-
PDF
- Split View
-
Views
-
Cite
Cite
Margaret L Kerr, Kerrie A Fanning, Tuyen Huynh, Inés Botto, Christina N Kim, Parents’ Self-Reported Psychological Impacts of COVID-19: Associations With Parental Burnout, Child Behavior, and Income, Journal of Pediatric Psychology, Volume 46, Issue 10, November-December 2021, Pages 1162–1171, https://doi.org/10.1093/jpepsy/jsab089
Close - Share Icon Share
Abstract
The current study investigates associations between parents’ perceived coronavirus disease 2019 (COVID-19) psychological impacts and experiences of parental burnout, children’s behaviors, and income.
Data were collected during an online survey of parents’ (N = 1000) pandemic experiences in April 2020. Parents (M = 36.5 years old, SD = 6.0; 82.1% White) with at least one child 12 years or younger reported on measures of mental health, perceived COVID-19 impacts, parental burnout, and perceived increases in children’s stress and positive behaviors.
Path model analyses revealed that parents who perceived increased psychological impacts from COVID-19 reported higher levels of parental burnout, greater increases in children’s stress behaviors, and less positive behavior in children. Additionally, there were significant indirect effects of parental burnout on the link between COVID-19 psychological impacts and children’s behaviors. Finally, family income moderated associations between psychological impacts and children’s stress behaviors, such that the association was stronger for families with lower income.
These results suggest parents’ perceptions of how the COVID-19 pandemic has impacted their mental health has implications for parent and child well-being, with stronger associations for low-income families. Given the potential for spillover effects between parents and children, promoting family well-being through practice and policy initiatives is crucial, including providing financial and caregiving relief for parents, and mental and behavioral health support for families.
Introduction
The coronavirus disease 2019 (COVID-19) pandemic’s pervasive impact persists worldwide, with the United States reporting over 33 million cases and nearly 600,000 deaths as of June 2021 (World Health Organization, 2021). Along with physical health impacts, the pandemic disrupted families’ lives and strained mental health, with disproportionate impacts for low-income individuals (Park et al., 2020) and families with children (American Psychological Association, 2020). Family stress theory (FST; McCubbin & Patterson, 1983) articulates the intersections among family stress, resources, and perceptions and its consequences for family adaptation. Indeed, studies prior to COVID-19 have evidenced this in numerous contexts (Boss et al., 2017). COVID-19 scholarship applying FST emphasizes interactions between pandemic stressors (e.g., job instability), families’ pre-pandemic resources (e.g., income), and families’ perceptions of the pandemic (Wu & Xu, 2020), with empirical support from emerging studies (e.g., Wu et al., 2021). Using this lens, the current study examines associations between parents’ perceived psychological impacts due to COVID-19, parental burnout, and child behaviors during COVID-19, including variations by income.
The COVID-19 pandemic created and magnified sources of family stress, including psychological distress (Russell et al., 2020; Twenge & Joiner, 2020), job instability (Park et al., 2020), and food insecurity (Karpman et al., 2020; Patrick et al., 2020). These stressors hindered family well-being and functioning, even among families who were not facing these challenges pre-pandemic (e.g., American Psychological Association, 2020). Across multiple studies, parents identified educational interruptions (e.g., virtual learning), school closures, and worries about children’s development as significant sources of stress (American Psychological Association, 2020; Hiraoka & Tomoda, 2020), with implications for parents’ mental health (Prime et al., 2020). A widespread crisis like the COVID-19 pandemic is likely to have intergenerational impacts on families, given well-documented intergenerational associations between parental distress and psychopathology and child well-being (e.g., Fisher, 2017; Goodman et al., 2011). In addition to impacts to parent–child dynamics and parental mental health, many children experienced changes in primary caregivers’ routines (e.g., working from home), separation from peers, and continued uncertainty about returning to activities (e.g., school) (Patrick et al., 2020). Child stress often manifests through increased externalizing and internalizing behaviors, which are often seen as challenging to parents (Neece et al., 2012). Indeed, children are exhibiting higher rates of clinginess, distraction, irritability, and fear due to the pandemic (Jiao et al., 2020).
Parental burnout—characterized by overwhelming exhaustion, feelings of parental inadequacy, and emotional distancing from one’s children—results from a chronic imbalance of parenting risks and resources and typically occurs in 5–20% of parents (Griffith, 2020; Roskam et al., 2018). Preliminary evidence, however, suggests that parental burnout may be exacerbated by the COVID-19 pandemic, as it introduced additional parenting stressors (e.g., increased caregiving), while simultaneously reducing resources (e.g., family support), resulting in heightened parenting stress and exhaustion (e.g., Aguiar et al., 2021; Griffith, 2020; Marchetti et al., 2020). Parental burnout has detrimental consequences for parents and children—with associations between poorer parental mental and physical health and higher rates of child maltreatment (Mikolajczak et al., 2018; Roskam et al., 2018). Examining parental burnout poses an important area of study given changes in parents’ responsibilities, stress, and resources due to the COVID-19 pandemic.
Parents experiencing increased psychological symptoms (e.g., depression, anxiety) and parental burnout are more likely to engage in negative parenting behaviors (e.g., Fisher, 2017; Goodman et al., 2011), which is associated with negative child outcomes, including child psychopathology (e.g., Shaw & Starr, 2019). Due to the COVID-19 pandemic, increased demands on parents combined with inaccessible resources may increase use of maladaptive parenting behaviors, impacting child well-being (Wu & Xu, 2020). Past research in war and disaster contexts documents that reduced parental mental health strain—even within stressful contexts—is associated with more positive behaviors and fewer long-term emotional and behavioral disorders among children (e.g., Masten & Motti-Stefanidi, 2020). Emerging evidence suggests this may be true for the COVID-19 pandemic as well (Spinelli et al., 2020).
