-
PDF
- Split View
-
Views
-
Cite
Cite
Laura A. Cousins, Lindsey L. Cohen, Claudia Venable, Risk and Resilience in Pediatric Chronic Pain: Exploring the Protective Role of Optimism, Journal of Pediatric Psychology, Volume 40, Issue 9, October 2015, Pages 934–942, https://doi.org/10.1093/jpepsy/jsu094
Close - Share Icon Share
Abstract
Objective Fear of pain and pain catastrophizing are prominent risk factors for pediatric chronic pain-related maladjustment. Although resilience has largely been ignored in the pediatric pain literature, prior research suggests that optimism might benefit youth and can be learned. We applied an adult chronic pain risk-resilience model to examine the interplay of risk factors and optimism on functioning outcomes in youth with chronic pain. Method Participants included 58 children and adolescents (8–17 years) attending a chronic pain clinic and their parents. Participants completed measures of fear of pain, pain catastrophizing, optimism, disability, and quality of life. Results Consistent with the literature, pain intensity, fear of pain, and catastrophizing predicted functioning. Optimism was a unique predictor of quality of life, and optimism contributed to better functioning by minimizing pain-related fear and catastrophizing. Conclusions Optimism might be protective and offset the negative influence of fear of pain and catastrophizing on pain-related functioning.
Chronic or recurrent pain, pain that persists for a minimum of 3 months (Task Force on Taxonomy, 1994), impacts approximately 25% of children and adolescents, with 54% of youth reporting a significant pain episode within the previous 3 months (King et al., 2011; Perquin et al., 2000). Children and adolescents with chronic pain are vulnerable to adverse outcomes, such as disability and impaired quality of life (QOL; Gold et al., 2009; Walker & Greene, 1991). Clearly, pediatric chronic pain is a significant health concern.
In the past several years, risk-resilience models specific to adult chronic pain have been used to conceptualize the complexity of the pain experience and identify potential pathways for intervention (Sturgeon & Zautra, 2013). Whereas risk factors are described as those variables that increase the likelihood of negative outcomes, resilience is commonly defined as the experience of positive outcomes despite exposure to adversity (Masten, 2001). Management of a chronic medical condition, such as chronic pain, represents a health-related challenge, and a number of variables might be described as risk or resilience factors that influence the patient’s QOL and functioning. Risk-resilience models have been applied to pediatric chronic illness (Hilliard, Harris, & Weissberg-Benchell, 2012; Koinis-Mitchell et al., 2012), and these models describe how individual, family, social, and cultural factors might relate to health, illness management, adaptability, and psychosocial functioning. Although researchers have identified a number of risk factors for pediatric pain populations (Pagé, Huguet, & Katz, 2013), and authors have recognized the importance of resilience (Huguet, McGrath, Stinson, Chambers, & Míro, 2011), there is a dearth of data around resilience and there are no risk-resilience models proposed for pediatric chronic pain.
Arguably, the two most commonly studied risk factors in the pediatric chronic pain literature are fear of pain (Simons, Sieberg, Carpino, Logan, & Berde, 2011) and pain catastrophizing (Vervoort, Goubert, Eccleston, Bijttebier, & Crombez, 2006). Given that these risk factors have been extensively examined and ample data indicate their contribution to poor outcomes and maladjustment in youth with chronic pain (Simons & Kaczynski, 2012), they will not be the focus of discussion.
In contrast to risk factors, resilience factors have largely been ignored in pediatric pain (Huguet et al., 2011). However, in the larger field of health psychology, dispositional optimism has garnered ample attention as an important source of resilience (Carver, Scheier, & Segerstrom, 2010). Dispositional optimism is the extent to which an individual upholds generalized favorable expectancies for the future (Scheier & Carver, 1985), and data suggest that people who are high on optimism maintain confidence in achieving an outcome and persevere even when confronted with adversity (Carver et al., 2010). Optimists appear to persist more in academic and professional pursuits, better balance simultaneous goals, put more effort into relationships, report having more social support, report more benefit finding when confronted with adversity, and are more likely to engage in health-promoting behaviors (Carver & Scheier, 2014). Adolescents who are less optimistic reported more negative affect, depression, hopelessness, recent hassles, suicidal ideation, substance abuse, anger, and poorer health care practices (Lemola et al., 2010). In a meta-analysis of optimism and coping, Nes and Segerstrom (2006) found that optimistic individuals used more adaptive and flexible coping strategies, which contributed to better emotional and physical health outcomes. A later meta-analysis illustrated that optimism had a significant positive effect on physical health for all biomarkers considered, including immune function (Rasmussen & Scheier, 2009).
