past year | Over 75% of married or cohabiting veterans reported some type of family problem in the past week; 53.7% of veterans with current or recently separated partners reported conflicts involving shouting, pushing, or shoving. |
| Other study types | |||||||
| Jakupcak, 2007 (66) | 117 | United States | Clinical assessment questionnaire | Clinical series sample | Combat exposure and PTSD | Aggression (time period not specified) | 53.2% in PTSD group and subthreshold PTSD group endorsed at least one act of aggression compared with 20.4% in non-PTSD group. Combat exposure was positively associated with trait anger and hostility but not with aggression. Veterans who screened positive for PTSD reported greater recent aggression than did veterans who screened negative for PTSD (exp(β) = 4.17, 95% CI: 1.6, 10.7, P < 0.001) (after controlling for age and problem drinking). |
| Thomas, 2010 (19) | 13,226 | United States | Questionnaire survey | US combat brigade team | N/A | Aggressive behavior in the past month | Prevalence of aggression stable between 3 months and 12 months postdeployment: 35%–43% of soldiers threatened someone with physical violence or got angry enough with someone to kick, smash, or punch something, and 18% had gotten into a fight with someone and hit the person. |
Abbreviations: aOR, adjusted odds ratio; aHR, adjusted hazards ratio; ASB, antisocial behavior; CI, confidence interval; IPV, intimate partner violence; N/A, not applicable; OEF, Operation Enduring Freedom; OIF, Operation Iraqi Freedom; OND, Operation New Dawn; OR, odds ratio; PTSD, post-traumatic stress syndrome; RR, rate ratio; SE, standard error.
a Elbogen, 2012 (53),Elbogen, 2014 (59), and Sullivan, 2014 (64) are based on the same study sample.
b McManus, 2012 (54) and MacManus, 2013 (60) are based on the same study sample.
c Gallaway, 2012 (50) and Gallaway, 2013 (52) are based on the same study sample.
d Exponentiation of the β coefficient, which is an odds ratio.
The review assessed the quality of the eligible papers utilizing standard critical appraisal guidelines (43). The findings of all the studies are summarized qualitatively, and issues of quality are discussed as final conclusions from the review are drawn.
Studies were reviewed in order to compare characteristics, methods, and findings to determine the feasibility of completing a quantitative synthesis (i.e., meta-analysis) by exploring the completeness and methods of reporting of results and the homogeneity of the outcomes measured. Where a meta-analysis was appropriate, we estimated pooled prevalence with 95% confidence intervals using a random effects model that allowed us to assess heterogeneity between studies based on I2 statistics. Heterogeneity was categorized as low, moderate, or high on the basis of I2 values of 25%, 50%, and 75%, respectively. Because of the differences in types of aggression measured by each study, it was concluded that studies with prevalence rates for all types of aggression (undifferentiated) would be pooled together and that those with more similar measures of a specific type of aggression, such as fighting or hitting someone, would be pooled separately. We also carried out subgroup analyses of studies using similar period prevalence measures. We explored the feasibility of conducting a meta-analysis of the studies that explored the association between combat exposure and aggressive or violent behavior. As above, where possible, we proceeded with a meta-analysis.
Because of the relatively small number of studies included in both meta-analyses, it was not possible to explore sources of heterogeneity. Potential publication bias was also not examined as the power of funnel plot and statistical methods to detect publication bias in meta-analyses with less than 10 studies is limited (44). Meta-analyses were conducted by using the STATA 11 statistical package (StataCorp LP, College Station, Texas).
RESULTS
A total of 17 studies from the United States and the United Kingdom were reviewed: 1 descriptive study, 1 clinical series, 8 cross-sectional studies, and 7 longitudinal studies. A summary description of each of the studies is shown in Table 1; 13 of the studies explored only general aggression and violence, 3 studies specifically investigated family or partner/spousal aggression and violence, and 1 study explored both family and stranger aggression and violence.
General violence
Self-reported aggression and violence: descriptive study
In a study from the Walter Reid Institute of Army Research of 6 specific combat brigade units, 18,305 US soldiers were surveyed 3 and 12 months postdeployment in Iraq by using a nonanonymous questionnaire survey (Table 1) (19). Eighteen percent reported getting into a fight and hitting the person in the last month, with no significant difference between 3 and 12 months postdeployment follow-up. This study could potentially have underestimated the reporting of its outcome by the nonanonymous nature of the questionnaire (45), although this is a common limitation of studies in this area. This report did not examine the risk factors associated with aggressive or violent behavior nor did it compare the rates it found among deployed troops with the rates among nondeployed troops.
Self-reported aggression and violence: cross-sectional studies
Many of the studies that look at aggression and violence postdeployment were cross-sectional in design and used self-report outcome measures. Self-report measures are generally thought to underestimate the prevalence of aggressive or violent behavior, especially if a nonanonymous questionnaire is also used. However, the assessment of criminal history by use of self-report measures has been shown to have acceptable reliability (test-retest correlations of Q = 0.80) and acceptable-to-high validity (46, 47). Cross-sectional studies are also limited as causal interpretations can not be drawn from the results.
