-
PDF
- Split View
-
Views
-
Cite
Cite
Kyungmin Kim, Lauren R. Bangerter, Yin Liu, Courtney A. Polenick, Steven H. Zarit, Karen L. Fingerman, Middle-Aged Offspring’s Support to Aging Parents With Emerging Disability, The Gerontologist, Volume 57, Issue 3, 1 June 2017, Pages 441–450, https://doi.org/10.1093/geront/gnv686
Close - Share Icon Share
Abstract
A vast literature has examined family caregivers, but few studies explore transitions from providing ordinary support to parents to situations involving increasing dependency. Using 2 waves of data, we examined how parents’ increasing disability in activities of daily living (ADL) is associated with changes in everyday support patterns, relationship quality, and psychological well-being of middle-aged offspring, taking into account other informal and paid help to the parent.
Three hundred and eighty middle-aged adults reported on everyday support they provided to each parent (N = 487) and parent’s ADL at baseline and 5 years later.
Increased parents’ disability led to increases in offspring’s support, in particular tangible support. Support given by offspring was lower when parents received paid help but was not affected by help from other informal members (e.g., family members, friends). Increased disability was associated with decreases in positive relationship quality with parents; as well, offspring who provided actual help with ADL reported increases in negative relationship quality.
The effects of increasing parents’ disability on relationship quality and involvement of other informal and paid help may have implications for the longer-term impact of care on both offspring and their parents.
A fundamental issue in midlife is responding to parents’ illness or disability. Although caregiving is often described in the literature as if it has appeared de novo, care and other assistance to an older relative often emerge as a gradual process (Leopold, Raab, & Engelhardt, 2014). Most families have been providing ongoing support and assistance, including practical help and emotional support, prior to the onset of disabilities (Fingerman et al., 2011; Zarit & Eggebeen, 2002). In response to a parent’s developing disability, middle-aged children may augment the support they already give (e.g., providing more emotional support), as well as add new types of assistance (e.g., beginning to assist with activities of daily living [ADL]).
The transition period when a parent needs increasing help is important for establishing patterns of assistance that lead to more or less effective care down the road and affect the burden and well-being of their children (Gaugler, Zarit, & Pearlin, 2003; Rafnsson, Shankar, & Steptoe, 2015). We know little, however, about this formative period, particularly from a prospective standpoint. Most studies have examined situations where care patterns have already been established (Dunkle et al., 2014). Furthermore, research has focused almost exclusively on a single person identified as the primary caregiver, although assistance is often distributed among multiple offspring and relatives of disabled parents (Koehly, Ashida, Schafer, & Ludden, 2015; Tolkacheva, van Groenou, de Boer, & van Tilburg, 2011). When middle-aged adults are not providing hands-on care, they may help in other ways (e.g., socializing, managing finances; Lawrence, Goodnow, Woods, & Karantzas, 2002). Moreover, the emotional impact of a parent’s disability affects offspring, whether they have a primary role in providing care (Amirkhanyan & Wolf, 2003, 2006).
The current paper examined middle-aged adults’ responses to increasing disability in their aging parents. Middle-aged offspring were followed longitudinally over a 5-year interval. At baseline, most of their parents were independent or had low levels of disability. Over the 5-year period, many of the parents became increasingly disabled. We focused on how rising levels of disability affect support to parents and how that support is modulated by involvement from other informal members or paid help. We also considered the effects of these changes on (a) the quality of relationship between middle-aged adults and their parents and (b) the psychological well-being among middle-aged offspring (i.e., life satisfaction and depressive symptoms).
Theoretical Perspectives
This study is guided by two theoretical frameworks: caregiving as a career (Pearlin & Aneshensel, 1994) and the caregiving stress process (Aneshensel, Pearlin, Mullan, Zarit, & Whitlatch, 1995). The notion of “career” underscores that caregiving is not a static condition, but rather a progression over time in which demands generally increase and the challenges to caregivers change accordingly. Pearlin and Aneshensel (1994) characterized this progression as having three main phases: role acquisition, enactment, and role disengagement. Of these phases, we know the least about role acquisition. The transition to the care role is an amorphous phase that is not easily distinguished from the usual mutual support that occurs within families. As a parent’s needs change, offspring may do more of what they are already doing, as well as begin providing new types of assistance. These early aspects of caregiving are important because they are likely to continue to have an influence on how care is enacted over the long term (Gaugler et al., 2003).
The widely used caregiving stress process model (Aneshensel et al., 1995) complements the caregiving career framework by focusing on how caregivers respond subjectively to specific changes in their role and the help they provide in response to the emergence of a parent’s disability. We examined psychological well-being as well as ratings of quality of relationship with parents as likely areas that would be affected early in the care process. We investigated the link between these outcomes and potential stressors represented by a parent’s increasing disabilities and increased help to that parent from the offspring respondents in our study.
Parent Care as an Extension of Ongoing Support
Middle-aged adults routinely exchange support with their parents, including emotional support, socializing, practical assistance with household tasks, and financial help (Fingerman et al., 2011; Zarit & Eggebeen, 2002). Changes in a parent’s ability to perform instrumental and personal activities of daily living (IADL, ADL) often occur gradually (Pearlin & Aneshensel, 1994). These changes may affect the routine support that adult offspring provide, and they may begin helping parents with ADL (e.g., personal care, housework, transportation, and finances).
This continuity of support to a parent raises questions about definitions and boundaries of role acquisition. Typically, caregiving is defined in research as assisting a person with one or more IADL or ADL. Sometimes this definition also includes decision-making responsibility for an elder’s health care or living arrangements. Yet given the continuity of support, prior studies suggest that there is considerable heterogeneity in when people begin to see themselves as caregivers (Albert, Moss, & Lawton, 1996; Gaugler et al., 2003). Accordingly, we focused on the response of adult offspring to increasing parents’ disability, rather than on whether they perceive themselves as caregivers.
Multiple Helpers With Parental Disabilities
Most work has focused on primary caregivers (i.e., the person who provides the most help), but there is growing recognition that multiple family members may be involved in assisting a disabled elder with IADL or ADL needs or may provide other types of support (e.g., Szinovacz & Davey, 2007; Wolff & Kasper, 2006). Notably, Penrod, Kane, Kane, and Finch (1995) found that 88% of primary caregivers had at least one helper who provided direct care to the care receiver. Recent studies have similarly reported that multiple individuals are frequently involved in assisting disabled elders, some providing hands-on care and others giving other types of assistance to the elder and/or to a primary caregiver (Cheng, Lam, Kwok, Ng, & Fung, 2013; Koehly et al., 2015; Tolkacheva et al., 2011).
Support from family members has long been considered to have a fundamental impact on a caregiver’s burden and well-being (Zarit, Reever, & Bach-Peterson, 1980). The number of people involved in giving tangible and emotional support may be important for a caregiver’s well-being (Gatz, Bengtson, & Blum, 1990). Recent studies confirm that caregivers with larger support networks had lower burden and overload as well as greater satisfactions with their network (Cheng et al., 2013; Tolkacheva et al., 2011). Indeed, family interventions that focus on increasing participation of multiple family members in care are among the most effective interventions for reducing caregiver burden and distress (e.g., Joling et al., 2012; Mittelman, Ferris, Shulman, Steinberg, & Levin, 1996). Thus, assessing contributions by multiple family members early in the care process can be useful for understanding long-term caregiver outcomes.
This study examined the response of middle-aged adults to a parent’s increasing disability. Consistent with the caregiving career framework (Pearlin & Aneshensel, 1994), we looked longitudinally at continuities in support as well as how new demands for assistance may alter existing patterns of support. We expected that middle-aged offspring would increase support in response to a parent’s increasing disability. Specifically, we predicted that tangible assistance (e.g., practical assistance, financial support) would increase, whereas nontangible support (e.g., emotional support, listening to talk) would remain stable in response to a parent’s increasing disability. These changes in support are likely influenced by the presence of other informal members who provide help for parents as well as the use of paid help, and so we considered these other sources of support as a key contextual factor.