Importantly, due to job loss, working from home, and reduced access to paid leave, low-income families may be especially vulnerable to the pandemic’s impacts (Gassman-Pines et al., 2020). Early in the pandemic, more low-income compared to high-income families reported struggling to meet basic needs and arrange childcare (Karpman et al., 2020) and were less likely to receive pandemic-specific governmental aid (Ananat et al., 2020). These COVID-19-related stressors likely exacerbated prior distress and hardship for low-income families (Gassman-Pines et al., 2020). Indeed, intersections between financial resources and family stress using FST are well-documented (e.g., Boss et al., 2017). During the COVID-19 pandemic, financial strain may amplify the impact of parents’ COVID-19 psychological impacts on experiences of parental burnout and children’s behaviors, with more negative outcomes for low-income families.
Emerging research documents increased distress for parents since the start of the COVID-19 pandemic (American Psychological Association, 2020) with downstream impacts on children, which may differentially impact low-income families (Karpman et al., 2020). Based on FST, this study examines parents’ perceptions of COVID-19 impacts to their psychological health and associations with parental burnout, children’s behaviors, and differences by income. Controlling for depression and anxiety symptoms, we predicted that parents’ reports of how COVID-19 impacted their psychological health would be positively associated with children’s stress behaviors (Hypothesis 1a) and negatively with children’s positive behaviors (Hypothesis 1b). Second, we predicted that parental burnout would be positively associated with children’s stress behaviors (Hypothesis 2a) and negatively with children’s positive behaviors (Hypothesis 2b), controlling for parents’ mental health. Third, we predicted that parental burnout would partially explain cross-sectional associations between parents’ perceived COVID-19 psychological impacts and children’s behaviors (Hypothesis 3). Lastly, we predicted that family income would moderate the links between parents’ COVID-19 psychological impacts with parental burnout and children’s behaviors (Hypothesis 4), with stronger links for lower-income families.
Methods
Participants and Procedure
Data were collected from parents with at least one child 12 years old or younger through a 30–45 min online-survey of parents’ COVID-19 experiences in April 2020. Parents were recruited through social networking sites (e.g., Facebook) and university-affiliated listservs. The study was deemed exempt by University of Wisconsin-Madison IRB, #2020-0557, and all participants provided informed consent. Parents received a $15 gift card for participation.
Because online studies have the potential for “bot” or spam responses, researchers completed a rigorous verification process to validate all responses, including verifying demographic characteristics through email, evaluating open-ended responses, and matching participant’s IP address and zip code. Out of 1,588 completed responses, 537 were determined as “bots” or spam and were removed. Subsequently, 42 additional responses were removed due to participants completing the survey in less than 10 min or missing two or more attention checks, leaving 1,009 valid responses.
Parents primarily identified as women (88.7%), 10.9% as men, and 0.4% as other genders or gender non-conforming. Parents ranged from 21 to 64 years old (M = 36.5 years, SD = 6.0), had two children on average (M = 2.1 children, SD = 1.0, range = 1–9), and 16.7% of parents were caring for a child with an illness or disability. The majority identified as White (82.1%), 5.9% as Asian/Asian American, 2.8% as Black/African American, 2.3% as Hispanic/Latinx/Spanish origin, 0.4% as American Indian/Alaskan Native, 5.3% as more than one race, and 0.8% as other. The majority of parents were Wisconsin residents (80.2%), while the remaining were from other U.S. states (e.g., 5.2% CA, 2.0% NY, 1.3% MI). Most parents were married (82.1%) and most (78.5%) reported household income above $50,000 a year, with 20.8% of families living at or below 200% of the federal poverty level. Thirty percent of families utilized at least one form of public assistance, such as Medicare or Medicaid, Social Security Income, or Unemployment benefits. Most parents (74.9%) had a bachelor’s degree or higher. Parents with more than one child reported on their child with the most recent birthday (M = 6.17 years, SD = 3.67, range 0–17). Nine participants who reported on children over 17 years were removed from analyses, resulting in a final sample size of 1,000.
Measures
Several measures were created or modified for this study, given a lack of COVID-19 pandemic-specific measures at the time of data collection. When applicable, modifications are described and psychometric information is provided. In-depth descriptive statistics for the mental health, parental burnout, and child stress measures are presented in Kerr et al. (2021).
Parental Anxiety and Depression Symptoms
Parents’ anxiety and depression symptoms were assessed using the General Anxiety Scale 7-Item (GAD-7; Spitzer et al., 2006; α = .92) and Patient Health Questionnaire 8-Item (PHQ-8; Kroenke et al., 2009; α = .88), respectively. Both measures use a 4-point scale (0 = not at all to 3 = nearly every day), with higher total scores reflecting greater symptom severity. These measures are widely used in clinical and research settings as screening tools for depression- and anxiety-related disorders (Kroenke et al., 2009; Löwe et al., 2008). Scores of 10 or above indicate clinically significant levels of depression or anxiety symptoms. In the current sample, 31.0% and 30.8% of parents’ scores fell within the borderline to severe depression and anxiety categories, respectively.