Hellmuth et al. (48) examined aggression among 359 US Iraq and Afghanistan combat veterans who had presented to a Department of Veterans Affairs health-care clinic for physical or mental health problems (Table 1): 31.8% reported at least one act of physically aggressive behavior in the past 4 months, 27.7% reported less severe physical aggression (i.e., threatening without a weapon), and 18.9% reported more severe physical aggression (i.e., physical fight). They did not look specifically at the link with deployment or combat exposure. In a nonanonymous, questionnaire-based, cross-sectional study of 1,543 US Marines enlisted in the US Armed Forces who had been deployed to Iraq or Afghanistan between 2002 and 2007, Booth-Kewley et al. (49) showed that 23% of this sample of combat-exposed Marines scored “high” on antisocial behavior. Combat exposure was positively associated with antisocial behavior after adjustment for a range of demographic and military confounders (Table 1).
Gallaway et al. (50) looked at a nonrandom sample of active duty US Army soldiers in Colorado. They reported the prevalence of self-reported physical aggression in the last 12 months (using questions from the physical assault subscale of the Revised Conflict Tactics Scale (51) excluding deployment-related aggression) at 6 months following return from deployment and the factors associated with lower and higher levels of aggression. Twenty-two percent of the soldiers reported punching or hitting someone, and 4% reported using a knife or gun on someone. Soldiers who were deployed and exposed to highest combat intensity reported more minor and severe physically aggressive actions compared with those who had not previously deployed. In multivariate analyses, the factors most strongly associated with minor and major aggression in the last year were lifetime history of physical altercations with a significant other, high combat intensity, and alcohol misuse (Table 1) (50). The authors acknowledge that the sample may not have been representative of all US Army soldiers, thus limiting the generalizability of the prevalence findings. They further showed that, in comparison with nondeployed soldiers, high combat exposure was significantly associated with general criminal behavior and physical altercations with a significant other (Table 1) (52). Indeed, the strength of the associations increased with increased cumulative exposure to combat.
In a national survey of a sample of 1,388 formerly serving US military personnel drawn from a random selection of over 1 million veterans, Elbogen et al. (53) found that over a third reported violent or aggressive behavior in the past year (using a composite measure from the Conflict Tactics Scale and the McArthur Community Violence Scale), although mostly involving minor aggressive behavior. Eleven percent reported one or more acts of severe non–combat-related violence. In this study, the authors stratified for “severe violence” (e.g., use of a weapon, threatened with a weapon, sexual violence) and “other physical aggression” (e.g., kicking, slapping, using fists, and getting into fights) (Table 1). Self-reported combat exposure and a previous arrest record were both independent predictors of both “severe violence” and “other physical aggression” on multivariate analyses (53).
Our group at King's College London used nonanonymous questionnaire data from a randomly selected sample of 10,272 United Kingdom military personnel in service at the time of the Iraq War in 2003 to explore the prevalence of and risk factors for violence following return from deployment, accounting for preenlistment antisocial behavior (Table 1) (54); 12.6% of Regulars reported having physically assaulted someone “in the weeks following deployment” (not a very precise outcome time period). Preenlistment antisocial behavior was the strongest predictor of this violence. After controlling for sociodemographic and military factors as well as preenlistment antisocial behavior, we found that combat role was still strongly associated with postdeployment violence. Consistent with other studies, our study found that the strength of the association with self-reported violence was shown to increase with the cumulative increase in number of exposures to traumatic events in combat.
In spite of the variation in outcome measurement, the majority of cross-sectional studies found a small-to-moderate association (odds ratio = 1.5–3.5) (55) between combat exposure, or specific combat experiences, and postdeployment physical aggression and violence, with several studies finding that the risk of violence increased with increased intensity and frequency of exposure to combat traumas (Table 1).
Self-reported aggression and violence: longitudinal studies
The temporal sequence of outcomes following the independent variables of longitudinal studies is a major advantage for causal inference. Killgore et al. (56) explored the link between different combat experiences reported immediately on return from deployment and risk-taking behaviors and aggressive behaviors reported 3 months later in a sample of 1,252 US soldiers returned from Operation Iraqi Freedom (42% of the original nonrandom sample) (Table 1). They found that 2.2% reported getting into a fight and hitting the person in the last month. The most consistent predictor of risk-taking propensity was “violent combat exposure,” which remained significant after controlling for demographic confounders, but it did not predict actual physical violence, probably because of low statistical power. A number of combat exposures were significantly correlated with verbal aggression and threats of violence, but killing the enemy and killing of nonhostiles were the only combat factors significantly correlated with actual physical aggression toward others in the preceding month.
Wright et al. (57) explored the link between combat exposures, externalizing behaviors (e.g., alcohol misuse, aggressive behavior, and risk-taking behavior), and internalizing symptoms in a survey of 1,397 (42%) soldiers from a US military unit 4 and 9 months postdeployment (only 589 followed up at 9 months) (Table 1). Their validated 4-item aggression scale (58) included an item on getting into a fight and hitting someone, as well as threatening violence. Notably, the sample reported experiencing high levels of combat exposure during their last deployment; 67% reported aggressive behavior in the past month, but this included verbal and physical threats of aggression and property aggression so it is not comparable with estimates of physical aggression alone. Combat exposure was associated with externalizing behaviors at both 4 and 9 months in the cross-sectional and longitudinal analyses, even after controlling for internalizing and social environment factors (57). Unfortunately they did not report on any separate relationship or path from combat exposure to individual externalizing behaviors, such as aggressive behavior.
