-
PDF
- Split View
-
Views
-
Cite
Cite
Peipei Zhang, Lianyi Zhao, Jing Liang, Yan Qiao, Quanyan He, Liuyi Zhang, Fang Wang, Yuan Liang, Societal determination of usefulness and utilization wishes of community health services: a population-based survey in Wuhan city, China, Health Policy and Planning, Volume 30, Issue 10, December 2015, Pages 1243–1250, https://doi.org/10.1093/heapol/czu128
Close - Share Icon Share
Abstract
Background As a developing country with the world’s largest population in a state of economic transition, reforms to China’s health system, including community health services (CHS), are very complex and difficult. The aim of this study is to provide evidence and policy recommendations for the sustainable development of CHS for China, which could also be applicable to other developing countries.
Methods A cross-sectional survey was conducted door-to-door and face-to-face in Wuhan city, central China with a sample of 1134 individuals aged 15 and older. The independent variables were duration of residence, previous treatment experience, familiarity with health staff, self-reported family economic status and health insurance. The dependent variables were views on the usefulness of CHS and willingness to use them. Sociodemographic variables and health status were used as control variables. Multiple logistic regression analysis was used to analyse the influence of the independent variables on the dependent variables.
Findings This study shows that 26.10% of participants reported that the CHSs are not useful and 37.74% reported they did not want to use their CHS. The results found ‘familiarity with health staff’ and ‘previous experience of using services’ had a negative influence on their views on usefulness of and willingness to use CHS.
Conclusion The aim of CHS to see ‘minor illnesses treated in the community and serious illness treated in hospital’ is not being fully realized. The key to increasing the use of CHS may be to enhance the quality of services and health staff. A policy pathway of targeting older residents and those with higher education levels as the priority population, and using these groups to encourage the rest of the community to seek minor services at CHS, may be an effective and sustainable development mechanism.
The aim of CHS to see ‘minor illnesses treated in the community and serious illness treated in hospital’ is not being fully realized.
The key to increasing the use of CHS may be to enhance the quality of services and health staff.
A policy pathway of targeting older residents and those with higher education levels as the priority population, and using these groups to encourage the rest of the community to seek minor services at CHS, may be an effective and sustainable development mechanism.
Background
Community health services (CHS) are a relatively new concept in China. CHSs were first officially implemented in China in 1997 as a response to concerns over primary healthcare (Liu and David 2007; Bhattacharyya et al. 2011; Yu et al. 2011). With the establishment of CHS, health policymakers hoped to encourage residents to visit their doctor with the aim of seeing ‘minor illnesses treated in the CHS and serious illnesses treated in hospital’. Many people in China feel that seeing a doctor is both difficult and expensive (Akin et al. 2005; Liu et al. 2007; Li et al. 2012). The establishment of CHS was also an important measure to resolve the difficulties and expense of seeing a doctor. In February 2006, China’s State Council published its ‘Guidelines for the Development of the Urban Community Health Service’, declaring that China would create a basic urban CHS system by 2010. These guidelines and goals were accompanied by extensive and complex healthcare reforms 2009–11; instigated by the State Council in April 2009 (The Central People’s Government, PRC 2006; The Central People’s Government, PRC 2009). Together, these set China on the path to a strong system of primary healthcare based on urban CHS and rural township hospitals.
For more than 10 years now, CHSs in China have experienced rapid development. According to the Statistical Information Center of the Ministry of Health, by the end of February 2013, China has established 33 748 CHS agencies (including CHS departments and centres; Statistical Information Center of National Health and Family Planning Commission, PRC 2013). Although the number of CHS centres has grown rapidly, CHS do not appear to be as effective as hoped (Pan et al. 2006; Yang and Yang 2009; Dib et al. 2010). CHS centres could meet the health needs of the majority of residents; however, most residents still go to hospitals for both minor and serious illnesses. Because of differences in regional economic development and CHS progress, there are significant differences in the use of CHS, with recent research showing a low level of use in many areas. For example, a longitudinal study in Guangzhou, southern China showed that although the proportion of residents visiting a CHS centre for the first time is increasing (from 3.2% in 2004 to 7.9% in 2008), overall usage rates remain low (Li et al. 2010). At the same time, many are not willing to use CHS. For example, according to a population-based survey in Changsha, central China, only 33.53% were willing to use CHS (Guo et al. 2008). These low usage rates show that China’s CHS are not meeting the aims of the policymakers. We therefore need to identify the factors that influence CHS usage and determine how we can improve them.