Stress Associated With the Transition to Care
Despite the extensive literature on caregiving stress, only a few studies have examined family members’ stress and well-being during role acquisition and the transition into caregiving. The available studies show that in the pre-caregiving period, family members experience increased depression or other symptoms of emotional distress (e.g., Burton, Zdaniuk, Schulz, Jackson, & Hirsch, 2003; Dunkle et al., 2014; Marks, Lambert, & Choi, 2002; Rafnsson et al., 2015). Furthermore, a parent’s increasing disability may lead to greater depressive symptoms whether an offspring is involved in providing hands-on help (Amirkhanyan & Wolf, 2003, 2006). Thus, we considered the effects of a parent’s increasing disability on offspring’s depressive symptoms and life satisfaction, regardless of whether they were directly involved in assisting with their parents’ disabilities.
Another consideration is how increased parents’ disability may affect the quality of relationship between middle-aged adults and their parents. When parents experience increasing cognitive, behavioral, and emotional problems, quality of the relationship may suffer (Aneshensel et al., 1995; Quinn, Clare, & Woods, 2009; Stoller & Pugliesi, 1989). Furthermore, parents who need help with daily activities or for living safely at home often will resist efforts of their children to provide help or to hire paid assistance (Heid, Zarit, & Fingerman, 2015). There may also be continuity or intensifying of tensions in the parent–child relationship that preceded onset of disabilities (Fingerman, Hay, Kamp Dush, Cichy, & Hosterman, 2007). Thus, we expected that increasing disability will lead to less positive quality and more negative quality in their relationship with parents.
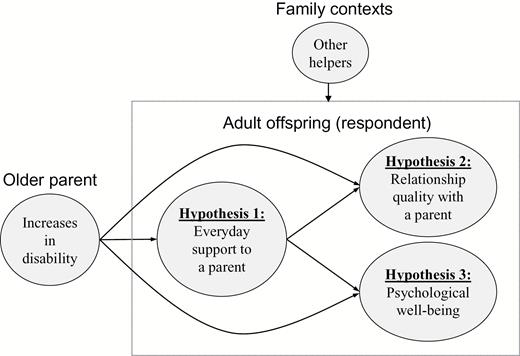
In sum, we proposed the following hypotheses (see Figure 1).
Three hypotheses to examine effects of increasing parents’ disabilities.
Hypothesis 1: With increases in parents’ disability, middle-aged offspring will increase overall support provided to parents—specifically, tangible support (i.e., practical and financial help), but not nontangible support (i.e., emotional support, socializing, and advice). When parents receive help from other family members, friends/neighbors, or paid help, offspring will show smaller increases in support over time. Also, offspring will show an attenuated response to increasing parents’ disability.
Hypothesis 2: Increasing disability of a parent will lead to poorer relationship quality. Changes in the relationship quality with parents will be affected by ADL help that the middle-aged adult provides as well as whether parents receive help from other family members or paid help.
Hypothesis 3: Increasing disability of a parent will lead to declines in life satisfaction and increases in depressive symptoms. These changes will be affected by ADL help that the middle-aged adult provides as well as whether parents receive help from other family members or paid help.
Methods
Sample
We used data from two waves of the Family Exchanges Study (Fingerman, Miller, Birditt, & Zarit, 2009). The original sample consisted of 633 middle-aged adults (aged 40–60) who reside in the Philadelphia Metropolitan Area in 2008. Since the Family Exchanges Study aimed to examine middle-aged adults’ intergenerational relationships across three generations, eligible participants should have at least one child over age 18 and one living parent. The study identified potential participants via listed samples from Genesys Corporation supplemented with random digit dialing within geographic area codes. Computer-assisted telephone interviews were conducted with the middle-aged participants for approximately 1hr.
We collected a second wave of data in 2013, and 490 participants from Wave 1 completed a telephone or web-based surveys (77%) lasting approximately 1hr. Out of 490 participants, 383 (78%) had at least one living parent at Wave 2. Because three participants did not provide information on parents’ disabilities, this study included 380 middle-aged adults reporting on 487 parents (see Table 1 for sample characteristics).
Characteristics of Middle-Aged Offspring and Their Parents at Wave 2
| . | Middle-aged offspring . | Parent . | ||
|---|---|---|---|---|
| . | M . | (SD) . | M . | (SD) . |
| Age | 55.43 | (4.90) | 81.05 | (6.27) |
| Female, % | 56 | 66 | ||
| Years of education | 14.44 | (1.98) | 12.39 | (2.72) |
| Household incomea | 6.39 | (2.79) | — | |
| Physical healthb | 3.31 | (0.98) | 2.71 | (1.02) |
| Racial/ethnic minority, % | 35 | — | ||
| Marital status, % | ||||
| Married/remarried | 72 | 41 | ||
| Divorced/separated | 17 | 12 | ||
| Never married | 6 | 2 | ||
| Widowed | 3 | 45 | ||
| Employed for pay, % | 71 | 6 | ||
| Number of children | 2.82 | (1.47) | — | |
| Number of siblings | 3.02 | (2.18) | — | |
| Number of living parents | 1.29 | (0.46) | — | |
| Distance from (respondent) offspringc | — | 210.48 | (526.90) | |
| Coresiding with (respondent) offspring, % | — | 7 | ||
| . | Middle-aged offspring . | Parent . | ||
|---|---|---|---|---|
| . | M . | (SD) . | M . | (SD) . |
| Age | 55.43 | (4.90) | 81.05 | (6.27) |
| Female, % | 56 | 66 | ||
| Years of education | 14.44 | (1.98) | 12.39 | (2.72) |
| Household incomea | 6.39 | (2.79) | — | |
| Physical healthb | 3.31 | (0.98) | 2.71 | (1.02) |
| Racial/ethnic minority, % | 35 | — | ||
| Marital status, % | ||||
| Married/remarried | 72 | 41 | ||
| Divorced/separated | 17 | 12 | ||
| Never married | 6 | 2 | ||
| Widowed | 3 | 45 | ||
| Employed for pay, % | 71 | 6 | ||
| Number of children | 2.82 | (1.47) | — | |
| Number of siblings | 3.02 | (2.18) | — | |
| Number of living parents | 1.29 | (0.46) | — | |
| Distance from (respondent) offspringc | — | 210.48 | (526.90) | |
| Coresiding with (respondent) offspring, % | — | 7 | ||
Notes: Child (respondent) N = 380; parent N = 487.
a1 = less than $10,000; 2 = $10,001–$25,000; 3 = $25,001–$40,000; 4 = $40,001–$50,000; 5 = $50,000–$60,000; 6 = $60,001–$75,000; 7 = $75,001–$100,000; 8 = $100,001–$125,000; 9 = $125,001–$150,000; 10 = $150,001–$200,000; 11 = $200,001–$250,000; 12 = $250,001 or more.
bRated 1 = poor to 5 = excellent.
cDistance in miles.
Characteristics of Middle-Aged Offspring and Their Parents at Wave 2
| . | Middle-aged offspring . | Parent . | ||
|---|---|---|---|---|
| . | M . | (SD) . | M . | (SD) . |
| Age | 55.43 | (4.90) | 81.05 | (6.27) |
| Female, % | 56 | 66 | ||
| Years of education | 14.44 | (1.98) | 12.39 | (2.72) |
| Household incomea | 6.39 | (2.79) | — | |
| Physical healthb | 3.31 | (0.98) | 2.71 | (1.02) |
| Racial/ethnic minority, % | 35 | — | ||
| Marital status, % | ||||
| Married/remarried | 72 | 41 | ||
| Divorced/separated | 17 | 12 | ||
| Never married | 6 | 2 | ||
| Widowed | 3 | 45 | ||
| Employed for pay, % | 71 | 6 | ||
| Number of children | 2.82 | (1.47) | — | |
| Number of siblings | 3.02 | (2.18) | — | |
| Number of living parents | 1.29 | (0.46) | — | |
| Distance from (respondent) offspringc | — | 210.48 | (526.90) | |
| Coresiding with (respondent) offspring, % | — | 7 | ||
| . | Middle-aged offspring . | Parent . | ||
|---|---|---|---|---|
| . | M . | (SD) . | M . | (SD) . |
| Age | 55.43 | (4.90) | 81.05 | (6.27) |
| Female, % | 56 | 66 | ||
| Years of education | 14.44 | (1.98) | 12.39 | (2.72) |
| Household incomea | 6.39 | (2.79) | — | |
| Physical healthb | 3.31 | (0.98) | 2.71 | (1.02) |
| Racial/ethnic minority, % | 35 | — | ||
| Marital status, % | ||||
| Married/remarried | 72 | 41 | ||
| Divorced/separated | 17 | 12 | ||
| Never married | 6 | 2 | ||
| Widowed | 3 | 45 | ||
| Employed for pay, % | 71 | 6 | ||
| Number of children | 2.82 | (1.47) | — | |
| Number of siblings | 3.02 | (2.18) | — | |
| Number of living parents | 1.29 | (0.46) | — | |
| Distance from (respondent) offspringc | — | 210.48 | (526.90) | |
| Coresiding with (respondent) offspring, % | — | 7 | ||
Notes: Child (respondent) N = 380; parent N = 487.