Elbogen et al. (59) followed up their national sample of 1,388 formerly serving Iraq and Afghanistan veterans after 1 year (with a good retention rate of 79%). Overall, 9% endorsed engaging in severe violence (e.g., use of a weapon, threatened with a weapon, sexual violence) and 26% in other physical aggression (e.g., kicking, slapping, using fists, and getting into fights) in the previous year. This is one of the only studies, along with those by MacManus et al. (54, 60), to adjust for history of violence before military service, an important preenlistment factor. When this covariate and other covariates were adjusted for, combat exposure was still associated with severe violence and other aggressive behavior (Table 1) (59). Overall the longitudinal studies generally support the findings of the cross-sectional studies. The association between combat and aggression or violence ranges from small to moderate (odds ratio = 1.5–3.5) (55) even after adjustment for premilitary violence.
Offending records and incarceration studies
Tsai et al. (61), reported on a national study of 30,968 incarcerated formerly serving personnel, including 1,201 Iraq and Afghanistan veterans as well as those from other conflict eras (Table 1). Once again, the most common category of offense was violent offenses, and the proportion of incarcerated Iraq and Afghanistan veterans who were incarcerated for violent offenses was similar to the proportion of incarcerated veterans of other conflict eras incarcerated for a violent offense (37.5 vs. 35%). Iraq and Afghanistan veterans were more likely to report combat exposure and to suffer from combat-related PTSD than were other veterans. However, despite being a study of incarcerated veterans, it still relied on self-reported criminal offenses and nonstandardized measures of diagnoses and did not take account of the time since deployment. Hence, the finding that the most recent veterans (i.e., Operation Enduring Freedom/Operation Iraqi Freedom/Operation New Dawn) were less likely to be incarcerated may simply reflect differences in the time at risk rather than any true differences.
The King's College London group were able to link comprehensive data from a longitudinal study of a nationally representative sample of almost 14,000 United Kingdom military personnel with national offending records (Table 1) (60). Overall, the results were congruent with the previous work based on self-report of violence. Deployment itself was not found to be a risk for violent offending, but being deployed in a combat role and an increased burden of traumatic events on deployment significantly predicted subsequent violent offending. Although a history of violent offending prior to joining the military was the strongest risk factor for postdeployment violent offending, after adjustment for this factor and other factors, combat role and deployment-related traumatic events were still predictors of subsequent violent offending. While studies that use conviction records fail to capture the offenses that do not come to the attention of the police, they provide an objective assessment of the most serious offences, that is, those that attract a conviction.
Domestic violence
Fewer studies were found that focused on domestic or family violence among Iraq or Afghanistan veterans. In a cross-sectional survey of a small clinical population (n = 199), Sayers et al. (62) investigated family problems among recently returned military veterans who had served in Iraq or Afghanistan and who presented for a medical evaluation at the Philadelphia Veterans Affairs Medical Center (Table 1). Among veterans with current or recently separated partners, 54% reported conflicts involving shouting, pushing, or shoving in the past year. However, as the authors acknowledge, this was a small sample that was not representative of the US military.
Rabenhorst et al. (63) conducted the first population-based study of 4,874 married US Air Force personnel couples that compared spousal abuse rates (as recorded in military records) before and after combat-related deployments during Operation Enduring Freedom/Operation Iraqi Freedom (Table 1). They reported rates of incidents among couples who were engaging in partner abuse as opposed to the prevalence of perpetrators pre- and postdeployment. Among all abusive couples, the overall spousal abuse rate was 12.6% lower postdeployment. However, among specific couples in which only the husband abused and the abuse was moderate to severe, the rate increased. The rate increased even more if alcohol misuse was reported. A strength of this study is the use of objective record–based outcomes but, of course, as stated previously, studies that look only at recorded incidents are thought to underestimate the rates of violence, especially of domestic violence. This study is also limited to the Air Force, which, probably because of differences in selection and education, has lower rates of violent behavior than the other services.
In their 1-year follow-up study of their national sample of 1,090 US military personnel, Sullivan and Elbogen (64) compared rates of stranger versus family aggression and violence (the terms “severe violence” and “other physical aggression” merely distinguish between levels of severity of physical aggression) (Table 1); 13% reported any physical aggression or violence toward a family member during the year of study. This is a self-reported measure and may be an underestimation, but it is of interest that family-directed aggression or violence was found to be commoner than stranger-directed aggression or violence (9%). A history of arrest was positively associated with both stranger physical aggression and severe violence but not family physical aggression or severe violence. High combat exposure strongly predicted stranger aggression and severe violence, and it predicted severe family violence but not family aggression.