Optimism’s beneficial effects on physical health have also attracted some controversy, as several studies have found no effect or negative effects (Coyne, Tennen, & Ranchor, 2010). It has been suggested that optimism is negatively related to immunity when continually engaging with complex, persistent, or uncontrollable stressors, but positively related to immunity when engaging with brief, straightforward, or controllable stressors (Segerstrom, 2005).
In terms of optimism and pain, data with adults with chronic pain suggest that optimism is a protective factor (Goodin & Bulls, 2013). Using the cold pressor as a pain stimulus, researchers found that pain catastrophizing mediates the relation between optimism and self-reported pain in healthy adults, with those lower in optimism reporting higher catastrophizing and pain (Hanssen, Peters, Vlaeyen, Meevissen, & Vancleef, 2013; Hood, Pulvers, Carrillo, Merchant, & Thomas, 2012). In addition, Hanssen et al. (2013) demonstrated a causal link between optimism and experimental pain perception via an experimental manipulation of optimism. These data and other research suggesting optimism might be trained or learned (Seligman, 1991) are promising for future work with chronic pain patients.
The construct of optimism has only recently received attention in the pediatric literature. Examining a sample of healthy children and children with cancer, Williams, Davis, Hancock, & Phipps (2010) found that higher optimism was associated with lower self-reported pain and improved behavioral and emotional functioning. Also examining pediatric patients with cancer, Mannix, Feldman, and Moody (2009) found that higher optimism was related to decreases in pain reports, greater communication with physicians, increased psychological functioning, and better overall QOL. No studies to date have examined optimism in pediatric patients with chronic pain.
Whereas optimism is generally defined as a personality trait, it has also been conceptualized as an explanatory style (Peterson et al., 1982). Individuals with an optimistic explanatory style attribute negative events to external factors and interpret these events as temporary and proximal. Conversely, positive events are attributed to internal factors that are enduring and global. Thus, an optimistic explanatory style minimizes the overwhelming impact of adversity or setbacks, while emphasizing positive situations and their influence on future cognition and behavior. Most interestingly, individuals can learn how to foster an optimistic explanatory style by altering the way they interpret positive and negative events (Seligman, 1991). Given that optimism might be learned (Hanssen et al., 2013; Seligman, 1991), it could be incorporated into pain management interventions to mitigate the impact of pain-specific negative appraisals and emotions, such as catastrophizing and fear of pain.
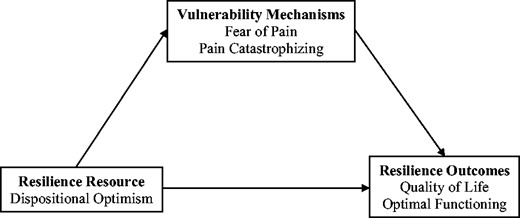
Sturgeon and Zautra’s (2010) risk-resilience model for adult chronic pain defines resilience resources as stable personal characteristics that enhance the likelihood of resilient outcomes. Conceptually, resilience resources increase the likelihood of adaptive outcomes through the promotion of resilience mechanisms (cognitions, affects, and behaviors used while experiencing pain that sustain functioning) or the minimization of vulnerability mechanisms (e.g., pain-related fear, catastrophizing). Thus, modifiable resilience and vulnerability mechanisms arguably mediate the relation between resilience resources and resilient outcomes. Theoretically, resilience resources are suggested to counteract the limited cognitive and emotional focus on threat-relevant cues, as a result of catastrophizing and pain-related fear, by broadening identification of potential supports and strengths and more effective coping strategies (Sturgeon & Zautra, 2013). The purpose of the present study was to apply Sturgeon and Zautra’s risk-resilience model to a sample of youth with chronic pain. Pain-related fear and pain catastrophizing were selected as the risk factors, optimism as the resilience factor, and disability and QOL as the outcomes (Figure 1). The first aim was to evaluate associations among optimism, fear of pain, pain catastrophizing, disability, and QOL. We expected that higher optimism would be associated with reduced disability, fear of pain, and pain catastrophizing and better QOL. We also expected that higher fear of pain and pain catastrophizing would be associated with greater disability and poorer QOL. The second aim was to explore the mediational relations among optimism, pain-related risk factors (fear of pain and pain catastrophizing), and functioning outcomes (disability and QOL). Consistent with Sturgeon and Zautra’s risk-resilience model, we predicted that both fear of pain and pain catastrophizing would mediate the effects of optimism on disability and QOL.