a1 = less than $10,000; 2 = $10,001–$25,000; 3 = $25,001–$40,000; 4 = $40,001–$50,000; 5 = $50,000–$60,000; 6 = $60,001–$75,000; 7 = $75,001–$100,000; 8 = $100,001–$125,000; 9 = $125,001–$150,000; 10 = $150,001–$200,000; 11 = $200,001–$250,000; 12 = $250,001 or more.
bRated 1 = poor to 5 = excellent.
cDistance in miles.
Measures
Parent’s Disability
At each wave, we assessed parents’ disability, using four items from the Community Disability Scale (Bassett & Folstein, 1991; Rovner, Zisselman, & Shmuely-Dulitzku, 1996). Participants indicated whether each living parent needed help with (a) personal care, (b) housework, (c) transportation, and (d) finances. The items were summed to indicate parent’s total disability (α = .84 at Wave 1; α = .78 at Wave 2).
Help With Parent’s ADL Tasks
If a parent had any disability in ADL, we asked how often participants provided help with ADL tasks, rated from 1 (less than once a year or not at all) to 8 (daily). Participants also listed any other people who helped their parent with ADL. Other helpers were categorized into three groups: (a) family members, (b) friends or neighbors, and (c) paid help.
Everyday Support
We assessed frequency of everyday support that middle-aged participants provided to each parent, using six items from the Intergenerational Support Scale (ISS; Fingerman et al., 2011): (a) emotional support, (b) practical assistance (e.g., fixing something around the house, running an errand), (c) advice, (d) socializing, (e) listening to talk about the parent’s daily events, and (f) financial support. Responses were rated from 1 (less than once a year or not at all) to 8 (daily). We calculated mean scores across the six types of support (i.e., “overall” support index; α = .88 at Wave 1; α = .87 at Wave 2). We examined the overall support index as well as each type of support.
Relationship Quality
Participants rated positive and negative relationship qualities toward each parent (Birditt, Tighe, Fingerman, & Zarit, 2012; Umberson, 1992). Positive relationship quality was assessed with two items: (a) loving and caring and (b) feeling understood by the parent. Two items assessed negative relationship quality: (a) criticizing and (b) demanding. Participants rated the items from 1 (not at all) to 5 (a great deal), and mean scores were calculated for positive relationship quality (α = .67 at Wave 1; α = .71 at Wave 2) and negative relationship quality (α = .72 at Wave 1; α = .71 at Wave 2). Positive and negative relationship qualities were negatively correlated (r = −.26 at Wave 1; r = −.25 at Wave 2).
Psychological Well-Being
We assessed two dimensions of psychological well-being: (a) depressive symptoms and (b) life satisfaction. For depressive symptoms, five items from the Brief Symptom Inventory (BSI; Derogatis, 2000) were used. Participants rated how often they experienced these feelings in the past 7 days (i.e., lonely, blue, worthless, hopeless about the future, no interest in things) from 1 (not at all) to 5 (extremely), and a mean score was calculated (α = .81 at Wave 1; α = .87 at Wave 2). Life satisfaction was measured by one item, rated from 1 (not at all satisfied) to 10 (completely satisfied; Diener, Gohm, Suh, & Oishi, 2000).
Background Characteristics
Participants reported their demographic characteristics: age, gender (1 = female, 0 = male), years of education, marital status (1 = re/married, 0 = not married), household income (1 = less than $10,000 to 12 = $250,001 or more), employment status (1 = employed for pay, 0 = not employed), physical health (1 = poor to 5 = excellent), and race/ethnicity (1 = racial/ethnic minority, 0 = non-Hispanic white). Participants also reported family size (i.e., the number of siblings, the number of children).
Participants provided background information about each living parent, including age, gender (1 = female, 0 = male), years of education, marital status (1 = re/married, 0 = not married), physical health (1 = poor to 5 = excellent), geographic distance to the parent’s residence (miles), and living arrangement (1 = coresiding with middle-aged offspring, 0 = not coresiding).
Analytic Strategy
To address whether parents’ increasing disability leads to changes in everyday support that middle-aged offspring provided to parents (Hypothesis 1), we estimated multilevel models (MLM; Littell, Milliken, Stroup, & Wolfinger, 1996). Because 107 participants had two living parents and 273 had one living parent, we considered a family level (Level 2) to explain the shared variance of parents from the same family. In the models, we examined overall support as well as each type of support at Wave 2 as separate outcomes. We entered parents’ ADL changes (i.e., change scores between Waves 1 and 2) as a main predictor, controlling for levels of ADL needs and support at Wave 1 (Model 1). Next, we added variables for three sources of help (i.e., family members, friends or neighbors, and paid help) indicating whether each parent is receiving help with ADL needs from these sources (Model 2). Finally, we examined interaction terms between parents’ ADL changes and three sources of help (Model 3) to see if the effect of increasing disability on changes in support the respondent offspring provided varies by the existence of other help. Participants’ demographics (i.e., gender, education, marital status, employment status, race/ethnicity, number of siblings, and number of children) and parents’ demographics (i.e., gender, age, education, marital status, distance from respondent child [log-transformed], and living arrangement) were controlled in the models.
To test implications of increased parents’ disability for relationship quality (Hypothesis 2), we estimated MLM with positive and negative relationship qualities with each parent (at Wave 2) as outcomes. We first examined ADL changes at Wave 2 as a predictor, controlling for levels of ADL needs and relationship quality at Wave 1 (Model 1). Then, we added participants’ ADL help and other sources of ADL help to the models (Model 2). The same demographic variables were controlled as in the previous models.
Finally, to examine offspring’s psychological well-being as outcomes (Hypothesis 3), multiple regressions were conducted. We used regressions because unlike outcomes in the previous models, well-being measures (i.e., depressive symptoms and life satisfaction) were offspring-level variables. For participants who had two living parents, we used information about the parent who showed higher ADL needs within the family as predictors. ADL changes between Waves 1 and 2 were first examined as a predictor for psychological well-being, controlling for levels of ADL needs and well-being at Wave 1 (Model 1). We then added participants’ ADL help and three sources of help to the models (Model 2). Participants’ demographics were controlled in the models.
Results
Parents’ disability increased over the 5-year period; 22% of parents (n = 109) had ADL disabilities in 2008, and 55% (n = 270) had ADL disabilities in 2013 (Table 2). The average number of ADL needs also increased between Waves 1 and 2 (paired t = −12.60, p < .001).
Parents’ Disability at Waves 1 and 2
| . | Wave 1 (2008) . | Wave 2 (2013) . |
|---|---|---|
| Have any ADL disabilities, % | 22 | 55 |
| (a) Help with personal care, % | 5 | 17 |
| (b) Help with housework, % | 19 | 29 |
| (c) Help with transportation, % | 18 | 44 |
| (d) Help with finances, % | 12 | 30 |
| Number of ADLa, M (SD) | 0.54 (1.11) | 1.29 (1.42) |
| . | Wave 1 (2008) . | Wave 2 (2013) . |
|---|---|---|
| Have any ADL disabilities, % | 22 | 55 |
| (a) Help with personal care, % | 5 | 17 |
| (b) Help with housework, % | 19 | 29 |
| (c) Help with transportation, % | 18 | 44 |
| (d) Help with finances, % | 12 | 30 |
| Number of ADLa, M (SD) | 0.54 (1.11) | 1.29 (1.42) |
Notes: Child (respondent) N = 380; parent N = 487. ADL = activities of daily living.
aCount of four ADL items.