Although there are several studies on the factors influencing health service use (HSU; Friedman et al. 2013), there are very few factors that influence the use of CHS. It is interesting to note that although Andersen’s Behavior Model has been used extensively to analyse what influences HSU, a recent systematic review of the model found that only a small common set of variables was used and that there were huge variations within the variables category, especially concerning their predisposing and enabling factors (Babitsch et al. 2012). An in-depth study is urgently required to further our understanding of HSU. In China, the factors influencing use of CHS include age, culture, family economic status, health status, quality of service and residents’ attitudes towards CHS (Li et al. 2007; Yang and Yang 2009; Shen et al. 2010). However, most of the existing studies on these factors in China did not use Andersen’s Behavioral Model. More importantly, according to biopsychosocial medical models, the factors influencing health must be extended from an individual level to a societal level (Engel 1977; Mechanic 2007). Such an extension is therefore required to determine the factors influencing CHS use. To our knowledge, there is little research into those factors (both societal and individual) that affect the use of CHS and wider health services.
To address this problem, this study provides an empirical view based on a population-based survey in Wuhan, central China. To determine the usefulness of CHS, and people’s willingness to use them, we focused on the influence of five societal determinations: duration of residence, previous treatment experience, familiarity with health staff, family economic status and health insurance. The aim of the study was to provide evidence and policy recommendations about the sustainable development of CHS in China. As a developing country with the world’s largest population, in a stage of economic transition, reforms to China’s health system, including CHS, are complex and difficult. China’s experience, whether a success or failure, will serve an important point of reference for other developing countries.
Methods
Participants
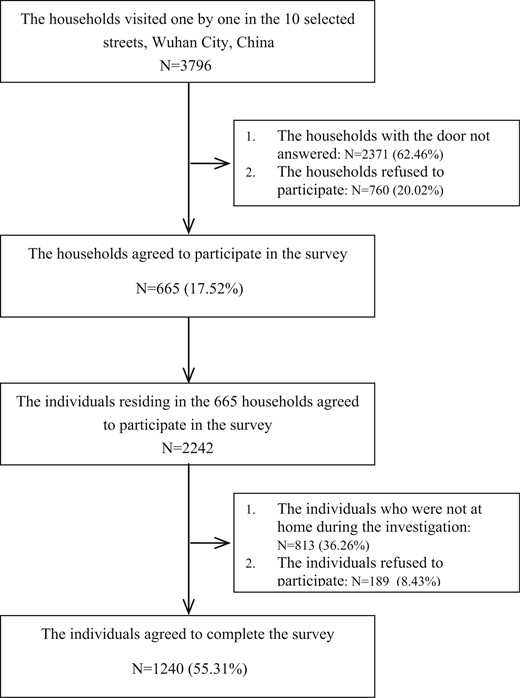
A cross-sectional survey was used in this study, and it was conducted door-to-door in selected areas and face-to-face with participants. Data were collected from May 2010 to August 2011. The study population was community residents who were at least 15 years old and above in Wuhan, the capital of Hubei Province, central China. We used stratified cluster sampling in seven administrative districts in Wuhan (Jiang’an, Hanjiang, Qiaokou, Hangyang, Wuchang, Qingshan and Hongshan). Five districts were selected, Jiang’an, Qiaokou, Hangyang, Qingshan and Hongshan, and then two streets were chosen from each district using purposive sampling by size and population distribution. In the 10 selected streets, all households were visited one by one. Figure 1 shows the flowchart for recruitment and response rates. In total, 3796 households were visited. The door was not answered in 2371 households (62.46%) and 760 households (20.02%) refused to participate. As a result, 665 households (17.52%) participated in the survey. Of the 2242 individuals residing in the 665 households, 1240 (55.31%) agreed to complete the survey. The final sample was 1134 (91.45%) because some questionnaires contained missing data.
Measures
Independent variables
The independent variables were duration of residence, previous treatment experience, familiarity with health staff, self-reported family economic status and health insurance. Duration of residence was surveyed by asking: ‘How long have you been living in the current community?’, to which participants could respond: 0–4 years, 5–9 years and 10 years or more. Familiarity with health staff was surveyed by asking: ‘How many of the health staff (doctors/nurses) do you know at the CHS in your community?’ Participants could choose from the following response options: 0, 1–2, 3–4 and 5 or more. Previous treatment experience was surveyed by asking: ‘Have you seen the doctor at the CHS in your community in the last year?’, and participants could respond either ‘yes’ or ‘no’. Self-reported family economic status was described by participants as ‘bad’, ‘fair’ or ‘good’, and participants answered ‘yes’ or ‘no’ to whether they had health insurance.
Dependent variable and control variables
The dependent variables were participants’ views on the usefulness of CHS and their willingness to use them. The usefulness of CHS was surveyed by asking: ‘How useful is the CHS?’ Participants responded with one of ‘not useful’, ‘neither useful nor not useful’ and ‘useful’. The willingness to use CHS was surveyed by asking: ‘Are you willing to visit the doctor at your CHS?’ Participants responded with ‘not willing’, ‘neither willing nor unwilling’ or ‘willing’. Sociodemographic variables, which included gender, age, education, marital status and health status (prevalence of doctor-diagnosed hypertension and self-reported illness in the last 2 weeks, namely 2-week prevalence) were used as control variables.
