-
PDF
- Split View
-
Views
-
Cite
Cite
Jun Zhao, Shama Virani, Hutcha Sriplung, Spatiotemporal mapping of cervical cancer incidence highlights need for targeted prevention in Songkhla province, Thailand, Health Policy and Planning, Volume 32, Issue 3, April 2017, Pages 430–436, https://doi.org/10.1093/heapol/czw145
Close - Share Icon Share
Abstract
Background: The national cervical cancer screening program in Thailand has been successful in reducing overall burden from this disease. However, evaluation on spatial and temporal scales is needed to assess the efficacy of this program in smaller regions. Here, we geographically assess incidence in a province with a uniquely heterogeneous distribution of lifestyle factors associated with religiosity.
Methods: Cervical cancer cases were extracted from the provincial cancer registry from 1989 to 2013. Age-adjusted incidence rates were calculated using population statistics from the census bureau and adjusted to the Segi world standard population. Bayesian hierarchical modelling was employed to spatiotemporally map cervical cancer incidence trends in Songkhla province in 5-year period.
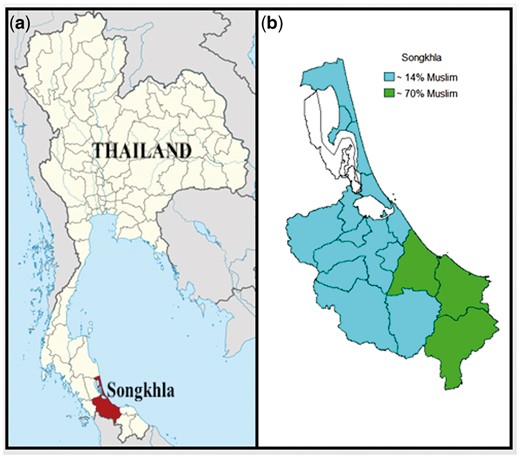
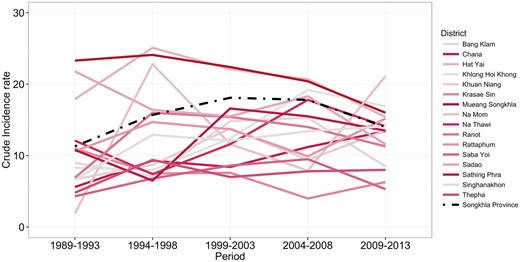
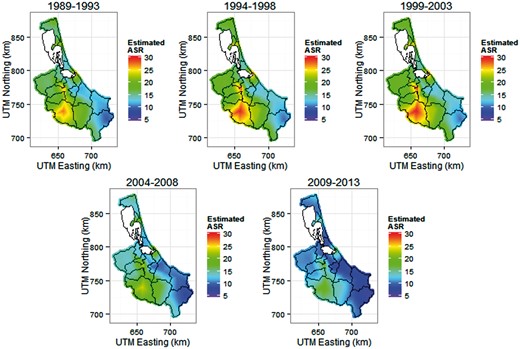
Results: Overall, the incidence of cervical cancer decreased in Songkhla province. The three districts with a Muslim population of greater than 70% had consistently lower cervical cancer rates from 1989 to 2013 compared with the rest of the predominantly Buddhist districts. Hotspots of incidence were identified in Sadao, Hat Yai and the juncture of Mueang Songkhla and Singhanakhon in each 5-year period.
Conclusions: Distinct cervical cancer incidence trends by religion over time indicate differences in sexual habits, lifestyle and religion-associated culture between Muslims and Buddhists, and suggest divergent risk factor profiles for these groups. The high incidence rates in Sadao and Hat Yai is likely explained by the main road to Malaysia, which runs across these two areas and has frequent commercial sex trade. Female sex workers should be targeted as a vulnerable population for screening efforts to address this continuing burden of cervical cancer.
Key Messages
This study is the first to use spatiotemporal modelling to identify hotspots of cervical cancer in Thailand in a region with a unique population and location.
Using Bayesian spatiotemporal modelling, we found that although rates have decreased in Songkhla, there were consistently high incidence rates in a vulnerable population of commercial sex workers and lower rates in predominantly Muslim districts.
Our findings indicate a need for targeted prevention efforts in the vulnerable population of female sex workers to continue to address the burden of cervical cancer in Thailand.