Parents’ Disability at Waves 1 and 2
| . | Wave 1 (2008) . | Wave 2 (2013) . |
|---|---|---|
| Have any ADL disabilities, % | 22 | 55 |
| (a) Help with personal care, % | 5 | 17 |
| (b) Help with housework, % | 19 | 29 |
| (c) Help with transportation, % | 18 | 44 |
| (d) Help with finances, % | 12 | 30 |
| Number of ADLa, M (SD) | 0.54 (1.11) | 1.29 (1.42) |
| . | Wave 1 (2008) . | Wave 2 (2013) . |
|---|---|---|
| Have any ADL disabilities, % | 22 | 55 |
| (a) Help with personal care, % | 5 | 17 |
| (b) Help with housework, % | 19 | 29 |
| (c) Help with transportation, % | 18 | 44 |
| (d) Help with finances, % | 12 | 30 |
| Number of ADLa, M (SD) | 0.54 (1.11) | 1.29 (1.42) |
Notes: Child (respondent) N = 380; parent N = 487. ADL = activities of daily living.
aCount of four ADL items.
Respondents reported providing help with parents’ ADL tasks between once to a few times a month (M = 4.61, SD = 2.12). Most parents (95%) received help with ADL tasks from other sources, in addition to the respondent offspring. Specifically, 75% of parents received help with ADL from other family members, including their spouse (13%), another child or child-in-law (62%), and other relatives (17%). Six percent of parents had help from friends or neighbors and 17% had paid assistance with ADL tasks.
Regarding Hypothesis 1 (Table 3), we found that respondent offspring increased overall support when parents’ disability increased between Waves 1 and 2 of the study (B = 0.11, p = .005; Model 1). Looking at each type of support separately (Model 1 in Supplementary Tables 1–6), we found significant increases in tangible support (i.e., practical assistance and financial support) and advice, but not in nontangible forms of everyday support (i.e., emotional support, listening to the parent talk about his/her daily events, and socializing). When other sources of help were added (Model 2), the association between increased parent’s disability and respondent offspring’s overall support remained significant (B = 0.13, p = .012). Parents’ use of paid help was associated with lower levels of respondents’ overall support, but help from other family members had no effect. For specific types of support (Model 2 in Supplementary Tables 1–6), increasing disability was significantly associated with respondents’ increased financial support (B = 0.15, p = .003), emotional support (B = 0.21, p = .023), and advice (B = 0.19, p = .028). Help with ADL by other family members was positively associated with amount of respondents’ practical assistance (B = 0.47, p = .009). Use of paid help was negatively associated with respondents’ emotional support (B = −0.67, p = .038) and financial support (B = −0.41, p = .033). The three sources of help (other family members, friends/neighbors, paid help) did not show moderating effects between parents’ ADL changes and the amount of the respondents’ overall support as well as types of support (Model 3 in Table 3 and Supplementary Tables 1–6).
Multilevel Models for Overall Everyday Support to Parents at Wave 2 With Parent Disability Changes and Other Informal and Paid Help
| . | Model 1 . | Model 2 . | Model 3 . | |||||
|---|---|---|---|---|---|---|---|---|
| . | Estimate . | (SE) . | . | Estimate . | (SE) . | . | Estimate . | (SE) . |
| Fixed effects | ||||||||
| Intercept | 0.31 | (0.87) | −0.00 | (0.87) | −0.00 | (0.88) | ||
| Parent ADL changes (at Wave 2) | 0.11** | (0.04) | 0.13* | (0.05) | 0.13* | (0.06) | ||
| Other help with parent ADL needs | ||||||||
| Family members | 0.03 | (0.12) | 0.04 | (0.14) | ||||
| Friends or neighbors | 0.48 | (0.28) | 0.30 | (0.49) | ||||
| Paid help | −0.41* | (0.18) | −0.47 | (0.26) | ||||
| Interactions of parent ADL changes | ||||||||
| × Family members | −0.01 | (0.08) | ||||||
| × Friends or neighbors | 0.14 | (0.32) | ||||||
| × Paid help | 0.03 | (0.11) | ||||||
| Controls | ||||||||
| Parent ADL needs (at Wave 1) | −0.04 | (0.05) | −0.02 | (0.06) | −0.01 | (0.06) | ||
| Support (at Wave 1) | 0.61*** | (0.04) | 0.61*** | (0.04) | 0.61*** | (0.04) | ||
| Demographics | ||||||||
| Child: Female | 0.07 | (0.11) | 0.06 | (0.11) | 0.06 | (0.11) | ||
| Child: Years of education | −0.02 | (0.03) | −0.01 | (0.03) | −0.01 | (0.03) | ||
| Child: Re/married | 0.14 | (0.12) | 0.15 | (0.12) | 0.15 | (0.12) | ||
| Child: Employed for pay | 0.12 | (0.12) | 0.14 | (0.12) | 0.14 | (0.12) | ||
| Child: Racial/ethnic minority | 0.06 | (0.13) | 0.07 | (0.13) | 0.07 | (0.13) | ||
| Child: Number of children | 0.04 | (0.04) | 0.04 | (0.04) | 0.04 | (0.04) | ||
| Child: Number of siblings | −0.02 | (0.02) | −0.02 | (0.02) | −0.02 | (0.02) | ||
| Parent: Female | 0.26** | (0.10) | 0.26** | (0.10) | 0.26** | (0.10) | ||
| Parent: Age | 0.01 | (0.01) | 0.01 | (0.01) | 0.01 | (0.01) | ||
| Parent: Years of education | 0.04 | (0.02) | 0.04* | (0.02) | 0.04* | (0.02) | ||
| Parent: Re/married | −0.04 | (0.11) | −0.03 | (0.11) | −0.04 | (0.11) | ||
| Parent: Coresiding with respondent | 0.90*** | (0.20) | 0.89*** | (0.20) | 0.89*** | (0.20) | ||
| Parent: Distance from respondenta | −0.24*** | (0.06) | −0.24*** | (0.06) | −0.24*** | (0.06) | ||
| Random effects | ||||||||
| Intercept variance | 0.50*** | (0.10) | 0.49*** | (0.10) | 0.49*** | (0.10) | ||
| Residual variance | 0.53*** | (0.08) | 0.53*** | (0.08) | 0.53*** | (0.08) | ||
| −2 log-likelihood | 1,325.4 | 1,321.0 | 1,326.9 | |||||
| . | Model 1 . | Model 2 . | Model 3 . | |||||
|---|---|---|---|---|---|---|---|---|
| . | Estimate . | (SE) . | . | Estimate . | (SE) . | . | Estimate . | (SE) . |
| Fixed effects | ||||||||
| Intercept | 0.31 | (0.87) | −0.00 | (0.87) | −0.00 | (0.88) | ||
| Parent ADL changes (at Wave 2) | 0.11** | (0.04) | 0.13* | (0.05) | 0.13* | (0.06) | ||
| Other help with parent ADL needs | ||||||||
| Family members | 0.03 | (0.12) | 0.04 | (0.14) | ||||
| Friends or neighbors | 0.48 | (0.28) | 0.30 | (0.49) | ||||
| Paid help | −0.41* | (0.18) | −0.47 | (0.26) | ||||
| Interactions of parent ADL changes | ||||||||
| × Family members | −0.01 | (0.08) | ||||||
| × Friends or neighbors | 0.14 | (0.32) | ||||||
| × Paid help | 0.03 | (0.11) | ||||||
| Controls | ||||||||
| Parent ADL needs (at Wave 1) | −0.04 | (0.05) | −0.02 | (0.06) | −0.01 | (0.06) | ||
| Support (at Wave 1) | 0.61*** | (0.04) | 0.61*** | (0.04) | 0.61*** | (0.04) | ||
| Demographics | ||||||||
| Child: Female | 0.07 | (0.11) | 0.06 | (0.11) | 0.06 | (0.11) | ||
| Child: Years of education | −0.02 | (0.03) | −0.01 | (0.03) | −0.01 | (0.03) | ||
| Child: Re/married | 0.14 | (0.12) | 0.15 | (0.12) | 0.15 | (0.12) | ||
| Child: Employed for pay | 0.12 | (0.12) | 0.14 | (0.12) | 0.14 | (0.12) | ||
| Child: Racial/ethnic minority | 0.06 | (0.13) | 0.07 | (0.13) | 0.07 | (0.13) | ||
| Child: Number of children | 0.04 | (0.04) | 0.04 | (0.04) | 0.04 | (0.04) | ||
| Child: Number of siblings | −0.02 | (0.02) | −0.02 | (0.02) | −0.02 | (0.02) | ||
| Parent: Female | 0.26** | (0.10) | 0.26** | (0.10) | 0.26** | (0.10) | ||
| Parent: Age | 0.01 | (0.01) | 0.01 | (0.01) | 0.01 | (0.01) | ||
| Parent: Years of education | 0.04 | (0.02) | 0.04* | (0.02) | 0.04* | (0.02) | ||
| Parent: Re/married | −0.04 | (0.11) | −0.03 | (0.11) | −0.04 | (0.11) | ||
| Parent: Coresiding with respondent | 0.90*** | (0.20) | 0.89*** | (0.20) | 0.89*** | (0.20) | ||
| Parent: Distance from respondenta | −0.24*** | (0.06) | −0.24*** | (0.06) | −0.24*** | (0.06) | ||
| Random effects | ||||||||
| Intercept variance | 0.50*** | (0.10) | 0.49*** | (0.10) | 0.49*** | (0.10) | ||
| Residual variance | 0.53*** | (0.08) | 0.53*** | (0.08) | 0.53*** | (0.08) | ||
| −2 log-likelihood | 1,325.4 | 1,321.0 | 1,326.9 | |||||
Notes: Child (respondent) N = 380; parent N = 487. ADL = activities of daily living.