COVID-19 Psychological Impacts
The psychological impacts scale of the Coronavirus Impacts Questionnaire (Conway et al., 2020; α = .83) was used to assess parents’ perceived psychological impacts due to COVID-19. To be consistent with other measures and to reduce participant burden, the original 7-point scale (not true of me at all to very to true of me) was converted to a 5-point scale (strongly disagree to strongly agree). The scale’s 3 items include: “I have become depressed because of the Coronavirus [COVID-19],” “The Coronavirus (COVID-19) outbreak has impacted my mental health negatively,” and “The Coronavirus (COVID-19) pandemic has NOT made me feel any worse than I did before” (reverse scored). The items were summed, with higher scores indicating greater COVID-19 psychological impacts.
Parental Burnout
To measure parental burnout, a modified version of the Parental Burnout Assessment (Roskam et al., 2018; α = .84) was used, which is similar to recent validated adaptations (Aunola et al., 2021). Respondents ranked five items (e.g., “I feel completely run down by my role as a parent” or “I’m no longer able to show my child(ren) how much I love them”) on a 7-point scale (0 = strongly disagree to 6 = strongly agree). The measure and response scale were modified to capture experiences of parental burnout specific to the COVID-19 pandemic. A sum score was created, with higher parental burnout reflected by higher scores.
Child Stress
A modified version of the Parent-Report of Post-Traumatic Stress (PROPS; Greenwald & Rubin, 1999; α = .76) captured children’s stress since the start of the pandemic. The original PROPS consists of 32 items reflecting Post-Traumatic Stress Disorder symptoms in children (e.g., mood swings, nightmares) as described in the Diagnostic and Statistical Manual of Mental Disorders, 4th edition (American Psychiatric Association, 1994). A description of the modifications was reported in Kerr et al. (2021). Previous studies incorporating the full PROPS measure with community-based samples have reported average scores ranging from 6.0 to 18.3 (Chung et al., 2019; Greenwald & Rubin, 1999) out of a possible score range of 0–60. The clinical cutoff in the full scale is 16; however, due to scale modifications, we were unable to compute a comparable cutoff in the current study.
Children’s Positive Behaviors
Using a subset of children’s health questions from the National Survey of Children's Health (Child and Adolescent Health Measurement Initiative, 2018; α = 73), parents reported on the frequency of their child’s engagement in positive or adaptive behaviors. Rating from never (0) to always (4), the four questions ask about children’s displays of affection toward the parent, smiles and laughter, and curiosity in new things, and their ability to bounce-back after facing challenges over the previous 2 weeks. Higher sum scores indicate children’s greater engagement in these behaviors.
Family Income
To capture family income prior to any COVID-19-related changes, parents were asked to report on household income from all sources (before taxes). Income categories were: 0 = Less than $10,000, 1 = $10,001 to $30,000, 2 = $30,001 to $50,000, 3 = $50,001 to $70,000, 4 = $70,001 to $90,000, 5 = $90,001 to $110,000, 6 = Over $110,001. We used this as a continuous variable in our analyses, which was normally distributed (skew and kurtosis less than ±1).
Results
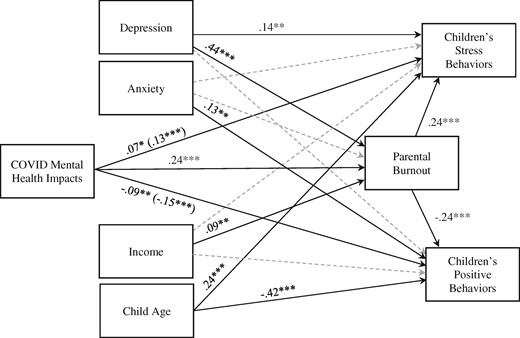
All hypotheses were tested using path models in the R package, Lavaan (Rosseel, 2012). RMSEA, TLI, and CFI fit indices are reported for each model (Hu & Bentler, 1999). Path Model 1 tests Hypotheses 1–3 (see Figure 1) and Path Model 2 tests Hypothesis 4. Preliminary analyses indicated a normal distribution for all key variables, with a skew and kurtosis less than ±2. Focal child age correlated with child stress behaviors, r = .23, p < .001, and child positive behaviors, r = −.41, p < .001. There were small negative correlations between income and parents’ anxiety, r = −.13, p = < .001, depression symptoms, r = −.15, p < .001, and child stress behaviors, r = −.07, p = .03. Descriptive statistics and correlations are presented in Table I.
Path model 1 depicting direct and indirect associations of parents’ psychological impacts of COVID-19 on perceptions of children’s behaviors.
Note. Standardized path estimates are presented. Dashed lines indicate non-significant paths. Values in parentheses represent total effects.
*p < .05. **p < .01, ***p < .001.
Indirect effect of COVID-19 psychological impacts on perception of children’s stress behavior through parental burnout: β = .06***, p < .001.
Indirect effect of COVID-19 psychological impacts on perception of children’s positive behavior through parental burnout: β = −.06***, p < .001.