Introduction
Cervical cancer is one of the top female cancers in Thailand, making up 13% of incidence cancer cases and 12% of cancer deaths in women in 2012 (Khuhaprema et al. 2012,, 2013). Cervical cancer screening was implemented occasionally and promoted only on special occasions. In 2004, systematic screening programs were implemented under universal health care coverage (UC) for all Thai women ages 35–60 years at 5-year intervals (Srivatanakul 2004; Sriamporn et al. 2006; Khuhaprema et al. 2012). The success of the screening program was demonstrated by the decreasing rates of cancer incidence nationally (Khuhaprema et al. 2013). Nonetheless, cervical cancer incidence rates are still a concern as they vary widely across and within regions in Thailand. Songkhla is a province in southern Thailand that exhibited a similar overall decrease in cervical cancer incidence upon screening implementation, although rates vary by district. This province is unique in that it consists of districts with a high proportion of Muslims (Sriplung et al. 2014a). Cultural differences by religion are associated with distinct lifestyle characteristics that can affect risk of cancer. In addition, Songkhla is located close to the Thai border and is an area of high tourism, potentially including sex tourism, due to its location. The unique religious makeup combined with the location of this region gives rise to a heterogeneous distribution of risk factors, which likely contributes to the varying incidence rates across Songkhla. To determine what districts should be targeted for further prevention strategies, it is necessary to visualize cervical cancer rates geospatially.
Population-based cancer registry data is an effective way to understand the nature of a disease in a population. Registry data have been used to identify cancer trends, inform resource planning and guide hypotheses for population-based epidemiologic research (Khuhaprema et al. 2012, 2013; Virani et al. 2014). To fully understand the extent of cervical cancer screening and incidence in Songkhla, it is important to look at incidence rates geographically across time. Spatiotemporal mapping is a tool used to visualize the spatial pattern of relative risks within a region over time. The mapping of disease incidence and prevalence has long been a part of public health, epidemiology, and the study of disease in human populations (Koch 2005). Here, we compile population-based cancer registry data from the Songkhla cancer registry to analyze data from 25 years (1989–2013) using Bayesian hierarchical modelling. The goal of these analyses was to highlight the change of cervical cancer incidence in the province, and visualize spatial and temporal variations by mapping the incidence of cervical cancer in Songkhla province over a time span of 25 years. This is the first study to utilize population-based cancer registry data for spatiotemporal modelling and mapping of incidence rates in southern Thailand.
Materials and methods
Region
Map of Songkhla and Thailand. (a) Location of Songkhla Province (highlighted) in Thailand and (b) Religious majority in each district within Songkhla Province.
Recruitment of cervical cancer cases
The population-based cancer registry of Songkhla covers 16 districts in southern Thailand. The population of southern Thailand at the 2010 census was 8.9 million people of which 4.4 million were females (National Statistical Office 2013). This registry actively compiles cancer cases from 23 sources including community hospitals, private hospitals and the population registration office. The number of undetected cases is difficult to estimate due to remote villages with limited access to health facilities and the use of traditional Thai medicine in lieu of health care services. However, this registry has expected completeness >95% evaluated by capture-recapture method (Suwanrungruang et al. 2011). Invasive cervical cancer cases were extracted from the Songkhla Cancer Registry from 1989 through 2013 using ICD-10 codes C53.X. Information collected from the cancer registry included age, date of diagnosis, cancer stage and address code. The registry codes cervical cancer stage as ‘In situ’, ‘Local’, ‘Regional’, ‘Distant’ and ‘Unknown’. In situ cases consist of cancerous cells in the surface layer of the cervix. Localized tumours have spread in the cervix but not spread beyond the uterus. These tumours correspond to stage IA to stage IIA in the FIGO staging system. Regional tumours have spread beyond the uterus but are still contained in the pelvic region. These tumours correspond to stage IIB to stage III in the FIGO staging system. Distant tumours have metastasized, usually to the liver, bones or brain.
Population denominators
Population denominators for incidence rate calculations were estimated from the three population censuses surveyed by the National Statistical Office in 1990, 2000 and 2010 (National Statistical Office 1994, 2002, 2013). The population denominators by both sexes for all districts were readily present in the censuses. Intercensal populations were estimated using a log-linear function between two consecutive censuses. The populations beyond 2010 were estimated and reported by the Office of the National Economic and Social Development Board (Office of the National Economic and Social Development Board of Thailand 2013).