The mediational effect of vulnerability mechanisms on the relation between optimism and resilience in pediatric chronic pain. Adapted from “Resilience: A New Paradigm for Adaptation to Chronic Pain,” by J. A. Sturgeon and A. J. Zautra, 2010, Current Pain and Headache Reports, 14, p. 107. Copyright 2010 by Springer.
Methods
Participants
A power analysis for a regression with three predictors and power of 0.90 revealed that 52 participants would be needed to detect a medium effect size. Inclusion criteria were participants who were diagnosed with chronic pain (i.e., experienced pain for a minimum of 3 months) and proficient in English. Exclusion criteria included severe developmental delays or the diagnosis of another chronic medical condition that was not pain-related to assure that outcomes were exclusively related to the impact of pain. Chart review was conducted to identify pain diagnoses and duration of pain. Sixty-five children and their families were approached to participate in the present study. Five families declined to participate due to a lack of interest (n = 3), preoccupation with other activities (n = 1), and having a child who was experiencing significant distress (n = 1). Further, two participants were excluded because they failed to complete any measures. Thus, the final sample consisted of 58 children and adolescents with chronic pain and their parents.
Participants included children and adolescents between the ages of 8 and 17 years (M = 14.60 years, SD = 2.27 years) who were newly scheduled or returning for a multidisciplinary outpatient pain clinic appointment at two large, urban, southeast pediatric hospitals. Participants were predominantly female (79.3%), White (59.6%), and Not Hispanic or Latino (94.8%). However, 31.6% were Black or African American and 8.8% identified as Multiracial. The majority of participants were accompanied by their mother (86.2%). Participant pain diagnoses included generalized amplified pain syndrome or musculoskeletal pain (25.5%), abdominal pain (19%), multiple pains (15.3%), migraines (5.2%), back pain (5.2%), foot pain (5.2%), knee or leg pain (5.2%), juvenile idiopathic arthritis or joint pain (4%), complex regional pain syndrome (3.4%), polyarthralgias (2%), bilateral hip dysplasia (2%), and other pain (8%; e.g., elbow, chest, head, facial). Mean duration of pain exceeded 2 years, M = 32.27 months (SD = 37.51). One participant’s pain diagnosis and duration of pain was not listed. Approximately 26% of participants endorsed having a psychological disorder, which was self-described as anxiety (40%), depression (26.7%), attention-deficit/hyperactivity disorder (6.7%), or multiple diagnoses (26.7%). Parents reported a median annual income of $40,001–$50,000, with six families not reporting their annual income.
Procedure
Appropriate hospital and university institutional review boards approved the study. Research assistants approached participants when they arrived for their regularly scheduled outpatient appointment. All measures were completed in the clinic rooms while participants waited to see health care providers. Measures were completed in the order listed.
Measures
Background Information
Parents completed the Background Information Form. This questionnaire includes questions about the parent (e.g., relation to child, gender, age, ethnicity, race, education, occupation, family income, and health status) and the child (e.g., gender, age, ethnicity, race, and health status).
Pain Intensity
Pain intensity was assessed using a 10-cm visual analog scale (VAS), asking participants to rate (a) their general pain during the past week and (b) their worst pain during the past week from 0 (no pain) to 10 (worst possible pain). VASs have demonstrated reliability and validity and are classified as well-established instruments for pain assessment (Cohen et al., 2008), with children as young as 6 years of age (von Baeyer, 2006).
Pain-Related Fear
The Fear of Pain Questionnaire, child report (FOPQ-C; Simons et al., 2011) is a 24-item measure with two subscales, Fear of Pain and Avoidance of Activities, assessing child perceptions of pain-related fears and avoidance behaviors. This instrument uses a 5-point Likert scale from 0 (strongly disagree) to 4 (strongly agree), with higher scores indicating higher levels of pain-related fear. The FOPQ-C has been shown to have good internal consistency, acceptable 1-month stability estimates, and construct validity among a sample of 8–17-year-olds with chronic pain (Simons et al., 2011). In the current sample, Cronbach’s α was .94, indicating good reliability.