aLog-transformed miles.
*p < .05. **p < .01. ***p < .001.
Multilevel Models for Overall Everyday Support to Parents at Wave 2 With Parent Disability Changes and Other Informal and Paid Help
| . | Model 1 . | Model 2 . | Model 3 . | |||||
|---|---|---|---|---|---|---|---|---|
| . | Estimate . | (SE) . | . | Estimate . | (SE) . | . | Estimate . | (SE) . |
| Fixed effects | ||||||||
| Intercept | 0.31 | (0.87) | −0.00 | (0.87) | −0.00 | (0.88) | ||
| Parent ADL changes (at Wave 2) | 0.11** | (0.04) | 0.13* | (0.05) | 0.13* | (0.06) | ||
| Other help with parent ADL needs | ||||||||
| Family members | 0.03 | (0.12) | 0.04 | (0.14) | ||||
| Friends or neighbors | 0.48 | (0.28) | 0.30 | (0.49) | ||||
| Paid help | −0.41* | (0.18) | −0.47 | (0.26) | ||||
| Interactions of parent ADL changes | ||||||||
| × Family members | −0.01 | (0.08) | ||||||
| × Friends or neighbors | 0.14 | (0.32) | ||||||
| × Paid help | 0.03 | (0.11) | ||||||
| Controls | ||||||||
| Parent ADL needs (at Wave 1) | −0.04 | (0.05) | −0.02 | (0.06) | −0.01 | (0.06) | ||
| Support (at Wave 1) | 0.61*** | (0.04) | 0.61*** | (0.04) | 0.61*** | (0.04) | ||
| Demographics | ||||||||
| Child: Female | 0.07 | (0.11) | 0.06 | (0.11) | 0.06 | (0.11) | ||
| Child: Years of education | −0.02 | (0.03) | −0.01 | (0.03) | −0.01 | (0.03) | ||
| Child: Re/married | 0.14 | (0.12) | 0.15 | (0.12) | 0.15 | (0.12) | ||
| Child: Employed for pay | 0.12 | (0.12) | 0.14 | (0.12) | 0.14 | (0.12) | ||
| Child: Racial/ethnic minority | 0.06 | (0.13) | 0.07 | (0.13) | 0.07 | (0.13) | ||
| Child: Number of children | 0.04 | (0.04) | 0.04 | (0.04) | 0.04 | (0.04) | ||
| Child: Number of siblings | −0.02 | (0.02) | −0.02 | (0.02) | −0.02 | (0.02) | ||
| Parent: Female | 0.26** | (0.10) | 0.26** | (0.10) | 0.26** | (0.10) | ||
| Parent: Age | 0.01 | (0.01) | 0.01 | (0.01) | 0.01 | (0.01) | ||
| Parent: Years of education | 0.04 | (0.02) | 0.04* | (0.02) | 0.04* | (0.02) | ||
| Parent: Re/married | −0.04 | (0.11) | −0.03 | (0.11) | −0.04 | (0.11) | ||
| Parent: Coresiding with respondent | 0.90*** | (0.20) | 0.89*** | (0.20) | 0.89*** | (0.20) | ||
| Parent: Distance from respondenta | −0.24*** | (0.06) | −0.24*** | (0.06) | −0.24*** | (0.06) | ||
| Random effects | ||||||||
| Intercept variance | 0.50*** | (0.10) | 0.49*** | (0.10) | 0.49*** | (0.10) | ||
| Residual variance | 0.53*** | (0.08) | 0.53*** | (0.08) | 0.53*** | (0.08) | ||
| −2 log-likelihood | 1,325.4 | 1,321.0 | 1,326.9 | |||||
| . | Model 1 . | Model 2 . | Model 3 . | |||||
|---|---|---|---|---|---|---|---|---|
| . | Estimate . | (SE) . | . | Estimate . | (SE) . | . | Estimate . | (SE) . |
| Fixed effects | ||||||||
| Intercept | 0.31 | (0.87) | −0.00 | (0.87) | −0.00 | (0.88) | ||
| Parent ADL changes (at Wave 2) | 0.11** | (0.04) | 0.13* | (0.05) | 0.13* | (0.06) | ||
| Other help with parent ADL needs | ||||||||
| Family members | 0.03 | (0.12) | 0.04 | (0.14) | ||||
| Friends or neighbors | 0.48 | (0.28) | 0.30 | (0.49) | ||||
| Paid help | −0.41* | (0.18) | −0.47 | (0.26) | ||||
| Interactions of parent ADL changes | ||||||||
| × Family members | −0.01 | (0.08) | ||||||
| × Friends or neighbors | 0.14 | (0.32) | ||||||
| × Paid help | 0.03 | (0.11) | ||||||
| Controls | ||||||||
| Parent ADL needs (at Wave 1) | −0.04 | (0.05) | −0.02 | (0.06) | −0.01 | (0.06) | ||
| Support (at Wave 1) | 0.61*** | (0.04) | 0.61*** | (0.04) | 0.61*** | (0.04) | ||
| Demographics | ||||||||
| Child: Female | 0.07 | (0.11) | 0.06 | (0.11) | 0.06 | (0.11) | ||
| Child: Years of education | −0.02 | (0.03) | −0.01 | (0.03) | −0.01 | (0.03) | ||
| Child: Re/married | 0.14 | (0.12) | 0.15 | (0.12) | 0.15 | (0.12) | ||
| Child: Employed for pay | 0.12 | (0.12) | 0.14 | (0.12) | 0.14 | (0.12) | ||
| Child: Racial/ethnic minority | 0.06 | (0.13) | 0.07 | (0.13) | 0.07 | (0.13) | ||
| Child: Number of children | 0.04 | (0.04) | 0.04 | (0.04) | 0.04 | (0.04) | ||
| Child: Number of siblings | −0.02 | (0.02) | −0.02 | (0.02) | −0.02 | (0.02) | ||
| Parent: Female | 0.26** | (0.10) | 0.26** | (0.10) | 0.26** | (0.10) | ||
| Parent: Age | 0.01 | (0.01) | 0.01 | (0.01) | 0.01 | (0.01) | ||
| Parent: Years of education | 0.04 | (0.02) | 0.04* | (0.02) | 0.04* | (0.02) | ||
| Parent: Re/married | −0.04 | (0.11) | −0.03 | (0.11) | −0.04 | (0.11) | ||
| Parent: Coresiding with respondent | 0.90*** | (0.20) | 0.89*** | (0.20) | 0.89*** | (0.20) | ||
| Parent: Distance from respondenta | −0.24*** | (0.06) | −0.24*** | (0.06) | −0.24*** | (0.06) | ||
| Random effects | ||||||||
| Intercept variance | 0.50*** | (0.10) | 0.49*** | (0.10) | 0.49*** | (0.10) | ||
| Residual variance | 0.53*** | (0.08) | 0.53*** | (0.08) | 0.53*** | (0.08) | ||
| −2 log-likelihood | 1,325.4 | 1,321.0 | 1,326.9 | |||||
Notes: Child (respondent) N = 380; parent N = 487. ADL = activities of daily living.
aLog-transformed miles.