Statistical analysis
Age-adjusted cervical cancer incidence rates in Songkhla, Thailand from 1989 to 2013 were calculated for eighteen age groups (0–4, 5–9, …, 80–84 and ≥85) and adjusted to the world standard population proposed by Segi (1960) and later modified by Doll et al. (1966). Due to small cell sizes for cases per age group and the resulting large standard errors, crude incidence rates were calculated for each district for each 5-year period and plotted to visualize variability. To produce the maps, crude incidence rates were calculated for each one of the total 127 subdistricts for 5-year periods 1989–1993, 1994–1998, 1999–2003, 2004–2008 and 2009–2013. Geographical data of specific coordinates of the provincial borders, districts’ borders, subdistricts’ borders, as well as the borders of Songkhla Lake was downloaded (Hijmans 2015). Latent spatial correlations among nearby areas, due to dependence on spatially varying unobserved risk factors, were accounted for using a Bayesian model-based approach. This approach offers a mechanism of utilizing measurements across small areas to improve local estimates, resulting in the smoothing of extreme rates (Sun et al. 2000). Integrated Nested Laplace Approximation (INLA) was used to provide the simulation-based Markov Chain Monte Carlo schemes needed for Bayesian integrations (Rue et al. 2009).
is the incidence rate of cervical cancer at location ; is the random effect of spatially latent factors; is the vector parameter of the random effect, determined from the smoothness parameter and the logarithm of the scale parameter .
The posterior marginal distributions followed by the posterior mean and posterior standard deviation were calculated from the random effect using the INLA approach implemented on R-INLA package. Posterior means calculated for each pixel were used as in the log linear model for smoothing of incidence rates. Posterior means were adjusted by mid-period ASRs (i.e. ASR in 1991 in the first period) as the reference year for each period.
Mapping
GFs are conventionally defined by their mean and covariance function defined for two locations and in a two-dimensional space. The SPDE approach transforms the continuously indexed GFs into discretely indexed Gaussian Markov random fields (GRMFs). It creates triangulation of the domain, through subdivision into non-intersecting triangles. Linear combinations of basic functions defined on the locations of the set of vertices in the triangulation are used to represent the field.
Integrated Nested Laplace Approximation (INLA) was used as the inferential algorithm to conduct MCMC computations of the dense GF spatial correlation matrix (Simpson et al. 2011). The smallest unit for the INLA computation was subdistricts. Observations for each subdistrict were assigned to a defined geographical central point. The central point was defined as the median coordinates of the boundaries of each subdistrict. The outputs of the Bayesian estimation model are x, y and estimated incidence for pixels (x, y) on a Cartesian coordinate system from the lower left corner to the upper right corner. The outputs were plotted on a dense grid in the domain and overlaid with the boundaries of districts and province. To make all periods comparable, a uniform relative scale with themed colour was chosen for all the maps. The rainbow colours ranged from indigo, representing low rates, to red, representing high rates. Progressive changing of the colour corresponds to relative change in the estimated ASR. Each map has 195651 pixel points. The unit of the estimated ASR is per 105 female populations.
Readers interested in the INLA methodology and SPDE approach are referred to the R-INLA tutorial: SPDE models (Krainski and Lindgren 2014). R-statistical software and a number of R packages were used to analyse and visualize the data (R Development Core Team; Sriplung 2014; Wickham and Chang 2014,; Lindgren and Rue 2015).
Results
Descriptive analysis
A total of 3218 cases were diagnosed with cervical cancer from 1989 to 2013. Out of these, 2492 cases (77%) were invasive cases and 726 (23%) presented in situ. The age of diagnosis ranged from 17 to 98 years.
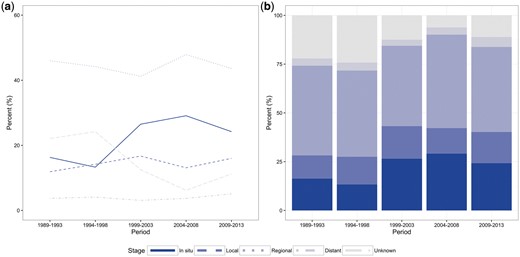
Stage distribution. (a) Regional tumours make up the largest proportion of cervical cancer cases across all periods while the percent of unknown cases has decreased by 2009–2013. (b) The proportion of in situ and localized tumours combined make up almost half of all cases in the last three periods.