Pain Catastrophizing
The Pain Catastrophizing Scale for Children (PCS-C; Crombez et al., 2003), an adaptation of the Pain Catastrophizing Scale (Sullivan, Bishop, & Pivik, 1995), consists of 13 items assessing negative thinking in the context of pain (e.g., “When I am in pain, I keep thinking about how much it hurts”). Children report how frequently they experience each thought or feeling using a 5-point scale ranging from 0 (not at all) to 4 (extremely), with higher scores representing greater catastrophic thinking. The total score, ranging from 0 to 52, is derived from the sum of three subscale scores for rumination, magnification, and helplessness. The PCS-C has demonstrated construct, internal, and predictive validity in 8–17-year-old community and chronic pain samples (Crombez et al., 2003). Internal consistency in the current sample was good with a Cronbach’s α of .90.
Optimism
The Youth Life Orientation Test (YLOT; Ey et al., 2005) is a developmentally appropriate measure of dispositional optimism in children, created as a downward extension of the Life Orientation Test (Scheier & Carver, 1985), a well-established measure of dispositional optimism in adults. Children rate their agreement on seven optimism items (e.g., “I usually expect to have a good day”), seven pessimism items (e.g., If something nice happens, chances are it won’t be to me”), and two filler items (e.g., “I like to be active”) using a 4-point Likert scale format (3—true for me, 2—sort of true for me, 1—sort of not true for me, and 0—not true for me). Both a total score (i.e., global optimism) and subscale scores for optimism and pessimism can be calculated. In this study, the optimism subscale was used as prior studies have recommended optimism and pessimism be examined separately given their differential impact on outcomes (Williams et al., 2010). The test–retest reliability of the YLOT has ranged from 0.68 to 0.70 over a 1-month period, and intraclass correlations of .65 to .75 across 7 months have been found (Ey et al., 2005). The two-factor structure and validity of the YLOT has been demonstrated with children with cancer and healthy controls between the ages of 7 and 18 years (Williams et al., 2010). Associations between the YLOT and measures of competency, hope, and psychological adjustment have also provided support for the YLOT’s convergent and discriminant validity (Ey et al., 2005). Internal consistency in the current sample was good with a Cronbach’s α of .87.
Functional Limitations
The Functional Disability Inventory (FDI; Walker & Greene, 1991) is a 15-item self-report measure that assesses children’s perceived difficulty in physical and psychosocial functioning due to their physical health (e.g., “Doing chores at home”). Children are asked to rate their perceptions of activity limitations during the past 2 weeks on a 5-point scale ranging from 0 (no trouble) to 4 (impossible). The FDI has demonstrated reliability and validity in children and adolescents (Claar & Walker, 2006; Walker & Green, 1991) and was selected for this study given its frequent administration to youth with a range of chronic pain conditions (Palermo & Kiska, 2005). Internal consistency in the current sample was good with a Cronbach’s α of .78.
Quality of Life
Participants completed the Pediatric Quality of Life Inventory (PedsQL 4.0 Generic Core Scale; Varni, Seid, & Kurtin, 2001), which has four subscales assessing physical, emotional, social, and school functioning that have been validated with children and adolescents between the ages of 5 and 18 years (e.g., “I cannot do things that other kids my age can do”). Respondents report the extent to which each item has been problematic over the past month using a Likert 5-point scale (0 = never a problem, 1 = almost never a problem, 2 = sometimes a problem, 3 = often a problem, and 4 = almost always a problem). Raw scores are transformed into standard scores ranging from 0 to 100, with higher scores indicating better functioning. The PedsQL has well-established reliability and validity in pediatric pain samples (e.g., Connelly & Rapoff, 2006). In the current study, Cronbach’s α was .93 for the total score, indicating good reliability.
Data Analyses
Preliminary Analyses
Initially, descriptive statistics were performed to characterize the sample. Data were tested for normality, and statistical assumptions were inspected. Correlations, t tests, and one-way analyses of variance (ANOVAs) were conducted to examine associations among study variables and identify potential covariates. Pain intensity composite scores were computed by averaging general pain and worst pain intensity ratings.