Means, Standard Deviations, and Correlations With Confidence Intervals
| Variable . | Range . | M . | SD . | 1 . | 2 . | 3 . | 4 . | 5 . | 6 . | 7 . |
|---|---|---|---|---|---|---|---|---|---|---|
| 1. Child age | 0–17 | 6.17 | 3.67 | |||||||
| 2. Income | 0–6 | 4.16 | 1.77 | −.00 | ||||||
| 3. Anxiety symptoms | 0–21 | 7.46 | 5.55 | .02 | −.13** | |||||
| 4. Depression symptoms | 0–24 | 7.44 | 5.38 | .04 | −.15** | .77** | ||||
| 5. C19 mental health | 3–15 | 9.95 | 3.20 | .02 | −.05 | .54** | .54** | |||
| 6. Parental burnout | 0–30 | 11.10 | 6.63 | −.06 | .01 | .46** | .56** | .47** | ||
| 7. C stress behaviors | 0–17 | 3.89 | 3.08 | .23** | −.07* | .30** | .35** | .28** | .35** | |
| 8. C positive behaviors | 1–5 | 3.88 | 0.63 | −.41** | .05 | −.12** | −.19** | −.20** | −.24** | −.34** |
| Variable . | Range . | M . | SD . | 1 . | 2 . | 3 . | 4 . | 5 . | 6 . | 7 . |
|---|---|---|---|---|---|---|---|---|---|---|
| 1. Child age | 0–17 | 6.17 | 3.67 | |||||||
| 2. Income | 0–6 | 4.16 | 1.77 | −.00 | ||||||
| 3. Anxiety symptoms | 0–21 | 7.46 | 5.55 | .02 | −.13** | |||||
| 4. Depression symptoms | 0–24 | 7.44 | 5.38 | .04 | −.15** | .77** | ||||
| 5. C19 mental health | 3–15 | 9.95 | 3.20 | .02 | −.05 | .54** | .54** | |||
| 6. Parental burnout | 0–30 | 11.10 | 6.63 | −.06 | .01 | .46** | .56** | .47** | ||
| 7. C stress behaviors | 0–17 | 3.89 | 3.08 | .23** | −.07* | .30** | .35** | .28** | .35** | |
| 8. C positive behaviors | 1–5 | 3.88 | 0.63 | −.41** | .05 | −.12** | −.19** | −.20** | −.24** | −.34** |
Note. M and SD are used to represent mean and standard deviation, respectively. C = Child; C19 = COVID-19.
p < .05;
p < .001.
Means, Standard Deviations, and Correlations With Confidence Intervals
| Variable . | Range . | M . | SD . | 1 . | 2 . | 3 . | 4 . | 5 . | 6 . | 7 . |
|---|---|---|---|---|---|---|---|---|---|---|
| 1. Child age | 0–17 | 6.17 | 3.67 | |||||||
| 2. Income | 0–6 | 4.16 | 1.77 | −.00 | ||||||
| 3. Anxiety symptoms | 0–21 | 7.46 | 5.55 | .02 | −.13** | |||||
| 4. Depression symptoms | 0–24 | 7.44 | 5.38 | .04 | −.15** | .77** | ||||
| 5. C19 mental health | 3–15 | 9.95 | 3.20 | .02 | −.05 | .54** | .54** | |||
| 6. Parental burnout | 0–30 | 11.10 | 6.63 | −.06 | .01 | .46** | .56** | .47** | ||
| 7. C stress behaviors | 0–17 | 3.89 | 3.08 | .23** | −.07* | .30** | .35** | .28** | .35** | |
| 8. C positive behaviors | 1–5 | 3.88 | 0.63 | −.41** | .05 | −.12** | −.19** | −.20** | −.24** | −.34** |
| Variable . | Range . | M . | SD . | 1 . | 2 . | 3 . | 4 . | 5 . | 6 . | 7 . |
|---|---|---|---|---|---|---|---|---|---|---|
| 1. Child age | 0–17 | 6.17 | 3.67 | |||||||
| 2. Income | 0–6 | 4.16 | 1.77 | −.00 | ||||||
| 3. Anxiety symptoms | 0–21 | 7.46 | 5.55 | .02 | −.13** | |||||
| 4. Depression symptoms | 0–24 | 7.44 | 5.38 | .04 | −.15** | .77** | ||||
| 5. C19 mental health | 3–15 | 9.95 | 3.20 | .02 | −.05 | .54** | .54** | |||
| 6. Parental burnout | 0–30 | 11.10 | 6.63 | −.06 | .01 | .46** | .56** | .47** | ||
| 7. C stress behaviors | 0–17 | 3.89 | 3.08 | .23** | −.07* | .30** | .35** | .28** | .35** | |
| 8. C positive behaviors | 1–5 | 3.88 | 0.63 | −.41** | .05 | −.12** | −.19** | −.20** | −.24** | −.34** |
Note. M and SD are used to represent mean and standard deviation, respectively. C = Child; C19 = COVID-19.
p < .05;
p < .001.
We controlled for parents’ depression and anxiety symptoms to account for known bias in depressed parents’ reports of children (e.g., Madsen et al., 2020); and to isolate the effects of parents’ psychological impacts specific to COVID-19, above and beyond general or pre-existing depression and anxiety symptoms. Income was a covariate in Path Model 1 and a moderator in Path Model 2. Focal child age was a covariate in associations with child outcomes. Because focal child age was randomized by children’s most recent birthdays and specific to the child behavior variables, it did not reflect a meaningful covariate for parental burnout. As such, the path between child age and parental burnout was set to zero. Number of children and marital/partner status were considered as covariates, but when included in the models they did not substantially change the coefficients and worsened model fit so they were not retained in final analyses.
Path Model 1
Our first model tested main effects and indirect associations between COVID-19 psychological impacts and child behaviors (see Figure 1), resulting in adequate fit, with CFI and TLI values of .992 and .967, respectively, and an RMSEA value of .039, 90% CI [.012, .067]. As predicted in Hypothesis 1, after controlling for parents’ depression and anxiety symptoms, family income, and focal child age, COVID-19 psychological impacts were positively associated with parents’ perceptions of increases in their children’s stress behaviors, B = .07, SE = .03, p = .04, and negatively associated with children’s positive behaviors, B = −.02, SE = .01, p = .006. Hypothesis 2 was also supported: After controlling for covariates, parental burnout was positively associated with increases in children’s stress behaviors, B = .11, SE = .02, p < .001, and negatively associated with children’s positive behaviors, B = −.02, SE = .003, p < .001.