Schmaling et al. (65) conducted a longitudinal examination of predictors of intimate partner violence among 546 reservist military personnel using data from before and after mobilization for Operation Iraqi Freedom (Table 1). Following demobilization, 13.5% reported engaging in intimate partner violence in the previous year. However, this may be more a reflection of intimate partner violence during deployment rather than postdeployment. They also found that deployment was associated with less stress and more relationship satisfaction, but it is important to note that most of the sample were not on active duty and had not served before, so the results cannot be extrapolated to troops deployed on active duty or exposed to combat.
Overall, only 4 studies were found that examined domestic-related violence or explored the relationship between deployment and combat and domestic violence among Iraq and Afghanistan veterans. Although their methodological rigor varies, overall they suggest that aggression and violence within the family may be as prevalent as general aggression and violence and that, among regular troops, these behaviors may increase after deployment (although this was not shown among reservists who are not deployed on active duty (65)), and this may be related to the intensity of combat exposure. More research is required before any meaningful conclusions can be drawn.
Impact of premilitary violence
A number of the studies found that previous aggression and violence is more strongly associated with self-reported postdeployment violence than any deployment-related risk factor, including having served in a combat role (50, 54, 59). We, at King's College London, took this further by looking longitudinally at postdeployment violent offending using official offending records and were therefore able to control for premilitary violent offending (objective records). We found that it was the strongest risk factor for postdeployment violent offending (60). This was adjusted for in our multivariate analyses exploring the link between deployment and combat and postdeployment violent offending.
Meta-analyses
Prevalence studies
Of the 17 papers reviewed, 10 were included in meta-analyses of prevalence of aggressive or violent behavior postdeployment. Papers were excluded for a range of reasons: 5 papers contained data from overlapping samples (50, 52, 53, 59, 64) so only data from the 2 original studies were included (50, 53); 3 studies concerned intimate partner violence, spousal abuse, or domestic violence, and heterogeneous outcomes precluded a separate meta-analysis of the prevalence of intimate partner violence postdeployment (62, 63, 65); 1 study explored official offending records (60); and 1 examined rates of incarceration for violence (61). The outcomes of 2 further studies were not suitable for combination in a meta-analysis.
We examined studies that included a measure of “all aggressive behavior” postdeployment first (48, 49, 53, 56, 57) and then examined studies that specifically examined behavior that involved physically hitting someone in the postdeployment period (19, 48, 50, 54, 56). Figure 2 shows the forest plot of the weighted estimated mean prevalence of “all aggressive behavior.” The pooled estimate of prevalence was 36% (95% confidence interval (CI): 25, 48); this estimate had significant heterogeneity (I2 = 99.1%). The influence of one study (57) that included “verbal aggression” in their outcome measure on the pooled prevalence rate was explored by repeating the meta-analysis omitting this study. The pooled estimate reduced to 29% (95% CI: 25, 36), but the heterogeneity remained high (I2 = 95.6%). The subgroup analyses illustrated in Figure 3 show forest plots of the weighted estimated mean prevalence of “hitting someone” postdeployment in the last month or a longer period and show pooled estimates of 10% (95% CI: 1, 20) for the past month and 14% (95% CI: 6, 22) for the past year. Heterogeneity was lower among the 2 studies that explored the outcome in a longer prevalence period but still remained moderately high.
Forest plot of studies measuring “all aggression.” CI, confidence interval; ES, estimate [of prevalence].
Forest plot of studies measuring “hitting/assaulting another person.” CI, confidence interval; ES, estimate [of prevalence].
Association between combat and aggressive or violent behavior
Of the 10 papers that reported results of their examinations of the association between combat exposure and general aggression and violent behavior (49, 50, 52–54, 56, 57, 59, 60, 64), only 3 could be included in the meta-analysis. Seven papers contained overlapping data from 3 original study samples (50, 52–54, 59, 60, 64), and 3 studies did not report their findings in a manner that allowed combination with other studies (52, 56, 57). Figure 4 shows the forest plot of the estimated weighted odds ratios for the association between combat exposure and aggressive or violent antisocial behavior postdeployment with a pooled estimate across the 3 studies of 3.24 (95% CI: 2.75, 3.82); the level of heterogeneity was low (I2 = 0.0%, P = 0.394).
Forest plot of studies that examined the association between combat and aggression. (Data for the study by Elbogen et al. (59) use data pertaining to “other aggression.”) CI, confidence interval; ES, estimate [of odds ratio].
Studies of mediating factors
Several studies included measurement of postdeployment psychopathology and explored the role this may have in the link between deployment and combat and postdeployment violence. The studies were heavily focused on PTSD as the main psychopathology of interest, and some also explored alcohol misuse.