Primary Analyses
To examine associations among optimism, fear of pain, pain catastrophizing, and functioning outcomes, linear regression analyses were performed. Covariates were accounted for in the first step of each regression. Bootstrapping, a non-parametric resampling technique to assess indirect effects, was performed to determine whether pain-related risk factors (fear of pain and pain catastrophizing) mediated the relation between optimism and functioning outcomes (disability and QOL) using published SPSS macros (Preacher & Hayes, 2004). A bootstrapping approach is recommended for smaller sample sizes that may not be normally distributed, rectifying the impact of asymmetrical sampling distributions on statistical power (Preacher & Hayes, 2004, 2008). The indirect effect was considered to be significantly different from zero at p < .05 when zero did not fall within the 95% confidence interval (95% CI; Preacher & Hayes, 2004).
Results
Preliminary and Descriptive Analyses
Descriptive statistics and intercorrelations between study variables are shown in Table I. Pain intensity and pain duration were entered as covariates in primary analyses. Interestingly, pain intensity was not significantly correlated with optimism and pain duration was not significantly correlated with fear of pain, catastrophizing, disability, or QOL. Significant positive associations emerged between fear of pain and catastrophizing, catastrophizing and disability, fear of pain and disability, and optimism and QOL. Significant negative correlations emerged between pain duration and optimism, fear of pain and optimism, catastrophizing and optimism, fear of pain and QOL, catastrophizing and QOL, optimism and disability, and disability and QOL. After performing ANOVAs and t tests, no additional variables were controlled for in subsequent analyses. Diagnostic analyses revealed that statistical assumptions were met for regressions.
Descriptives and Intercorrelations Among Study Variables
| Variable . | M (SD) . | Range . | Pain composite . | Pain duration . | PCS . | FOPQ . | YLOT . | FDI . |
|---|---|---|---|---|---|---|---|---|
| Pain composite | 7.20 (2.05) | 9.25 | – | |||||
| Pain duration (months) | 32.27 (37.51) | 177 | .02 | – | ||||
| Pain catastrophizing (PCS)a | 28.14 (9.71) | 47 | .44** | .02 | – | |||
| Fear of pain (FOPQ)b | 48.68 (19.69) | 88 | .46** | .14 | .74** | – | ||
| Optimism (YLOT)c | 11.04 (4.42) | 16 | −.25 | −.28* | −.42* | −.54** | – | |
| Functional disability (FDI)d | 25.47 (12.28) | 54 | .56** | −.03 | .47** | .47** | −.28* | – |
| Quality of life (PedsQL)e | 51.32 (21.07) | 85.87 | −.61** | .04 | −.60** | −.71** | .57** | −.73** |
| Variable . | M (SD) . | Range . | Pain composite . | Pain duration . | PCS . | FOPQ . | YLOT . | FDI . |
|---|---|---|---|---|---|---|---|---|
| Pain composite | 7.20 (2.05) | 9.25 | – | |||||
| Pain duration (months) | 32.27 (37.51) | 177 | .02 | – | ||||
| Pain catastrophizing (PCS)a | 28.14 (9.71) | 47 | .44** | .02 | – | |||
| Fear of pain (FOPQ)b | 48.68 (19.69) | 88 | .46** | .14 | .74** | – | ||
| Optimism (YLOT)c | 11.04 (4.42) | 16 | −.25 | −.28* | −.42* | −.54** | – | |
| Functional disability (FDI)d | 25.47 (12.28) | 54 | .56** | −.03 | .47** | .47** | −.28* | – |
| Quality of life (PedsQL)e | 51.32 (21.07) | 85.87 | −.61** | .04 | −.60** | −.71** | .57** | −.73** |
Note. *p < .05. **p < .001.
aPCS scores range from 0 to 52, with higher scores indicative of more catastrophizing.
bFOPQ scores range from 0 to 96, with higher scores indicative of greater fear of pain.
cYLOT optimism scores range from 0 to 18 (healthy sample mean [standard deviation] = 14.40 [3.59]), with higher scores indicative of greater optimism.
dFDI scores range from 0 to 60, with higher scores indicative of worse daily functioning.
ePedsQL total scores range from 0 to 100, with higher scores indicative of greater overall quality of life.