For Hypothesis 3, results revealed that COVID-19 psychological impacts were positively associated with parental burnout, B = .49, SE = .06, p < .001. There were significant indirect effects of parental burnout for children’s stress behaviors, B = .05, SE = .01, p < .001 and children’s positive behaviors, B = −.01, SE = .002, p < .001. In other words, parental burnout explained a significant amount of variance in the associations between parents’ COVID-19 psychological impacts and children’s behavior. Prior to controlling for parental burnout, the total effect of parents’ COVID-19 psychological impacts on children’s stress and positive behaviors were, B = .12, SE = .03, p < .001, and B = −.03, SE = .01, p < .001, respectively.
To rule out the reverse model, we also tested whether parental burnout served as an indirect link between child stress and positive behaviors and parents’ COVID-19 psychological impacts. While the direct and indirect paths were still significant, compared to the hypothesized model all standardized effects were lower and the model showed worse fit (CFI = 0.811, TLI = 0.539, RMSEA = 0.173), so this model was rejected.
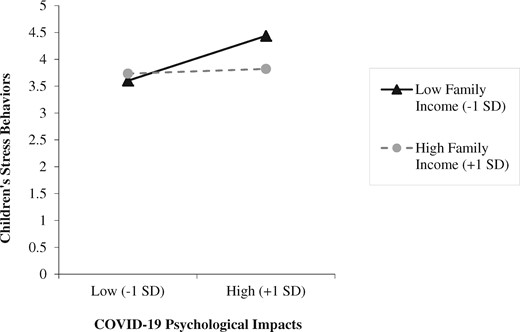
Path Model 2
In the second model, interaction terms with family income were added (see Table II). Fit indices showed an adequate fit to the data; CFI and TLI values of .993 and .969, respectively, and an RMSEA value of .035, 90% CI [.008, .061]. As predicted in Hypothesis 4, after controlling for parents’ depression and anxiety symptoms and focal child age, income significantly moderated associations between parents’ COVID-19 psychological impacts and children’s stress behaviors, B = −.03, SE = .02, p = .028. Simple slope analyses revealed that the positive association was only significant at lower-income levels (−1 SD), b = .13, t (985) = 4.12, p < .001 (higher income (+1 SD): b = .01, t (985) = 0.43, p = .67) (see Figure 2). Contrary to our predictions, income did not moderate associations between parents’ COVID-19 psychological impacts and parental burnout or children’s positive behaviors (see Table II).
Interaction between COVID-19 psychological impacts and family income on children’s stress behaviors.
Significant interaction between parents’ self-reported psychological impacts of COVID-19 and family income on children’s stress behaviors. The positive association between COVID-19 impacts and children’s stress is only significant for families who reported low (−1 SD) income, t(985) = 4.12, p <.001.
Standardized and Unstandardized Parameter Estimates From Path Analysis Models
| . | Path model 1 . | Path model 2 . | ||
|---|---|---|---|---|
| Std. est. | Estimate (SE) | Std. est. | Estimate (SE) | |
| Child stress behaviors | ||||
| COVID-19 impacts | 0.07 | 0.07(0.03)* | 0.08 | 0.07(0.03)* |
| Parental burnout | 0.24 | 0.11(0.02)*** | 0.23 | 0.11(0.02)*** |
| Depressive symptoms | 0.14 | 0.08(0.03)** | 0.14 | 0.08(0.03)** |
| Anxiety symptoms | 0.03 | 0.02(0.03) | 0.03 | 0.02(0.03) |
| Income | −0.04 | −0.07(0.05) | −0.04 | −0.07(0.05) |
| Child age | 0.24 | 0.20(0.02)*** | 0.24 | 0.20(0.02)*** |
| C19 Impacts × Income | −0.06 | −0.03(0.02)* | ||
| Child positive behavior | ||||
| COVID-19 impacts | −0.09 | −0.02(0.01)** | −0.10 | −0.02(0.01)** |
| Parental burnout | −0.24 | −0.02(0.00)*** | −0.24 | −0.02(0.00)*** |
| Depressive symptoms | −0.08 | −0.01(0.01) | −0.08 | −0.01(0.01) |
| Anxiety symptoms | 0.13 | 0.01(0.01)** | 0.13 | 0.01(0.01)** |
| Income | 0.05 | 0.02(0.01) | 0.05 | 0.02(0.01) |
| Child age | −0.42 | −0.07(0.01)*** | −0.42 | −0.07(0.01)*** |
| C19 Impacts × Income | 0.01 | 0.00(0.00) | ||
| Parental burnout | ||||
| COVID-19 impacts | 0.24 | 0.49(0.06)*** | 0.24 | 0.50(0.06)*** |
| Depressive symptoms | 0.44 | 0.54(0.05)*** | 0.43 | 0.53(0.05)*** |
| Anxiety symptoms | 0.01 | 0.01(0.05) | 0.02 | 0.02(0.05) |
| Income | 0.09 | 0.32(0.10)*** | 0.09 | 0.32(0.10)*** |
| C19 Impacts × Income | −0.01 | −0.02(0.03) | ||
| Indirect effects | ||||
| C19 Impacts → Burnout → C Stress | 0.06 | 0.05(0.01)*** | ||