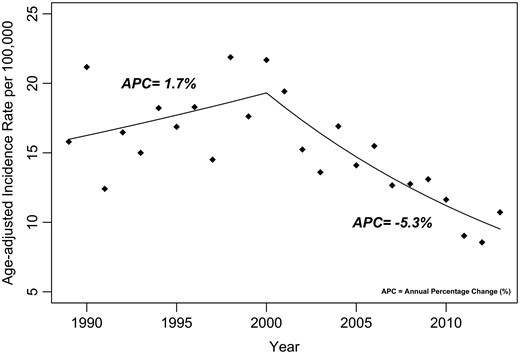
Age-adjusted standardized incidence rates of cervical cancer for Songkhla province from 1989 to 2013.
Crude incidence rates for each 5-year period for each district in Songkhla province (multicoloured) compared with crude incidence in Songkhla province (black).
Bayesian hierarchical models
Triangulation, used to transform the continuously indexed GFs into discretely indexed GRMFs, fit 83 triangles to our data. Parameter estimates for each model are shown in Table 1. We applied these parameter values into the inverse of the link functions to get the response scales of the occurrence variable and the incidence variable (Table 2). The estimated values look similar to the observed values calculated directly from our data in each period, demonstrating that the smoothed rates are reasonable estimations.
Parameter estimates used to calculate posterior statistics for mapping
| Model . | αy . | αz . | β . | φ . | ||||
|---|---|---|---|---|---|---|---|---|
| . | Mean . | SD . | Mean . | SD . | Mean . | SD . | Mean . | SD . |
| Model1 (1989-1993) | 0.768 | 0.266 | 2.610 | 0.165 | 1.160 | 0.298 | 4.151 | 0.737 |
| Model2 (1994-1998) | 1.227 | 0.303 | 2.729 | 0.199 | 1.103 | 0.305 | 3.581 | 0.525 |
| Model3 (1999-2003) | 1.362 | 0.310 | 2.696 | 0.206 | 1.041 | 0.305 | 5.277 | 0.791 |
| Model4 (2004-2008) | 1.554 | 0.406 | 2.840 | 0.318 | 0.986 | 0.321 | 3.568 | 0.521 |
| Model5 (2009-2013) | 1.966 | 0.404 | 2.531 | 0.249 | 1.127 | 0.312 | 4.616 | 0.673 |
| Model . | αy . | αz . | β . | φ . | ||||
|---|---|---|---|---|---|---|---|---|
| . | Mean . | SD . | Mean . | SD . | Mean . | SD . | Mean . | SD . |
| Model1 (1989-1993) | 0.768 | 0.266 | 2.610 | 0.165 | 1.160 | 0.298 | 4.151 | 0.737 |
| Model2 (1994-1998) | 1.227 | 0.303 | 2.729 | 0.199 | 1.103 | 0.305 | 3.581 | 0.525 |
| Model3 (1999-2003) | 1.362 | 0.310 | 2.696 | 0.206 | 1.041 | 0.305 | 5.277 | 0.791 |
| Model4 (2004-2008) | 1.554 | 0.406 | 2.840 | 0.318 | 0.986 | 0.321 | 3.568 | 0.521 |
| Model5 (2009-2013) | 1.966 | 0.404 | 2.531 | 0.249 | 1.127 | 0.312 | 4.616 | 0.673 |
Observed values are mean crude incidence rates of subdistricts.