Descriptives and Intercorrelations Among Study Variables
| Variable . | M (SD) . | Range . | Pain composite . | Pain duration . | PCS . | FOPQ . | YLOT . | FDI . |
|---|---|---|---|---|---|---|---|---|
| Pain composite | 7.20 (2.05) | 9.25 | – | |||||
| Pain duration (months) | 32.27 (37.51) | 177 | .02 | – | ||||
| Pain catastrophizing (PCS)a | 28.14 (9.71) | 47 | .44** | .02 | – | |||
| Fear of pain (FOPQ)b | 48.68 (19.69) | 88 | .46** | .14 | .74** | – | ||
| Optimism (YLOT)c | 11.04 (4.42) | 16 | −.25 | −.28* | −.42* | −.54** | – | |
| Functional disability (FDI)d | 25.47 (12.28) | 54 | .56** | −.03 | .47** | .47** | −.28* | – |
| Quality of life (PedsQL)e | 51.32 (21.07) | 85.87 | −.61** | .04 | −.60** | −.71** | .57** | −.73** |
| Variable . | M (SD) . | Range . | Pain composite . | Pain duration . | PCS . | FOPQ . | YLOT . | FDI . |
|---|---|---|---|---|---|---|---|---|
| Pain composite | 7.20 (2.05) | 9.25 | – | |||||
| Pain duration (months) | 32.27 (37.51) | 177 | .02 | – | ||||
| Pain catastrophizing (PCS)a | 28.14 (9.71) | 47 | .44** | .02 | – | |||
| Fear of pain (FOPQ)b | 48.68 (19.69) | 88 | .46** | .14 | .74** | – | ||
| Optimism (YLOT)c | 11.04 (4.42) | 16 | −.25 | −.28* | −.42* | −.54** | – | |
| Functional disability (FDI)d | 25.47 (12.28) | 54 | .56** | −.03 | .47** | .47** | −.28* | – |
| Quality of life (PedsQL)e | 51.32 (21.07) | 85.87 | −.61** | .04 | −.60** | −.71** | .57** | −.73** |
Note. *p < .05. **p < .001.
aPCS scores range from 0 to 52, with higher scores indicative of more catastrophizing.
bFOPQ scores range from 0 to 96, with higher scores indicative of greater fear of pain.
cYLOT optimism scores range from 0 to 18 (healthy sample mean [standard deviation] = 14.40 [3.59]), with higher scores indicative of greater optimism.
dFDI scores range from 0 to 60, with higher scores indicative of worse daily functioning.
ePedsQL total scores range from 0 to 100, with higher scores indicative of greater overall quality of life.
Regression Analyses
The first aim of this study was to examine associations among fear of pain, catastrophizing, optimism, and functioning outcomes. When examining the associations between risk factors and functioning outcomes, catastrophizing was a significant predictor of disability, β = .281, t (51) = 2.31, p < .05, accounting for 6.5% of the variance, FΔ (1, 51) = 5.36, p < .05, and QOL, β = −.459, t (51) = −4.00, p < .001, accounting for 17.3% of the variance, FΔ (1, 51) = 15.96, p < .001. Furthermore, pain-related fear was a significant predictor of disability, β = .275, t (51) = 2.18, p < .05, accounting for 5.8% of the variance, FΔ (1, 51) = 4.73, p < .05, and QOL, β = −.608, t (51) = −5.72, p < .001, accounting for 28.3% of the variance, FΔ (1, 51) = 32.72, p < .001. Optimism was not a significant predictor of disability, β = −.174, t (51) = −1.42, p = .162, and only accounted for 2.6% of the variance in disability, FΔ (1, 51) = 2.014, p = .162. However, optimism was a significant predictor of QOL, β = .528, t (51) = 5.02, p < .001, accounting for 24% of the variance, FΔ (1, 51) = 25.22, p < .001. Finally, when examining the associations between optimism and risk factors, optimism was a significant predictor of pain-related fear, β = −.456, t (52) = −3.95, p < .001, accounting for 17.9%percent of the variance, FΔ (1, 52) = 15.60, p < .001, and catastrophizing, β = −.357, t (52) = −2.86, p < .05, accounting for 11% of the variance, FΔ (1, 52) = 8.19, p < .05.
Mediation Analyses
Four mediation analyses were conducted using nonparametric bootstrapping with 5,000 samples to generate 95% bias corrected CIs for indirect effects. Results indicated that neither fear of pain (95% CI: −0.78, 0.05) nor catastrophizing (95% CI: −0.63, 0.00) mediated the effect of optimism on disability. However, both fear of pain (95% CI: 0.38, 1.79) and catastrophizing (95% CI: 0.14, 1.21) each mediated the effect of optimism on child QOL, such that youths with higher optimism reported heightened QOL through decreased fear of pain and catastrophizing.