| C19 Impacts → Burnout → C Pos Beh | −0.06 | −0.01(0.00)*** | ||
| Total effects | ||||
| C19 Impacts → C Stress | 0.13 | 0.12(0.03)*** | ||
| C19 Impacts → C Pos Beh | −0.15 | −0.03(0.01)*** | ||
| Fit indices | ||||
| CFI | 0.992 | 0.993 | ||
| TLI | 0.967 | 0.969 | ||
| RMSEA | 0.039 | 0.035 | ||
| . | Path model 1 . | Path model 2 . | ||
|---|---|---|---|---|
| Std. est. | Estimate (SE) | Std. est. | Estimate (SE) | |
| Child stress behaviors | ||||
| COVID-19 impacts | 0.07 | 0.07(0.03)* | 0.08 | 0.07(0.03)* |
| Parental burnout | 0.24 | 0.11(0.02)*** | 0.23 | 0.11(0.02)*** |
| Depressive symptoms | 0.14 | 0.08(0.03)** | 0.14 | 0.08(0.03)** |
| Anxiety symptoms | 0.03 | 0.02(0.03) | 0.03 | 0.02(0.03) |
| Income | −0.04 | −0.07(0.05) | −0.04 | −0.07(0.05) |
| Child age | 0.24 | 0.20(0.02)*** | 0.24 | 0.20(0.02)*** |
| C19 Impacts × Income | −0.06 | −0.03(0.02)* | ||
| Child positive behavior | ||||
| COVID-19 impacts | −0.09 | −0.02(0.01)** | −0.10 | −0.02(0.01)** |
| Parental burnout | −0.24 | −0.02(0.00)*** | −0.24 | −0.02(0.00)*** |
| Depressive symptoms | −0.08 | −0.01(0.01) | −0.08 | −0.01(0.01) |
| Anxiety symptoms | 0.13 | 0.01(0.01)** | 0.13 | 0.01(0.01)** |
| Income | 0.05 | 0.02(0.01) | 0.05 | 0.02(0.01) |
| Child age | −0.42 | −0.07(0.01)*** | −0.42 | −0.07(0.01)*** |
| C19 Impacts × Income | 0.01 | 0.00(0.00) | ||
| Parental burnout | ||||
| COVID-19 impacts | 0.24 | 0.49(0.06)*** | 0.24 | 0.50(0.06)*** |
| Depressive symptoms | 0.44 | 0.54(0.05)*** | 0.43 | 0.53(0.05)*** |
| Anxiety symptoms | 0.01 | 0.01(0.05) | 0.02 | 0.02(0.05) |
| Income | 0.09 | 0.32(0.10)*** | 0.09 | 0.32(0.10)*** |
| C19 Impacts × Income | −0.01 | −0.02(0.03) | ||
| Indirect effects | ||||
| C19 Impacts → Burnout → C Stress | 0.06 | 0.05(0.01)*** | ||
| C19 Impacts → Burnout → C Pos Beh | −0.06 | −0.01(0.00)*** | ||
| Total effects | ||||
| C19 Impacts → C Stress | 0.13 | 0.12(0.03)*** | ||
| C19 Impacts → C Pos Beh | −0.15 | −0.03(0.01)*** | ||
| Fit indices | ||||
| CFI | 0.992 | 0.993 | ||
| TLI | 0.967 | 0.969 | ||
| RMSEA | 0.039 | 0.035 | ||
Note. C Pos Beh = child positive behavior; C Stress = child stress; C19 Impacts = COVID-19 psychological impacts.
p< .05;
p < .01;
p< .001.
Standardized and Unstandardized Parameter Estimates From Path Analysis Models
| . | Path model 1 . | Path model 2 . | ||
|---|---|---|---|---|
| Std. est. | Estimate (SE) | Std. est. | Estimate (SE) | |
| Child stress behaviors | ||||
| COVID-19 impacts | 0.07 | 0.07(0.03)* | 0.08 | 0.07(0.03)* |
| Parental burnout | 0.24 | 0.11(0.02)*** | 0.23 | 0.11(0.02)*** |
| Depressive symptoms | 0.14 | 0.08(0.03)** | 0.14 | 0.08(0.03)** |
| Anxiety symptoms | 0.03 | 0.02(0.03) | 0.03 | 0.02(0.03) |
| Income | −0.04 | −0.07(0.05) | −0.04 | −0.07(0.05) |
| Child age | 0.24 | 0.20(0.02)*** | 0.24 | 0.20(0.02)*** |
| C19 Impacts × Income | −0.06 | −0.03(0.02)* | ||
| Child positive behavior | ||||
| COVID-19 impacts | −0.09 | −0.02(0.01)** | −0.10 | −0.02(0.01)** |
| Parental burnout | −0.24 | −0.02(0.00)*** | −0.24 | −0.02(0.00)*** |
| Depressive symptoms | −0.08 | −0.01(0.01) | −0.08 | −0.01(0.01) |
| Anxiety symptoms | 0.13 | 0.01(0.01)** | 0.13 | 0.01(0.01)** |
| Income | 0.05 | 0.02(0.01) | 0.05 | 0.02(0.01) |
| Child age | −0.42 | −0.07(0.01)*** | −0.42 | −0.07(0.01)*** |
| C19 Impacts × Income | 0.01 | 0.00(0.00) | ||
| Parental burnout | ||||
| COVID-19 impacts | 0.24 | 0.49(0.06)*** | 0.24 | 0.50(0.06)*** |
| Depressive symptoms | 0.44 | 0.54(0.05)*** | 0.43 | 0.53(0.05)*** |
| Anxiety symptoms | 0.01 | 0.01(0.05) | 0.02 | 0.02(0.05) |
| Income | 0.09 | 0.32(0.10)*** | 0.09 | 0.32(0.10)*** |
| C19 Impacts × Income | −0.01 | −0.02(0.03) | ||
| Indirect effects | ||||
| C19 Impacts → Burnout → C Stress | 0.06 | 0.05(0.01)*** | ||
| C19 Impacts → Burnout → C Pos Beh | −0.06 | −0.01(0.00)*** | ||
| Total effects | ||||
| C19 Impacts → C Stress | 0.13 | 0.12(0.03)*** | ||
| C19 Impacts → C Pos Beh | −0.15 | −0.03(0.01)*** | ||
| Fit indices | ||||
| CFI | 0.992 | 0.993 | ||
| TLI | 0.967 | 0.969 | ||
| RMSEA | 0.039 | 0.035 | ||
| . | Path model 1 . | Path model 2 . | ||