Parameter estimates used to calculate posterior statistics for mapping
| Model . | αy . | αz . | β . | φ . | ||||
|---|---|---|---|---|---|---|---|---|
| . | Mean . | SD . | Mean . | SD . | Mean . | SD . | Mean . | SD . |
| Model1 (1989-1993) | 0.768 | 0.266 | 2.610 | 0.165 | 1.160 | 0.298 | 4.151 | 0.737 |
| Model2 (1994-1998) | 1.227 | 0.303 | 2.729 | 0.199 | 1.103 | 0.305 | 3.581 | 0.525 |
| Model3 (1999-2003) | 1.362 | 0.310 | 2.696 | 0.206 | 1.041 | 0.305 | 5.277 | 0.791 |
| Model4 (2004-2008) | 1.554 | 0.406 | 2.840 | 0.318 | 0.986 | 0.321 | 3.568 | 0.521 |
| Model5 (2009-2013) | 1.966 | 0.404 | 2.531 | 0.249 | 1.127 | 0.312 | 4.616 | 0.673 |
| Model . | αy . | αz . | β . | φ . | ||||
|---|---|---|---|---|---|---|---|---|
| . | Mean . | SD . | Mean . | SD . | Mean . | SD . | Mean . | SD . |
| Model1 (1989-1993) | 0.768 | 0.266 | 2.610 | 0.165 | 1.160 | 0.298 | 4.151 | 0.737 |
| Model2 (1994-1998) | 1.227 | 0.303 | 2.729 | 0.199 | 1.103 | 0.305 | 3.581 | 0.525 |
| Model3 (1999-2003) | 1.362 | 0.310 | 2.696 | 0.206 | 1.041 | 0.305 | 5.277 | 0.791 |
| Model4 (2004-2008) | 1.554 | 0.406 | 2.840 | 0.318 | 0.986 | 0.321 | 3.568 | 0.521 |
| Model5 (2009-2013) | 1.966 | 0.404 | 2.531 | 0.249 | 1.127 | 0.312 | 4.616 | 0.673 |
Observed values are mean crude incidence rates of subdistricts.
Comparison between estimated parameters and observed values for the incidence variable in each 5-year period model
| Model . | Incidence variable z . | |
|---|---|---|
| . | Estimated . | Observed . |
| . | µ . | mean (zi) . |
| Model1(1989-1993) | 13.595 | 14.636 |
| Model2(1994-1998) | 15.318 | 16.912 |
| Model3(1999-2003) | 14.820 | 16.298 |
| Model4(2004-2008) | 17.118 | 17.477 |
| Model5(2009-2013) | 12.566 | 15.232 |
| Model . | Incidence variable z . | |
|---|---|---|
| . | Estimated . | Observed . |
| . | µ . | mean (zi) . |
| Model1(1989-1993) | 13.595 | 14.636 |
| Model2(1994-1998) | 15.318 | 16.912 |
| Model3(1999-2003) | 14.820 | 16.298 |
| Model4(2004-2008) | 17.118 | 17.477 |
| Model5(2009-2013) | 12.566 | 15.232 |
Comparison between estimated parameters and observed values for the incidence variable in each 5-year period model
| Model . | Incidence variable z . | |
|---|---|---|
| . | Estimated . | Observed . |
| . | µ . | mean (zi) . |
| Model1(1989-1993) | 13.595 | 14.636 |
| Model2(1994-1998) | 15.318 | 16.912 |
| Model3(1999-2003) | 14.820 | 16.298 |
| Model4(2004-2008) | 17.118 | 17.477 |
| Model5(2009-2013) | 12.566 | 15.232 |
| Model . | Incidence variable z . | |
|---|---|---|
| . | Estimated . | Observed . |
| . | µ . | mean (zi) . |
| Model1(1989-1993) | 13.595 | 14.636 |
| Model2(1994-1998) | 15.318 | 16.912 |
| Model3(1999-2003) | 14.820 | 16.298 |
| Model4(2004-2008) | 17.118 | 17.477 |
| Model5(2009-2013) | 12.566 | 15.232 |
Spatial and temporal mapping of cervical cancer incidence in Songkhla for each 5-year period on a Cartesian coordinate system.
Discussion
Here, we report spatiotemporal patterns of cervical cancer incidence across Songkhla, Thailand. We found that predominantly Muslim districts have consistently lower incidence rates of cervical cancer and that Sadao, Hat Yai and the juncture between Mueang Songkhla and Singha Nakhon have the highest rates of cervical cancer in Songkhla over time.
The increases in incidence before 2003 are likely due to the occasional campaigns of cervical cancer screening since the nationally organized cervical screening program was implemented in Songkhla in 2004. After implementation, health centres and governmental hospitals were assigned target populations of women ages 35–60 years in their district, for screening once every 5 years. Thus, screening activities remained continuous and fluctuation in incidence rates was reduced. These results conform closely with previous findings (Sriplung et al. 2014b).