Discussion
Despite the prominence of risk-resilience models as theory-driven frameworks in the developmental and health psychology literatures, such models have not yet been applied to pediatric pain research. To provide a starting point to further work in this area, the primary aim of this study was applying a proposed model (Figure 1) to examine associations among pain-related risk factors, optimism, and functioning outcomes, and explore potential mechanisms that minimize risk and contribute to resilience.
Comparable with the extant literature, the sample consisted primarily of White, Not Hispanic/Latino, adolescent females with chronic pain accompanied by their mothers. However, the sample included more racial diversity relative to prior research, with almost one-third of youth identifying as Black or African–American, which is reflective of the multidisciplinary pain clinics’ patient populations in Atlanta, Georgia. The sample also exhibited mean values of independent and outcome variables that approximate those found in previous studies (Crombez et al., 2003; Gold et al., 2009; Simons et al., 2011). As expected, mean optimism scores in our population were lower than those found in a sample of healthy school children (Ey et al., 2005). Consistent with prior research (Crombez et al., 2003; Gold et al., 2009; Goodin & Bulls, 2013; Simons et al., 2011; Walker & Greene, 1991), preliminary results revealed that pain intensity was positively associated with pain-related fear, catastrophizing, and disability, and negatively associated with QOL. However, pain intensity was not associated with optimism. The nonsignificant association between optimism and pain intensity may be related to the previously mentioned controversy and mixed findings observed in the adult literature, indicative of the inconsistent effects of optimism on physical health indicators relative to mental health. However, it is also crucial to highlight that pain-related functioning can be targeted without impacting pain intensity. Psychological interventions that have received empirical support for improving functioning in adults and youth with pain, such as Acceptance and Commitment Therapy (Hayes, Strosahl, & Wilson, 1999), illustrate that such improvements occur through changing responses to pain rather than the pain itself (Vowles & Thompson, 2011). A non-significant association between optimism and pain has also been found in a sample of adolescents with sickle cell disease (Pence, Valrie, Gil, Redding-Lallinger, & Daeschner, 2007) and a sample of adults with chronic musculoskeletal pain (Wright et al., 2011). Optimism was positively associated with QOL and negatively associated with pain-related fear, catastrophizing, and disability. Given optimism’s positive impact on physical health and functioning in adult populations (Carver et al., 2010), as well as literature revealing optimism’s positive association with QOL among children and adolescents with cancer (Mannix et al., 2009; Williams et al., 2010), these findings were anticipated.
In terms of primary analyses, when controlling for pain intensity and duration of pain, pain-related fear and catastrophizing predicted poorer functioning (i.e., increased disability and reduced QOL), which is consistent with the literature. Interestingly, optimism did not predict disability, but as hypothesized, was a significant predictor of QOL. This significant finding is consistent with theories and data in the extant literature, suggesting that optimism is related to greater psychological and physical well-being (Alarcon, Bowling, & Khazon, 2013; Goodin & Bulls, 2013; Ramírez-Maestre & Esteve, 2013). Furthermore, consistent with Sturgeon and Zautra’s model, optimism also predicted lower catastrophizing and fear of pain. These results suggest that optimism may also be an important resilience factor for youth with chronic pain. Optimism may have emerged as a predictor of QOL and not disability because optimism and QOL are not pain-specific constructs. Thus, generalized positive expectancies are not sufficient in counteracting the adverse impact of pain intensity on disability, but do contribute to greater well-being beyond pain intensity. Selecting resilience constructs that are pain-specific, such as positive pain expectancies, may have produced alternative findings.
The mediation analyses partially supported the applied risk-resilience model, revealing that catastrophizing and fear of pain each mediated the optimism–QOL relation, but had no effect on the optimism–disability relation. A nonsignificant mediation for the optimism–disability relation may be a result of the nonsignificant association initially found between optimism and disability. Consistent with prior research (Pulvers & Hood, 2013) and Sturgeon and Zautra’s model, results showed that optimism contributes to better functioning (e.g., enhanced well-being) through lower pain-related fear and catastrophizing. As prior research has primarily used healthy adult samples (Hanssen et al., 2013; Hood et al., 2012), our findings are the first to suggest that risk-resilience mechanisms might function in similar ways in pediatric chronic pain.
One distinct difference between the current study and prior research is that previous studies with adults have only established catastrophizing as a mediator in the relation between optimism and pain perception. The current study uniquely examined the mediating effect of both pain-related fear and catastrophizing on the relation between optimism and prominent functioning outcomes. Optimism may indeed provide individuals with flexible coping resources that facilitate better adjustment to pain (Ramírez-Maestre & Esteve, 2013).