|---|---|---|---|---|
| Std. est. | Estimate (SE) | Std. est. | Estimate (SE) | |
| Child stress behaviors | ||||
| COVID-19 impacts | 0.07 | 0.07(0.03)* | 0.08 | 0.07(0.03)* |
| Parental burnout | 0.24 | 0.11(0.02)*** | 0.23 | 0.11(0.02)*** |
| Depressive symptoms | 0.14 | 0.08(0.03)** | 0.14 | 0.08(0.03)** |
| Anxiety symptoms | 0.03 | 0.02(0.03) | 0.03 | 0.02(0.03) |
| Income | −0.04 | −0.07(0.05) | −0.04 | −0.07(0.05) |
| Child age | 0.24 | 0.20(0.02)*** | 0.24 | 0.20(0.02)*** |
| C19 Impacts × Income | −0.06 | −0.03(0.02)* | ||
| Child positive behavior | ||||
| COVID-19 impacts | −0.09 | −0.02(0.01)** | −0.10 | −0.02(0.01)** |
| Parental burnout | −0.24 | −0.02(0.00)*** | −0.24 | −0.02(0.00)*** |
| Depressive symptoms | −0.08 | −0.01(0.01) | −0.08 | −0.01(0.01) |
| Anxiety symptoms | 0.13 | 0.01(0.01)** | 0.13 | 0.01(0.01)** |
| Income | 0.05 | 0.02(0.01) | 0.05 | 0.02(0.01) |
| Child age | −0.42 | −0.07(0.01)*** | −0.42 | −0.07(0.01)*** |
| C19 Impacts × Income | 0.01 | 0.00(0.00) | ||
| Parental burnout | ||||
| COVID-19 impacts | 0.24 | 0.49(0.06)*** | 0.24 | 0.50(0.06)*** |
| Depressive symptoms | 0.44 | 0.54(0.05)*** | 0.43 | 0.53(0.05)*** |
| Anxiety symptoms | 0.01 | 0.01(0.05) | 0.02 | 0.02(0.05) |
| Income | 0.09 | 0.32(0.10)*** | 0.09 | 0.32(0.10)*** |
| C19 Impacts × Income | −0.01 | −0.02(0.03) | ||
| Indirect effects | ||||
| C19 Impacts → Burnout → C Stress | 0.06 | 0.05(0.01)*** | ||
| C19 Impacts → Burnout → C Pos Beh | −0.06 | −0.01(0.00)*** | ||
| Total effects | ||||
| C19 Impacts → C Stress | 0.13 | 0.12(0.03)*** | ||
| C19 Impacts → C Pos Beh | −0.15 | −0.03(0.01)*** | ||
| Fit indices | ||||
| CFI | 0.992 | 0.993 | ||
| TLI | 0.967 | 0.969 | ||
| RMSEA | 0.039 | 0.035 | ||
Note. C Pos Beh = child positive behavior; C Stress = child stress; C19 Impacts = COVID-19 psychological impacts.
p< .05;
p < .01;
p< .001.
Discussion
The current study investigated associations between parent and child well-being during the onset of the COVID-19 pandemic. Analyses revealed significant relations between parents’ perceptions of COVID-19’s psychological impacts and their experiences of parental burnout, and both predicted greater stress and fewer positive behaviors in children. Cross-sectional mediation analyses supported indirect links between parents’ COVID-19 psychological impacts and children’s stress and positive behaviors through parental burnout. Finally, the association between parents’ COVID-19 psychological impacts and children’s stress varied based on income, such that it was only significant at lower-income levels. Overall, these results highlight interrelations between parents’ and children’s well-being, suggesting parents’ perceptions of the pandemic’s mental health impacts contributed to both their own and their children’s well-being.
These results replicate what is known about parental stress and variations by income during non-pandemic contexts and expand to incorporate the novel stressor of the COVID-19 pandemic on parents’ mental health. Our results corroborate emerging COVID-19 work documenting links between parent and child well-being, such as links between parents’ general and COVID-19-specific worries and children’s internalizing and externalizing behaviors (Li & Zhou, 2021) and between decreased parental stress and positive child outcomes (Spinelli et al., 2020). Our analyses controlled for general depression and anxiety symptoms, suggesting that parents’ perceived pandemic-related mental health challenges uniquely contributed to their own and their children’s well-being. Furthermore, the moderating effect of income suggests that parents’ COVID-19 psychological impacts may amplify risk for children in lower-income families. This is not surprising given research documenting the pandemic’s exploitation of systemic inequalities present prior to the pandemic (e.g., Millett et al., 2020). Combined, these results indicate that parents’ perceptions of how the COVID-19 pandemic has impacted them have implications for their own and their children’s well-being, with inequities emerging based on income.