*p < .05. **p < .01. ***p < .001.
Regarding Hypothesis 2, parents’ increasing disability at Wave 2 was associated with decreased reports by respondents of positive relationship quality (Table 4, Model 1; B = −0.10, p < .001) and increased negative relationship quality (B = 0.08, p = .005). When we entered ADL help given by the respondent offspring and the presence of other sources of help into the models (Model 2), the effects of increasing parents’ disability on positive relationship quality were still significant (B = −0.14, p = .001). For negative relationship quality, increasing disability was no longer significant. Rather, when respondents specifically assisted with ADL, negative relationship quality with parents was greater (B = 0.06, p = .009).
Multilevel Models Predicting Relationship Quality at Wave 2 With Parent Disability Changes and Offspring Help With ADL
| . | Positive relationship quality . | Negative relationship quality . | ||||||
|---|---|---|---|---|---|---|---|---|
| . | Model 1 . | Model 2 . | Model 1 . | Model 2 . | ||||
| . | Estimate . | (SE) . | Estimate . | (SE) . | Estimate . | (SE) . | Estimate . | (SE) . |
| Fixed effects | ||||||||
| Intercept | 0.77 | (0.59) | 0.70 | (0.60) | 1.19 | (0.61) | 1.23* | (0.61) |
| Parent ADL changes (at Wave 2) | −0.10*** | (0.03) | −0.14** | (0.04) | 0.08** | (0.03) | 0.01 | (0.04) |
| Help with parent ADL needsa | 0.03 | (0.02) | 0.06** | (0.02) | ||||
| Other help with parent ADL needs | ||||||||
| Family members | 0.06 | (0.09) | −0.08 | (0.09) | ||||
| Friends or neighbors | 0.01 | (0.19) | 0.01 | (0.20) | ||||
| Paid help | −0.10 | (0.12) | 0.12 | (0.13) | ||||
| Controls | ||||||||
| Parent ADL needs (at Wave 1) | −0.08* | (0.03) | −0.11* | (0.04) | 0.03 | (0.04) | −0.04 | (0.05) |
| Relationship quality (at Wave 1) | 0.71*** | (0.04) | 0.70*** | (0.04) | 0.68*** | (0.04) | 0.68*** | (0.04) |
| Demographics | ||||||||
| Child: Female | −0.10 | (0.07) | −0.10 | (0.07) | 0.09 | (0.07) | 0.11 | (0.07) |
| Child: Years of education | 0.01 | (0.02) | 0.01 | (0.02) | 0.02 | (0.02) | 0.01 | (0.02) |
| Child: Re/married | −0.06 | (0.08) | −0.06 | (0.08) | 0.03 | (0.09) | 0.01 | (0.09) |
| Child: Employed for pay | 0.00 | (0.08) | 0.02 | (0.08) | −0.07 | (0.08) | −0.06 | (0.08) |
| Child: Racial/ethnic minority | −0.09 | (0.09) | −0.10 | (0.09) | 0.18* | (0.09) | 0.16 | (0.09) |
| Child: Number of children | 0.02 | (0.02) | 0.01 | (0.02) | −0.04 | (0.02) | −0.05 | (0.02) |
| Child: Number of siblings | 0.01 | (0.02) | 0.01 | (0.02) | −0.02 | (0.02) | −0.01 | (0.02) |
| Parent: Female | 0.03 | (0.07) | 0.03 | (0.07) | 0.14 | (0.07) | 0.14* | (0.07) |
| Parent: Age | 0.01 | (0.01) | 0.01 | (0.01) | −0.01 | (0.01) | −0.01 | (0.01) |
| Parent: Years of education | −0.02 | (0.01) | −0.02 | (0.01) | −0.01 | (0.01) | −0.02 | (0.01) |
| Parent: Re/married | 0.03 | (0.08) | 0.04 | (0.08) | −0.01 | (0.08) | 0.01 | (0.08) |
| Parent: Coresiding with respondent | 0.23 | (0.14) | 0.20 | (0.14) | 0.39** | (0.14) | 0.30* | (0.15) |
| Parent: Distance from respondentb | 0.00 | (0.04) | 0.02 | (0.04) | −0.02 | (0.04) | 0.01 | (0.04) |
| Random effects | ||||||||
| Intercept variance | 0.19*** | (0.05) | 0.20*** | (0.05) | 0.19** | (0.07) | 0.18** | (0.06) |
| Residual variance | 0.28*** | (0.04) | 0.27*** | (0.04) | 0.32*** | (0.06) | 0.32*** | (0.06) |
| −2 log-likelihood | 984.8 | 993.6 | 1,025.0 | 1,029.6 | ||||
| . | Positive relationship quality . | Negative relationship quality . | ||||||
|---|---|---|---|---|---|---|---|---|
| . | Model 1 . | Model 2 . | Model 1 . | Model 2 . | ||||
| . | Estimate . | (SE) . | Estimate . | (SE) . | Estimate . | (SE) . | Estimate . | (SE) . |
| Fixed effects | ||||||||
| Intercept | 0.77 | (0.59) | 0.70 | (0.60) | 1.19 | (0.61) | 1.23* | (0.61) |
| Parent ADL changes (at Wave 2) | −0.10*** | (0.03) | −0.14** | (0.04) | 0.08** | (0.03) | 0.01 | (0.04) |
| Help with parent ADL needsa | 0.03 | (0.02) | 0.06** | (0.02) | ||||
| Other help with parent ADL needs | ||||||||
| Family members | 0.06 | (0.09) | −0.08 | (0.09) | ||||
| Friends or neighbors | 0.01 | (0.19) | 0.01 | (0.20) | ||||
| Paid help | −0.10 | (0.12) | 0.12 | (0.13) | ||||
| Controls | ||||||||
| Parent ADL needs (at Wave 1) | −0.08* | (0.03) | −0.11* | (0.04) | 0.03 | (0.04) | −0.04 | (0.05) |
| Relationship quality (at Wave 1) | 0.71*** | (0.04) | 0.70*** | (0.04) | 0.68*** | (0.04) | 0.68*** | (0.04) |
| Demographics | ||||||||
| Child: Female | −0.10 | (0.07) | −0.10 | (0.07) | 0.09 | (0.07) | 0.11 | (0.07) |
| Child: Years of education | 0.01 | (0.02) | 0.01 | (0.02) | 0.02 | (0.02) | 0.01 | (0.02) |
| Child: Re/married | −0.06 | (0.08) | −0.06 | (0.08) | 0.03 | (0.09) | 0.01 | (0.09) |
| Child: Employed for pay | 0.00 | (0.08) | 0.02 | (0.08) | −0.07 | (0.08) | −0.06 | (0.08) |
| Child: Racial/ethnic minority | −0.09 | (0.09) | −0.10 | (0.09) | 0.18* | (0.09) | 0.16 | (0.09) |
| Child: Number of children | 0.02 | (0.02) | 0.01 | (0.02) | −0.04 | (0.02) | −0.05 | (0.02) |
| Child: Number of siblings | 0.01 | (0.02) | 0.01 | (0.02) | −0.02 | (0.02) | −0.01 | (0.02) |
| Parent: Female | 0.03 | (0.07) | 0.03 | (0.07) | 0.14 | (0.07) | 0.14* | (0.07) |
| Parent: Age | 0.01 | (0.01) | 0.01 | (0.01) | −0.01 | (0.01) | −0.01 | (0.01) |
| Parent: Years of education | −0.02 | (0.01) | −0.02 | (0.01) | −0.01 | (0.01) | −0.02 | (0.01) |
| Parent: Re/married | 0.03 | (0.08) | 0.04 | (0.08) | −0.01 | (0.08) | 0.01 | (0.08) |
| Parent: Coresiding with respondent | 0.23 | (0.14) | 0.20 | (0.14) | 0.39** | (0.14) | 0.30* | (0.15) |
| Parent: Distance from respondentb | 0.00 | (0.04) | 0.02 | (0.04) | −0.02 | (0.04) | 0.01 | (0.04) |
| Random effects | ||||||||
| Intercept variance | 0.19*** | (0.05) | 0.20*** | (0.05) | 0.19** | (0.07) | 0.18** | (0.06) |
| Residual variance | 0.28*** | (0.04) | 0.27*** | (0.04) | 0.32*** | (0.06) | 0.32*** | (0.06) |
| −2 log-likelihood | 984.8 | 993.6 | 1,025.0 | 1,029.6 | ||||
Notes: Child (respondent) N = 380; parent N = 487. ADL = activities of daily living.