When interpreting the results, some caveats should be considered. First, this clinic-based sample may not be representative of the general population of youth living with chronic pain, as participants were seeking or receiving treatment for their pain. However, this sample is comparable with prior research recruiting from outpatient pain clinics. Participants’ frequency of visits to the pain clinic was also not assessed. Returning participants may have lower optimism relative to new visit participants, as they have previously received recommendations and treatment but may continue to experience significant pain and limited functioning. Furthermore, it is impossible to determine any causal relations or the direction of influence among optimism, pain-related fear, catastrophizing, functioning, and QOL given the cross-sectional design. Longitudinal or experimental studies are needed to better understand the mechanisms and causal links associated with these variables. As optimism has not previously been explored in the pediatric pain population, it will be particularly important to determine the consistency and stability of optimism self-report responses across time as the pain experience changes. Recent research with adults has provided support for the causal link between optimism and experimental pain perception, and the meditational effect of situational pain catastrophizing, through the experimental manipulation of optimism (Hanssen et al., 2013). This potential modifiability of optimism proves promising for future experimental work with chronic pain patients.
Second, this study solely relied on self-report data. It will be imperative for future studies to decrease potential response biases by including parent reports, health care professional perceptions, and behavioral measures. Furthermore, shared method variance may have inflated associations between predictor and outcome variables in this study, as all variables were assessed using self-reports. Consistent with this concern of shared method variance, in a meta-analysis evaluating optimism’s impact on physical health, Rasmussen & Scheier (2009) revealed that the mean effect size for studies using subjective measures of physical health was higher compared with those assessing physical health objectively. Additionally, this study did not use a counterbalanced design. Thus, the order of completing measures may have influenced self-report responses. Although the sample size is similar to most other pediatric psychology research, a larger sample size would have enabled more advanced statistical analyses (e.g., structural equation modeling). Future studies with larger samples should account for pain and psychological diagnoses, family history of pain, and number of multidisciplinary pain clinic visits as potential covariates.
Although the most prominent risk factors studied in chronic pain are arguably fear of pain and pain catastrophizing, this study did not account for other factors that might influence these constructs, such as anxiety, anxiety sensitivity, and depression. Similarly, although optimism has been most prevalently explored in health psychology as well as adult pain sensitivity models, future research should examine other potential resilience factors in pediatric chronic pain, such as acceptance and positive affect (Pulvers & Hood, 2013), mindfulness (Petter, McGrath, Chambers, & Dick, 2014), self-efficacy (Carpino, Segal, Logan, Lebel, & Simons, 2014), racial/ethnic identification and cultural and community resources (Koinis-Mitchell et al., 2012), and family factors (Palermo, Valrie, & Karlson, 2014). Such research will provide the foundation to explore how resilience factors impact coping strategies, cognitive processes, cortical involvement, and ultimately, adjustment to pediatric pain.
Better understanding of these resilience mechanisms will be useful in developing more effective treatment approaches to chronic pain. Optimism training interventions can potentially be applied to youth with chronic pain. For example, positive future thinking techniques and best possible self exercises encourage individuals to visualize or write about an optimal life and optimal self, which fosters flexible and realistic positive future expectancies. Integrating optimism training into current intervention approaches might increase positive cognitions and highlight strengths. Such interventions may not only counteract maladaptive cognitive processes related to pain and avoidance or withdrawal behaviors but also expand and cultivate psychological resources. Individuals may no longer feel confined or handicapped by their pain, but rather become less attentive to pain, gain acceptance, and engage in benefit finding during pain episodes. Promoting optimism might minimize the impact of adversity and may enhance perseverance and adaptive coping to seek out positive resources, such as social support or continued engagement in valued activities. Resilience-based interventions can foster key strengths, such as mindfulness, self-efficacy, pain-specific optimism, social connectedness, and problem-solving skills, which all promote behavioral engagement and may contribute to a healthier lifestyle and better treatment adherence. In closing, the current study is the first to examine resilience in pediatric chronic pain; it is hoped that these findings will inform new avenues for improving functioning and QOL in youth with chronic pain.
Acknowledgments
This research is the thesis project of the first author under the supervision of the second author at Georgia State University.
Funding
This research was supported by an American Psychological Association, Division 54 (Society of Pediatric Psychology) Mary Jo Kupst Trainee Grant for Research in Resilience to the first author.
Conflicts of interest: None declared.