FST centers on interactions between family resources and perceptions in contributing to family outcomes when facing stress (McCubbin & Patterson, 1983), which is reflected in our findings. That is, families’ income (resources) interacted with families’ perceptions of COVID-19’s psychological impact (perception) to influence children’s behaviors. Extensions of FST have included the influence of changes to resources and in perceptions over time (e.g., McCubbin & Patterson, 1983), especially relevant given tremendous changes in family resources (e.g., income) since COVID-19’s onset (e.g., Ananat et al, 2020). Further research incorporating longitudinal pandemic-related changes to both family income and families’ meaning making of the pandemic are needed to expand on these findings.
Parents who reported greater COVID-19 psychological impacts also felt more burned out in their parenting role, and this explained much of the connection with children’s behaviors. Given established links between parental burnout and harsh parenting and child maltreatment (e.g., Mikolajczak et al., 2018), supporting parents and reducing parental burnout presents an important avenue for mitigating the impact of the pandemic on children. Especially early in the pandemic, families were stretched to their limits as they adjusted quickly to pandemic-related changes (e.g., social support access, school/childcare closures) and simultaneously navigated their own fears and uncertainties. Many families may still feel this strain in the form of parental burnout. While not specifically examined in this study, parents caring for children with physical or behavioral health concerns may have been especially vulnerable to both COVID-19 psychological impacts and increased parental burnout due to pre-pandemic strain (Tervo, 2012). Bolstering caregiving support for families (e.g., childcare, school programming, respite) is desperately needed to help alleviate caregiving strain and prevent spillover effects on children.
Furthermore, in addition to their own stress, children were also likely experiencing downstream effects of their parents’ stress, and vice versa, resulting in cascades of stress throughout the family unit. This bidirectionality may appear as changes in parenting behaviors and parents’ engagement with their children, resulting in parent-child relationship strain (e.g., Neece et al., 2012) and has implications for long-term transmission of psychopathology across generations. Our results highlight how parent-specific COVID-19 impacts (e.g., parents’ perception, job loss) present imminent risk to families’ well-being, potentially contributing to and exacerbating parents’ and children’s development of emotional and behavioral disorders. Longitudinal research is needed to disentangle these bidirectional and intergenerational effects and to determine the role of COVID-19 pandemic-specific stressors and psychological impacts on parent–child interactions, relationships, and mental and overall well-being.
Underscoring a critical need for family systems approaches to supporting families and alleviating pandemic impacts, these findings have numerous implications for clinical practice. First, with increased evidence of mental health strain and parental burnout, expanding parents’ and children’s access to and utilization of psychotherapy and other programs will be crucial moving forward. The COVID-19 pandemic illuminated the possibilities of telehealth and tele-mental health care, reducing some of the barriers to attending psychotherapy in person (e.g., Pierce et al., 2021). Continuing to expand on and ensure equitable access to “virtual” mental health resources is a promising avenue for supporting families.
Second, our results highlight the need for intergenerational preventative interventions aiming to mitigate the impact of the pandemic on parents and children and reduce the likelihood for intergenerational transmission of psychopathology. Given the likelihood of bidirectional and long-term intergenerational impacts between parents and children, supporting access to mental and behavioral health resources and interventions is needed. Expanding access to and funding for community- and school-based emotional and behavioral therapeutic interventions for families targeting both parents and children will be an important area for forthcoming policy and practice.
This study is not without limitations. First, generalizability is limited given the non-probability survey distribution method. This convenience sample contains an overrepresentation of those who are White (82% in this sample vs. 72% of the American population), women (89%), and those with higher incomes (65% of the sample earns more than $70,000/year compared to U.S. median family income of $63,179); though, it is more representative of the Wisconsin population (81% White) from which 80% of the sample was comprised. Given the COVID-19 pandemic’s disproportionate impacts on communities of color (Millett et al., 2020), these data likely do not reflect the experiences of marginalized families. Second, these data are cross-sectional and all data were from a single-reporter. Parents’ retrospective views of changes since the start of the pandemic are likely skewed and do not reflect true longitudinal change. Additionally, the child behavior questions were also parent-reported and retrospective in nature (e.g., have you noticed increases in your child’s behavior in any of the following?). It may have been difficult for parents to accurately perceive or report children’s experiences, and especially for parents most impacted by the pandemic. Future studies should include direct observations or assessments of parents and children and the use of multiple-informants (e.g., teachers) to better understand the impact the COVID-19 pandemic has had on families. Still, these findings provide a glimpse into U.S. parents’ perceptions of their well-being and parent–child relationships early in the COVID-19 pandemic.
Understanding how the broader COVID-19 pandemic context impacts parents and subsequently children both short- and long-term is important to support family well-being effectively. This study illuminates the added influence of COVID-19 pandemic-specific psychological impacts on parents during the beginning of the pandemic. Findings suggest that the extent to which parents perceive that the COVID-19 pandemic has negatively impacted their mental health is associated with more negative parent and child outcomes, especially for lower-income families. It is imperative that family-friendly policies, such as those providing direct child tax credits, and clinical interventions be implemented to offer the support that families need to overcome the immense challenges faced during these unprecedented times.
Funding
Support for this research was provided by the University of Wisconsin–Madison, Office of the Vice Chancellor for Research and Graduate Education with funding from the Wisconsin Alumni Research Foundation.
Conflicts of interest: None declared.
References
American Psychiatric Association. (
American Psychological Association. (
Child and Adolescent Health Measurement Initiative. (
World Health Organization (