A study of a consecutive sample of 117 treatment-seeking Iraq and Afghanistan combat veterans presenting to a Department of Veterans Affairs center found that a significantly higher proportion of veterans with PTSD (53.2%) and subthreshold PTSD (52.4%) reported at least one act of violence in the past 4 months compared with a group without PTSD (20.3%) (Table 1) (66). They also found that those who screened positive for PTSD and subthreshold PTSD also reported greater aggressive behavior than those without PTSD. Although such a study is an initial indicator of a possible link between PTSD and violence among veterans of these conflicts, more robust methodology is needed to explore associations and mediation. Booth-Kewley et al. (49) found in their cross-sectional analyses that combat-exposed Marines with PTSD were over 6 times more likely to engage in antisocial behavior than those who did not have PTSD, thus suggesting an association between PTSD and antisocial behavior among Marines who had combat experience. In our cross-sectional population study of the United Kingdom Armed Forces, we found that mental health problems such as PTSD, alcohol misuse, and symptoms of common mental disorders were strongly associated with self-reported postdeployment violence (54, 60). Further, by linking our data with national offending registers to provide the timings of offending behavior, we show that postdeployment violent offending was predicted by previously reported postdeployment mental health and behavior problems (PTSD and alcohol problems and to lesser extent “symptoms of common mental disorder”) and indeed that these problems mediated some of the link between combat and traumatic exposures and violent offending (60). In the longitudinal study by Elbogen et al. (59) described above, they found that veterans with both PTSD and alcohol misuse had a substantially higher rate of subsequent severe violence (35.9%) compared with veterans with alcohol misuse without PTSD (10.6%), PTSD without alcohol misuse (10.0%), or neither PTSD nor alcohol misuse (5.3%). Upon multiple regression, veterans with PTSD without alcohol misuse were not at significantly higher risk of severe violence than were veterans with neither PTSD nor alcohol misuse.
Hellmuth et al. (48) modeled how PTSD symptom clusters, alcohol misuse, and anger related to aggression using pathway analysis of cross-sectional data from their clinical sample of 359 US Iraq and Afghanistan War veterans (Table 1). The PTSD-reexperiencing cluster and alcohol misuse were found to relate directly to aggression, whereas the PTSD-numbing and -hyperarousal clusters were indirectly related to aggression through trait anger. We found that, of the PTSD symptom clusters, the hyperarousal cluster was most strongly associated with subsequent violent offending (60). In their longitudinal study described above, Sullivan and Elbogen (64) found that PTSD anger symptoms predicted family aggression and violence but not stranger aggression and violence and that PTSD flashbacks predicted stranger aggression and severe violence but not family aggression and violence.
DISCUSSION
This review has appraised 17 papers that have investigated postdeployment violence, both general violence and violence against family, spouses, and partners, among veterans of the Iraq and Afghanistan conflicts. A number of the studies also explored the role of postdeployment psychopathology in the mediation of the link among deployment, combat, and violence.
Prevalence of postdeployment aggression and violence
The range of definitions and measures of aggression and violence continues to make interstudy comparisons difficult as studies used a different measure of aggression and violence or used the same measures but with different cutoffs or over different time periods. If we consider studies with the most similar outcome measure of physical acts of violence postdeployment, the pooled estimates of 10% in the last month and 20% in the longer time period should be accepted with caution given the high level of heterogeneity among the studies. This high heterogeneity could be in part explained by levels of operational tempo and combat exposure, enlistment status (still serving or nonserving personnel), and other specific characteristics of the study. The range of estimates in the United Kingdom compared with the United States was as follows: In the United Kingdom, 13% of a representative sample of serving and formerly serving deployed military personnel self reported getting into a fight and hitting someone in the weeks following deployment (54); 18% of a fairly comparable representative sample of deployed US troops self reported getting into a fight and hitting someone in the past month (19); a comparatively lower proportion of 2.2% of a nonrandom sample of returned Iraq veterans reported hitting someone in the last month in another study (56), and an apparently higher proportion, 22%, of a sample of still serving US combat personnel who reported high levels of combat exposure reported punching or hitting someone, but the time period of the last 12 months was comparatively longer (50). Studies that reported overall aggression found higher prevalence rates (pooled estimate of 29%–36% depending on whether verbal aggression was measured).
The self-report nature of most of the outcome measures remains a limitation of research in this area. As far as we know, we are the only group to date that has accessed objective measures of postdeployment violence (i.e., convictions) and, as expected, found that a lower percentage, 8% (which is also over a longer period of time), of our large representative sample of United Kingdom military personnel had a record of a violent offense postdeployment (60). The lack of studies that have explored aggression and violence among military personnel limits the possible exploration of differences between those still serving compared with formerly serving personnel.
We found only one study that estimated the prevalence of postdeployment intimate partner violence perpetration among a nonclinical sample of Iraq and Afghanistan veteran reservists (65). Rabenhorst et al. (63) looked at rates of incidents among couples who were engaging in partner abuse as opposed to prevalence of perpetrators pre- and postdeployment. Sullivan and Elbogen (64) found that 13% of their national sample of nonactive Iraq and Afghanistan veterans reported physical aggression and violence toward a family member, which is an important differentiation from stranger violence although it does not specify partner violence.
In summary, estimates of the prevalence of postdeployment violence among Iraq and Afghanistan veterans depend on the sample under study and the definition and measure of aggression and violence used. With one exception (56), the studies in this review highlight that this behavior is prevalent among serving and formerly serving personnel (estimates of 10% for physical assault and 29% for all types of physical aggression in the last month) and worthy of further exploration. Further research into the prevalence of postdeployment domestic violence is required, especially into partner- and family-directed violence.