aHelp respondent offspring provided to parents; rated 1 = less than once per year to 8 = daily.
bLog-transformed miles.
*p < .05. **p < .01. ***p < .001.
Multilevel Models Predicting Relationship Quality at Wave 2 With Parent Disability Changes and Offspring Help With ADL
| . | Positive relationship quality . | Negative relationship quality . | ||||||
|---|---|---|---|---|---|---|---|---|
| . | Model 1 . | Model 2 . | Model 1 . | Model 2 . | ||||
| . | Estimate . | (SE) . | Estimate . | (SE) . | Estimate . | (SE) . | Estimate . | (SE) . |
| Fixed effects | ||||||||
| Intercept | 0.77 | (0.59) | 0.70 | (0.60) | 1.19 | (0.61) | 1.23* | (0.61) |
| Parent ADL changes (at Wave 2) | −0.10*** | (0.03) | −0.14** | (0.04) | 0.08** | (0.03) | 0.01 | (0.04) |
| Help with parent ADL needsa | 0.03 | (0.02) | 0.06** | (0.02) | ||||
| Other help with parent ADL needs | ||||||||
| Family members | 0.06 | (0.09) | −0.08 | (0.09) | ||||
| Friends or neighbors | 0.01 | (0.19) | 0.01 | (0.20) | ||||
| Paid help | −0.10 | (0.12) | 0.12 | (0.13) | ||||
| Controls | ||||||||
| Parent ADL needs (at Wave 1) | −0.08* | (0.03) | −0.11* | (0.04) | 0.03 | (0.04) | −0.04 | (0.05) |
| Relationship quality (at Wave 1) | 0.71*** | (0.04) | 0.70*** | (0.04) | 0.68*** | (0.04) | 0.68*** | (0.04) |
| Demographics | ||||||||
| Child: Female | −0.10 | (0.07) | −0.10 | (0.07) | 0.09 | (0.07) | 0.11 | (0.07) |
| Child: Years of education | 0.01 | (0.02) | 0.01 | (0.02) | 0.02 | (0.02) | 0.01 | (0.02) |
| Child: Re/married | −0.06 | (0.08) | −0.06 | (0.08) | 0.03 | (0.09) | 0.01 | (0.09) |
| Child: Employed for pay | 0.00 | (0.08) | 0.02 | (0.08) | −0.07 | (0.08) | −0.06 | (0.08) |
| Child: Racial/ethnic minority | −0.09 | (0.09) | −0.10 | (0.09) | 0.18* | (0.09) | 0.16 | (0.09) |
| Child: Number of children | 0.02 | (0.02) | 0.01 | (0.02) | −0.04 | (0.02) | −0.05 | (0.02) |
| Child: Number of siblings | 0.01 | (0.02) | 0.01 | (0.02) | −0.02 | (0.02) | −0.01 | (0.02) |
| Parent: Female | 0.03 | (0.07) | 0.03 | (0.07) | 0.14 | (0.07) | 0.14* | (0.07) |
| Parent: Age | 0.01 | (0.01) | 0.01 | (0.01) | −0.01 | (0.01) | −0.01 | (0.01) |
| Parent: Years of education | −0.02 | (0.01) | −0.02 | (0.01) | −0.01 | (0.01) | −0.02 | (0.01) |
| Parent: Re/married | 0.03 | (0.08) | 0.04 | (0.08) | −0.01 | (0.08) | 0.01 | (0.08) |
| Parent: Coresiding with respondent | 0.23 | (0.14) | 0.20 | (0.14) | 0.39** | (0.14) | 0.30* | (0.15) |
| Parent: Distance from respondentb | 0.00 | (0.04) | 0.02 | (0.04) | −0.02 | (0.04) | 0.01 | (0.04) |
| Random effects | ||||||||
| Intercept variance | 0.19*** | (0.05) | 0.20*** | (0.05) | 0.19** | (0.07) | 0.18** | (0.06) |
| Residual variance | 0.28*** | (0.04) | 0.27*** | (0.04) | 0.32*** | (0.06) | 0.32*** | (0.06) |
| −2 log-likelihood | 984.8 | 993.6 | 1,025.0 | 1,029.6 | ||||
| . | Positive relationship quality . | Negative relationship quality . | ||||||
|---|---|---|---|---|---|---|---|---|
| . | Model 1 . | Model 2 . | Model 1 . | Model 2 . | ||||
| . | Estimate . | (SE) . | Estimate . | (SE) . | Estimate . | (SE) . | Estimate . | (SE) . |
| Fixed effects | ||||||||
| Intercept | 0.77 | (0.59) | 0.70 | (0.60) | 1.19 | (0.61) | 1.23* | (0.61) |
| Parent ADL changes (at Wave 2) | −0.10*** | (0.03) | −0.14** | (0.04) | 0.08** | (0.03) | 0.01 | (0.04) |
| Help with parent ADL needsa | 0.03 | (0.02) | 0.06** | (0.02) | ||||
| Other help with parent ADL needs | ||||||||
| Family members | 0.06 | (0.09) | −0.08 | (0.09) | ||||
| Friends or neighbors | 0.01 | (0.19) | 0.01 | (0.20) | ||||
| Paid help | −0.10 | (0.12) | 0.12 | (0.13) | ||||
| Controls | ||||||||
| Parent ADL needs (at Wave 1) | −0.08* | (0.03) | −0.11* | (0.04) | 0.03 | (0.04) | −0.04 | (0.05) |
| Relationship quality (at Wave 1) | 0.71*** | (0.04) | 0.70*** | (0.04) | 0.68*** | (0.04) | 0.68*** | (0.04) |
| Demographics | ||||||||
| Child: Female | −0.10 | (0.07) | −0.10 | (0.07) | 0.09 | (0.07) | 0.11 | (0.07) |
| Child: Years of education | 0.01 | (0.02) | 0.01 | (0.02) | 0.02 | (0.02) | 0.01 | (0.02) |
| Child: Re/married | −0.06 | (0.08) | −0.06 | (0.08) | 0.03 | (0.09) | 0.01 | (0.09) |
| Child: Employed for pay | 0.00 | (0.08) | 0.02 | (0.08) | −0.07 | (0.08) | −0.06 | (0.08) |
| Child: Racial/ethnic minority | −0.09 | (0.09) | −0.10 | (0.09) | 0.18* | (0.09) | 0.16 | (0.09) |
| Child: Number of children | 0.02 | (0.02) | 0.01 | (0.02) | −0.04 | (0.02) | −0.05 | (0.02) |
| Child: Number of siblings | 0.01 | (0.02) | 0.01 | (0.02) | −0.02 | (0.02) | −0.01 | (0.02) |
| Parent: Female | 0.03 | (0.07) | 0.03 | (0.07) | 0.14 | (0.07) | 0.14* | (0.07) |
| Parent: Age | 0.01 | (0.01) | 0.01 | (0.01) | −0.01 | (0.01) | −0.01 | (0.01) |
| Parent: Years of education | −0.02 | (0.01) | −0.02 | (0.01) | −0.01 | (0.01) | −0.02 | (0.01) |
| Parent: Re/married | 0.03 | (0.08) | 0.04 | (0.08) | −0.01 | (0.08) | 0.01 | (0.08) |
| Parent: Coresiding with respondent | 0.23 | (0.14) | 0.20 | (0.14) | 0.39** | (0.14) | 0.30* | (0.15) |
| Parent: Distance from respondentb | 0.00 | (0.04) | 0.02 | (0.04) | −0.02 | (0.04) | 0.01 | (0.04) |
| Random effects | ||||||||
| Intercept variance | 0.19*** | (0.05) | 0.20*** | (0.05) | 0.19** | (0.07) | 0.18** | (0.06) |
| Residual variance | 0.28*** | (0.04) | 0.27*** | (0.04) | 0.32*** | (0.06) | 0.32*** | (0.06) |
| −2 log-likelihood | 984.8 | 993.6 | 1,025.0 | 1,029.6 | ||||
Notes: Child (respondent) N = 380; parent N = 487. ADL = activities of daily living.