The reason behind the high incidence at the juncture between Mueang Songkhla and Singhanakhon is unclear, however, the high incidence rates in Sadao and Hat Yai is likely explained by the main road to Malaysia, which runs across these two areas and has frequent commercial sex trade (Wongboonsin et al. 2008). This area is known for its tourism; the immigration checkpoint in Sadao has seen a steady increase in traffic since 2001 (Wongboonsin et al. 2008). During this time, there was also an increase in immigration of workers from other regions in Thailand searching for jobs, including sex services, due to low wages, low agricultural productivity and high unemployment in their places of origin (Wongboonsin et al. 2008). Commercial sex trade provided higher wages and better employment opportunities. In terms of public health, sex workers had access to the public health care system, including services such as medical check-ups, blood testing and free condoms (Wongboonsin et al. 2008). Although the presence of human papilloma virus (HPV) testing is not currently implemented, increased sexual behaviour is associated with high HPV prevalence, which is an etiologic factor for cervical cancer (Bosch and de Sanjose 2003). Despite public health programs, the level of condom use by female sex workers in Thailand brothels is low, especially when patrons are foreign Asians and native Thai men (Buckingham et al. 2005). This is relevant as male condoms have been shown to effectively reduce the risk of male-to-female genital HPV transmission (Winer et al. 2006). Low adherence to condom use occurred in spite of official campaigns by local public health offices mandating condom use in brothels and an agreement between the public health office in the area and entertainment venues to bring service workers for medical check-up at least once a month. This high-risk behaviour was found to be exacerbated when combined with drug use (Wongboonsin et al. 2008). These factors may explain the potential behavioural and social determinants that drive our findings.
It is important to note, however, that our methods were not designed to test an association between cervical cancer incidence and sex workers specifically, and it is likely that unobserved confounders may play a role our findings. Therefore, further studies should focus on cervical cancer incidence in this vulnerable population to understand specific mechanisms that may be driving the increased prevalence, and assess cervical cancer risk in female sex workers, to provide evidence for potential changes in screening policies. Particularly, screening coverage in these two subdistricts should be carefully monitored and adapted to this vulnerable population. For example, female sex workers could be screened more frequently than once every 5 years and not be limited to the age restriction for the current screening policy in Thailand. Our findings showed that in every 5-year period, cervical cancer incidences among predominantly Muslim districts were lower than among predominantly Buddhist districts. Similar trends were seen in other cancers (Sriplung et al. 2014a), indicating there might be divergent risk factors in these two subpopulations. Future studies should focus on identification of these risk factors to inform prevention strategies.
Smoothing permits easy visualization of the underlying geographic pattern of the disease through omission of administrative boundaries, which may obscure trends. In addition, smoothing omits boundary effects, which shape screening activities, especially in earlier periods, when economic development and health resources were not balanced among subdistricts. Overlaying administrative boundaries on the geographic patterns is informative in discerning where public responsibility lies for screening implementation. The incidence rates during screening were dependent on health care providers, which are associated with administrative boundaries. In consideration of this point, variation of incidence among subdistricts is not surprising.
Overall, incidence rates are continuously decreasing due to higher coverage of cervical cancer screening and better utilization of health care facilities. The goal of cervical cancer incidence in Songkhla province is to be under 10 per 105 person-years by the year 2030. To achieve this, the systematic screening program in the province must be consistently maintained with a focus on high screening coverage across all subdistricts in Songkhla province.
Conclusion
Utilization of spatiotemporal analyses with cancer incidence rates from all provinces in Thailand will allow assessment of the cervical cancer screening program on a national basis and provide evidence for policy changes that can address gaps in coverage. As shown here, spatiotemporal analyses are useful in determining areas for targeted prevention within the current context of the national screening program. Commercial sex workers were identified as a vulnerable population and should be screened more frequently than once every 5 years. In addition, they should not be limited to the age restriction for the current screening policy in Thailand.
Acknowledgement
This work was supported by Fogarty International Center (04R25TW009345).
Ethical approval
Thai Ethics Research Committee (REC 58-013-18-1).
Conflict of interest statement. None declared.
References
Office of the National Economic and Social Development Board of Thailand. 2013. Population Projections for Thailand 2553-2573. http://www.nesdb.go.th/, accessed 6 May 2013.