Impact of deployment and combat on risk of postdeployment aggression and violence
Most of the research into violence among combat veterans has been carried out in the United States, much of which has utilized data from past conflicts, such as the Vietnam War and the 1990–1991 Gulf War. The results have been mixed. A number of these studies found associations between combat exposure (rather than deployment) and physical aggression and incarceration postdeployment (24–28). However, other studies did not find that combat exposure itself but rather certain combat exposure, such as participating in war-zone violence, predicted violence postdeployment (31). Others found premilitary characteristics to be the strongest risk factor for postdeployment violence (32, 33). Postdeployment intimate partner violence is a form of violence that has received much research attention in the United States. A number of pre–Operation Enduring Freedom/Operation Iraqi Freedom studies found an association between combat exposure and intimate partner violence perpetration (29, 30, 67). In contrast, a number of studies found no significant difference in the perpetration of domestic violence between veterans with combat experience and those without, although these studies did not examine specific combat-related variables (68).
In this review of studies of Iraq and Afghanistan, in spite of the variation in outcome measurement and study design, the majority of studies supported a small-to-moderate (55) association between combat exposure and postdeployment physical aggression and violence (42, 49, 50, 52–54, 56, 57, 60, 69) with several studies finding that the risk of violence increased with increased intensity and frequency of exposure to combat “traumas” (50, 52, 54, 60). Our limited meta-analysis of a subset of studies from both the United States and the United Kingdom estimated a pooled unadjusted odds ratio of 3.24 (95% CI: 2.75, 3.82). Despite the limitations of cross-sectional studies, their results are consistent with those studies which have used a longitudinal design. The only population-based longitudinal study that utilized an objective measure of both premilitary violent offending and postdeployment violent offending confirmed these findings (60).
The major limitation of most of the research to date among Iraq and Afghanistan veterans has been the neglect of premilitary risk of violence. Background violence risk factors are important to consider in the etiology of postdeployment violence when attempting to tease out the relative impact of deployment and combat. Research from the general population has shown that childhood antisocial behavior impacts on later antisocial behavior and criminality (70). Premilitary antisocial behavior may reflect a predisposition for such behavior, which may continue into adulthood irrespective of the impact of military service. Our group at King's College London found that the impact of preenlistment antisocial behavior on negative military behavioral outcomes in personnel deployed to Iraq was strongly independently associated with severe alcohol misuse, outbursts of anger or irritability, fighting or assaultative behavior, and risk-taking behavior (71). A number of studies of veterans from the Vietnam era found that prewar antisocial behavior was a stronger predictor of veteran violence than combat exposure (32, 33, 72). Similar to the Vietnam-era literature, the studies in this review of the Iraq and Afghanistan eras found that previous antisocial behavior or aggression was more strongly associated with postdeployment violence than combat exposure. However, combat exposure was still significantly associated on multivariable analyses (50, 54, 60). This review shows clearly that the association between combat and violence cannot be explained away solely by selection and ipso facto that improved recruit screening will not solve the problem. Whether or not better training or better postdeployment support might mitigate the link is an empirical question that we have not yet begun to address. However, the seductions of screening for vulnerability mean that it is something that is proposed from time to time for various reasons, even if there is still a lack of any robust evidence base to support it (73). One reason for not screening out those at risk of perpetrating violence is that it is well recognized by the military and the public alike that a proportion of military recruits come from difficult backgrounds and that enlisting in the military may be the changing point in the lives of many who go on to acquire education, training, skills, discipline, and self-esteem that they might never otherwise have had the opportunity to achieve (74). This review, however, clearly demonstrates that, for some, the military may provide an environment for continued and increasing violent behavior. These results highlight that ongoing violent behavior and increased violence postdeployment may be a concern among military personnel, especially among those with a history of offending prior to enlistment.
The role of psychopathology in the link between deployment to Iraq and Afghanistan and postdeployment violence
Most studies from the pre-Iraq and Afghanistan eras proposed that PTSD was an important mediator in the association between combat (trauma) and violent behavior (34–37). PTSD was frequently shown to be significantly related to both combat and violent and aggressive acts among veterans of previous conflict eras (27, 33, 40, 75–79). A body of research also established that a relationship exists between PTSD and intimate partner violence perpetration among US veterans (36, 80), and some have found the association between certain deployment experiences and intimate partner violence to be largely accounted for by PTSD symptoms (29).
Similar to pre-Iraq and Afghanistan studies, many studies of Iraq and Afghanistan veterans demonstrated a link between PTSD and postdeployment violence (42, 54, 59, 66), and some have provided evidence that PTSD can play a mediating role between combat exposure and violence (48, 60). Studies of pre-Iraq and Afghanistan era veterans found different aspects of the symptomatology to be specifically related to postdeployment violence, such as hyperarousal (40, 81), avoidance and numbing symptoms (40), or comorbid dysphoria (81). Studies in this review also suggest that, among Iraq and Afghanistan veterans, the clusters and indeed individual symptoms of PTSD relate differently to behavior with varying evidence for the specific role of hyperarousal (42, 60), flashbacks (64), and PTSD-related anger and irritability (64) in postdeployment violence. To add further complexity, Miller et al. (82, 83) reported that, among Vietnam combat veterans, those who internalized combat-related PTSD had high prevalence rates of panic and depression and were more likely to experience their distress internally through mood and thoughts. Those who externalized were more likely to express distress outwardly through behaviors and had high rates of antisocial personality traits, alcohol-related behaviors, and histories of delinquency. Rielage et al. (84) showed that this personality model of PTSD comorbidities can also be applied in the Iraq and Afghanistan veteran populations. Thus, the earlier studies showing a link between PTSD and postdeployment violence may not account for personality traits.