aHelp respondent offspring provided to parents; rated 1 = less than once per year to 8 = daily.
bLog-transformed miles.
*p < .05. **p < .01. ***p < .001.
Finally, we examined implications of parents’ increased disability for respondents’ psychological well-being (Hypothesis 3). We did not find any significant effects of increased parent’s disability on respondent offspring’s depressive symptoms and life satisfaction (see Supplementary Table 7). In addition, respondent offspring’s ADL help and presence of other helpers were not associated with offspring’s well-being at Wave 2.
Discussion
Guided by the caregiving career framework (Pearlin & Aneshensel, 1994), this study explored how middle-aged offspring changed their support provision in response to increasing parents’ disability over the 5-year period. We also considered whether the grown child’s support provision was affected by help from other family members, friends/neighbors, and paid help. Findings suggest that middle-aged children expand some of the support they are already giving as well as add new types of assistance.
Consistent with the relatively low levels of disability among parents in the study, adult offspring provided hands-on help with parental ADL needs infrequently (i.e., “monthly” to “a few times a month”). Most parents had other family members who helped with ADL tasks in addition to the respondent offspring, such as a spouse, siblings, or in-laws. Also, some parents employed paid help to assist with ADL tasks, suggesting that disabled parents rely on formal and informal sources of help to meet their needs (Koehly et al., 2015; Szinovacz & Davey, 2007; Tolkacheva et al., 2011). Future research should focus on how these support networks (in)effectively organize and coordinate with one another, including the degree of choice and control that older adults exert over who helps them.
Parents’ Disability and Everyday Support Patterns
With increases in parents’ disability, middle-aged offspring gave more tangible support (i.e., practical assistance and financial support), whereas most nontangible forms of everyday support (i.e., emotional support, listening to the parent talk, and socializing) were not associated with changes in parents’ disability. The finding is consistent with the caregiving literature, which focuses primarily on practical assistance or financial support (e.g., Wolff & Kasper, 2006). The one exception for nontangible support was advice, which increased when parents incurred disabilities. The question did not specify what type of advice offspring offered, but it is likely that at least some of these interactions pertained to decisions about medical and home care (Boerner, Carr, & Moorman, 2013).
When we considered other sources of help with parental ADL, the effect of increasing parents’ disabilities on respondents’ overall support remained significant. Respondents increased their support whether other family members or friends/neighbors were assisting with ADL. For parents who were married, we did not know if their spouse was helping with ADL, but parents’ marital status was not associated with increases in offspring’s routine support. Only parents’ use of paid help leads to less support provided by respondents.
We found somewhat different patterns of changes for each type of support after considering other sources of help. Specifically, practical assistance was no longer significant but emotional support was now significant. The attenuation of effects of disability on respondents’ practical assistance when other sources of support were added may suggest that all sources of help are increasing with growing disabilities. By contrast, the addition of paid help to the models may have unmasked the association of emotional support and disabilities for respondents, though the specific mechanisms for this process require further investigation.
We also examined if the respondent offspring’s response to increasing parents’ disabilities varied by the presence of other help. However, we did not find any significant moderating effects in overall support as well as types of support. Thus, it appears that other sources of help (i.e., paid help) were associated with the levels in support that adult offspring provide but did not alter how the offspring responds to parents’ disabilities.
Parents’ Disability, Relationship Quality With Parents, and Offspring Well-Being
Consistent with the stress process model (Aneshensel et al., 1995), increased parents’ disability had implications for relationship quality. Greater parents’ ADL disability led to diminished positive relationship quality. Prior work suggests that positive qualities of relationships may increase when parents incur health problems (Fingerman et al., 2007), but other research has found that offspring perceive less parental affection when parents’ health declines (Stoller & Pugliesi, 1989). Disability may reduce participation in activities and limit opportunities for enjoyable parent–child interactions that are critical to maintaining positive relationship quality.
Increasing disability also was associated with increased negative relationship quality, but offspring help with ADL tasks accounted for the increased negative relationship quality. Providing help with ADL goes beyond routine support and may generate situations that are wrought with friction. In general, it is difficult to provide support in a way that is helpful to the recipient (Maisel & Gable, 2009), and this may be particularly the case with parents. As such, offspring assistance with parents’ ADL needs requires considerable finesse to avoid impairing the parent–child relationship.
Surprisingly, offspring well-being was not sensitive to changes in parents’ disability or to providing increased support. The caregiving literature typically finds that providing intensive support has a detrimental impact on caregivers’ well-being (Aneshensel et al., 1995). The lack of findings pertaining to well-being in this study suggests that the transition to caregiving may not generate such detrimental effects.
Limitations and Directions for Future Research
The study is limited in several respects. Our measure/definition for parents’ disabilities was limited to ADL and did not include other common dimensions of disability, such as climbing stairs or walking (Fauth, Zarit, Malmberg, & Johansson, 2007). The current study involved a broad sample of older adults, rather than focusing on a caregiving sample. As such, it is not clear whether some offspring on this spectrum were unaffected, whereas others were affected by giving daily support. Finally, the study was limited to the perspective of one focal offspring. Future research should incorporate multiple family members with multiple perspectives to better understand how support processes evolve over time. Families may balance help to an aging parent across multiple sources of support (Szinovacz & Davey, 2007), and research should further investigate how they balance this support.
This study confirms that as parents incur physical disabilities over time, offspring provide increasing routine support as well as taking on assistance with ADL to compensate for their parents’ inability to complete tasks of daily life. Furthermore, most parents also have other people in their lives who provide support, including siblings, in-laws, and paid help. Good cooperation within a family around care issues may help them to continue the provision of high quality care at home for parents without over-burdening any particular individual. Interventions and policies that focus on a single caregiver may miss opportunities for building a more sustainable pattern of shared family assistance. Furthermore, as prior studies have suggested (Gaugler et al., 2003; Pearlin & Aneshensel, 1994), early intervention during this critical transition of enactment of care may help families avoid some of the predictable stressors associated with caregiving.
Supplementary Material
Supplementary material can be found at: http://gerontologist.oxfordjournals.org.
Funding
This study was supported by grants from the National Institute on Aging (NIA), R01AG027769, “Family Exchanges Study II” and “Psychology of Intergenerational Transfers” (Principal Investigator: K. L. Fingerman) and R03AG048879, “Generational Family Patterns and Well-Being” (Principal Investigator: K. Kim). This research was supported by grant, 5 R24 HD042849, awarded to the Population Research Center (PRC) at The University of Texas at Austin by the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD).
References
Author notes
*Address correspondence to Kyungmin Kim, PhD, Department of Gerontology, John W. McCormack Graduate School of Policy and Global Studies, University of Massachusetts Boston, 100 Morrissey Boulevard, Boston, MA 02125-3393. E-mail: kyungmin.kim@umb.edu
Decision Editor: Rachel Pruchno, PhD