Although PTSD is perhaps the most researched diagnosis when considering violence in combat veterans, there is literature suggesting that other psychopathologies can be linked with violence. Alcohol misuse has been shown to be strongly associated with aggressive behavior among combat veterans (39, 40). PTSD with comorbid alcohol dependence has also been shown to lead to greater violence than PTSD alone, hypothetically because of the effect on hyperarousal symptoms (39). Among studies of Vietnam veterans, direct relationships were found between alcohol misuse and PTSD symptoms and the frequency of intimate partner violence perpetration (85, 86). As this review shows, evidence is also emerging from Iraq and Afghanistan veterans to suggest the modifying effect of alcohol misuse on comorbid conditions such as PTSD to increase risk of postdeployment violence (48, 59). Indeed, the most recent study by Elbogen et al. (59) has suggested that, in the absence of alcohol misuse, PTSD is not associated with severe violence postdeployment but is associated with lesser physical aggression. These findings suggest that adjunct treatments aimed at stabilizing anger and alcohol misuse may help clinicians to ameliorate the maladaptive patterns that are often observed in veterans.
Findings from the United States suggest high rates of postdeployment PTSD with estimates of 10%–20% of returning US servicemen and women experiencing symptoms (87–89). With PTSD rates shown to be lower in the United Kingdom, the actual impact of this risk factor on violence at a population level may be less pertinent than among US military cohorts (90). This does not, however, affect the importance of PTSD as a risk factor for violence at an individual level. The converse may be true for alcohol misuse, which is a greater problem among the armed forces of the United Kingdom than among those in the United States (22) and was observed to increase among United Kingdom combat troops following return from deployment to Iraq or Afghanistan (16).
Implications
This growing body of literature emerging on veterans of the Iraq and Afghanistan conflicts provides evidence that postdeployment violence is a problem for a subgroup of veterans and that exposure to combat is one among many risk factors for violence in this population, which may be partly mediated by postdeployment mental health problems such as PTSD and alcohol misuse. As both the United States and the United Kingdom face the long-term consequences of 10 years of combat in Iraq and Afghanistan, this work provides information for developing a strategy to tackle issues related to risk of violence in military personnel.
However, the literature so far does not include an examination of the effectiveness of postdeployment violence screening and, therefore, despite pressure from the media in the wake of incidents like the Fort Hood shootings (91), implementation of any screening program should be based on the use of valid tools of assessment, as well as demonstrable effectiveness in the management of those identified by the program, preferably in a randomized controlled trial. The military is composed of a range of individuals, some roles require aggressive traits, and personnel are trained to respond to certain situations with targeted aggression. Interventions for military personnel on return from deployment to help these individuals adapt their responses to community and family environments may be more acceptable and potentially valuable. This evidence can be used to begin trial interventions targeted at the factors showing signs of being on the causal pathway.
Future research
This review has highlighted the lack of standardized practices in this area of research. We therefore recommend that future research give more consideration to the standardization of data collection instruments and that efforts are made to obtain objective information where possible through accessing criminal records. Research to date has been heavily weighted toward general violence. We suggest that this needs to be more focused and, in particular, that more work is needed on the prevalence of and risk factors for violence against the family by military personnel. Perhaps this will in time also help inform prevention and management strategies. We also have noted the focus on the role of PTSD in postdeployment violence, and we suggest that in the future more attention perhaps needs to be given to other mental disorders and most specifically to substance misuse.
ACKNOWLEDGMENTS
Author affiliations: King's Centre for Military Health Research, King's College London, Weston Education Centre, London, United Kingdom (Deirdre MacManus, Roberto Rona, Nicola Fear, Simon Wessely); Department of Forensic and Neurodevelopmental Science, Institute of Psychiatry, London, United Kingdom (Deirdre MacManus, Greta Somaini); Academic Centre for Defence Mental Health, Weston Education Centre, London, United Kingdom (Nicola Fear, Simon Wessely); and School of Psychology, University of West London, London, United Kingdom (Hannah Dickson).
N. F. and S. W. are employed by the Academic Centre for Defence Mental Health, based at King's College London, which receives funding from the Ministry of Defence of the United Kingdom. S. W. is also honorary civilian consultant advisor in psychiatry to the British Army and a trustee of Combat Stress, a United Kingdom charity that provides service and support for veterans with mental health problems. Financial support was also received from the Department of Health via the National Institute for Health Research (NIHR) Comprehensive Biomedical Research Centre Award to Guy's & St Thomas’ National Health Service Foundation Trust in partnership with King's College London and King's College Hospital National Health Service Foundation Trust.
Conflict of interest: none declared.
REFERENCES
Author notes
Abbreviations: CI, confidence interval; PTSD, post-traumatic stress disorder.



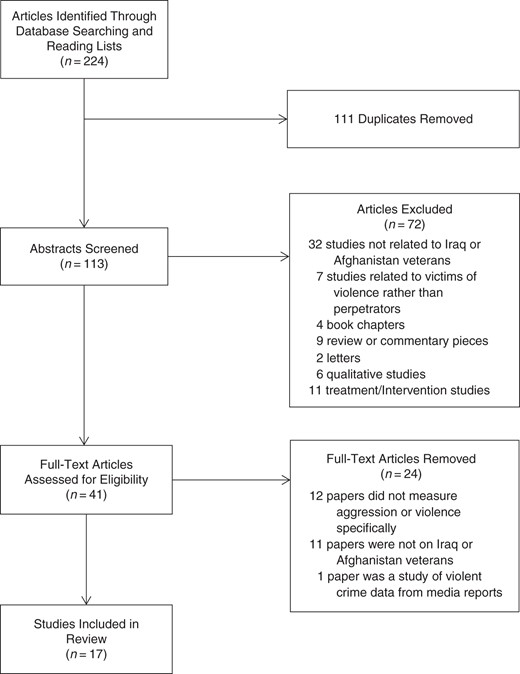
![Forest plot of studies measuring “all aggression.” CI, confidence interval; ES, estimate [of prevalence].](https://oup.silverchair-cdn.com/oup/backfile/Content_public/Journal/epirev/37/1/10.1093_epirev_mxu006/3/m_mxu00602.jpeg?Expires=1716405600&Signature=a6al4HMeRg~BeBRNsQZwz8nsWfI5M7Eu6BJuTkAI6ThMG74gJ3iiSDGjV7OtehiojngiJfIVKgHuEqwNnxRhoxL98czf6SHFwk~M1TDfOUxcvsIZt9ddd0iIwvXvGL5CMerOcESNp7HSzeh8g~0P-gsr1OG34FgAj6JE-De2LvqMzqYWe~xXuBUGwdUk8fwtUJRjTvwOwBdh8Bg-XmBv0bDxzHDrUEFuHVx80GKs5umoNBjvuztfCHLEcTrialluRUaC6euTyFK3yewrZD6Hir40jkUGuvv6MbqirLPLH3zifOGpsdT3ag8WJCRtBpvLDxTWXv6Q9N00KCwbfZEZgw__&Key-Pair-Id=APKAIE5G5CRDK6RD3PGA)
![Forest plot of studies measuring “hitting/assaulting another person.” CI, confidence interval; ES, estimate [of prevalence].](https://oup.silverchair-cdn.com/oup/backfile/Content_public/Journal/epirev/37/1/10.1093_epirev_mxu006/3/m_mxu00603.jpeg?Expires=1716405600&Signature=eF7SAUvg6cdvpn1gjfWyjfCRg4zUMMDl81oAOfBkCuV~n~j7fBig4GzyLOx5Kfy4693xxOw47iBBmm6HPvd~U15YQlpBnvTgk4SF2NmUhW38min2uhLAdwfMcAkIacm-Lq6OJ7~Wwwvvs6kzyJQIq4tde9z2swtIuhT3W1GEggE6450KGDpufxbsYaCRc1lClJm2kqdaKLy1X6kppsEX-Db1KnV8oJQwdLiKWv5Hwia69Fv0HMFMEPgXae7uuW7OvETefWWH~9ecNrvS0T6VNcf6fSKMyanc0kOYkvlgNCY2jSJilNs9POm44SWBRAEcP0cKm0ZdBUo1tSs-1J8Z-Q__&Key-Pair-Id=APKAIE5G5CRDK6RD3PGA)
![Forest plot of studies that examined the association between combat and aggression. (Data for the study by Elbogen et al. (59) use data pertaining to “other aggression.”) CI, confidence interval; ES, estimate [of odds ratio].](https://oup.silverchair-cdn.com/oup/backfile/Content_public/Journal/epirev/37/1/10.1093_epirev_mxu006/3/m_mxu00604.jpeg?Expires=1716405600&Signature=jdADrktt-4s8YQmqulRQqQrp8TjJuC3sj89Dx-CTcm~UEo7anMN4ndszPxsAJfEy1oq3uLKf5WtC0WvkqeBwam3-Wu3Hzh03zyMI9VZ67805bkx7fTLaTN0Hgj9xVz2FvO39zCaQ4UEV09OxXYM0K5TUTdCp6tU1VW72Ovpihz4Wd1EfogISHH2Y9Lc6Ed~PfSdAETIxN0AhvRJWuT8LGlQLSbWqb3chPcFP6DIRhg2GJAmaysuKyCNlA7shk9A1e1cx4ATTejM9jYARxW7AdlwJbeI94NtWBXzQdTJo82U~qvE0tCI0orSqJEA6Ue67FvciUtAzrTdvHdTbqKxCmg__&Key-Pair-Id=APKAIE5G5CRDK6RD3PGA)