Statistical Analysis
Descriptive analysis was carried out for the primary variables. Logistic regression analysis was used to analyse influence factors. We used two models to observe the effect of independent variables. In the first model, we added only the independent variables, including time living the community, previous treatment experience, the number of the health staff known, family economic status and health insurance. In the second model, we added potential confounding variables. Adjusted OR and 95% confidence interval (CI) were calculated using logistic regression. For all comparisons, differences were tested using two-tailed tests and P values <0.05 were considered statistically significant. All statistical procedures were performed using the Statistical Package for Social Sciences Version 12.0 (SPSS Inc., Chicago, IL, USA) for Windows.
Results
Table 1 presents the distribution characteristics of the research variables. In total, 26.10% of participants reported that their CHS was not useful, and 37.74% reported that they did not want to use them. The majority (67.99%) of participants had lived in their current community for 10 years or more. Only 31.39% had previous experience of using the CHS. Almost two-thirds of the participants, 62.70%, were female, perhaps because more males were at work when residents were approached to take part in the survey. The survey also found that 25.00% of participants had hypertension, which is consistent with results from a 2008 China National Health Services Survey.
Descriptive statistics of the primary variables (n = 1134)
| Variables . | N . | % . |
|---|---|---|
| Dependent variables | ||
| Usefulness of CHS | ||
| Not useful | 296 | 26.10 |
| Neither useful nor not useful | 235 | 20.72 |
| Useful | 603 | 53.17 |
| Utilization wishes of CHS | ||
| Not willing | 428 | 37.74 |
| Neither willing nor unwilling | 115 | 10.14 |
| Willing | 591 | 52.12 |
| Independent variables | ||
| Duration of residence | ||
| 0–4 | 190 | 16.75 |
| 5–9 | 173 | 15.26 |
| 10 years and above | 771 | 67.99 |
| Previous treatment experience | ||
| Yes | 356 | 31.39 |
| No | 778 | 68.61 |
| The number of the health staff known | ||
| 0 | 726 | 64.02 |
| 1–2 | 260 | 22.93 |
| 3–4 | 105 | 9.26 |
| 5 and above | 43 | 3.79 |
| Self-reported family economic status | ||
| Bad | 167 | 14.73 |
| Fair | 653 | 57.58 |
| Good | 314 | 27.69 |
| Health insurance | ||
| Yes | 877 | 77.82 |
| No | 250 | 22.18 |
| Potential confounding variables | ||
| Gender | ||
| Male | 423 | 37.30 |
| Female | 711 | 62.70 |
| Age | ||
| 15–44 | 355 | 31.31 |
| 45–59 | 342 | 30.16 |
| 60 and above | 437 | 38.54 |
| Education | ||
| Primary and below | 193 | 17.02 |
| Junior school | 337 | 29.72 |
| High School | 377 | 33.25 |
| College and above | 227 | 20.02 |
| Marital status | ||
| Never married | 96 | 8.47 |
| Divorced/widowed | 154 | 13.58 |
| Married/remarried | 884 | 77.95 |
| Ethnicity | ||
| Han nationality | 1116 | 99.47 |
| Others | 6 | 0.53 |
| 2-week prevalence | ||
| Yes | 303 | 26.72 |
| No | 831 | 73.28 |
| Hypertension | ||
| Yes | 283 | 25.00 |
| No | 849 | 75.00 |
| Variables . | N . | % . |
|---|---|---|
| Dependent variables | ||
| Usefulness of CHS | ||
| Not useful | 296 | 26.10 |
| Neither useful nor not useful | 235 | 20.72 |
| Useful | 603 | 53.17 |
| Utilization wishes of CHS | ||
| Not willing | 428 | 37.74 |
| Neither willing nor unwilling | 115 | 10.14 |
| Willing | 591 | 52.12 |
| Independent variables | ||
| Duration of residence | ||
| 0–4 | 190 | 16.75 |
| 5–9 | 173 | 15.26 |
| 10 years and above | 771 | 67.99 |
| Previous treatment experience | ||
| Yes | 356 | 31.39 |
| No | 778 | 68.61 |
| The number of the health staff known | ||
| 0 | 726 | 64.02 |
| 1–2 | 260 | 22.93 |
| 3–4 | 105 | 9.26 |
| 5 and above | 43 | 3.79 |
| Self-reported family economic status | ||
| Bad | 167 | 14.73 |
| Fair | 653 | 57.58 |
| Good | 314 | 27.69 |
| Health insurance | ||
| Yes | 877 | 77.82 |
| No | 250 | 22.18 |
| Potential confounding variables | ||
| Gender | ||
| Male | 423 | 37.30 |
| Female | 711 | 62.70 |
| Age | ||
| 15–44 | 355 | 31.31 |
| 45–59 | 342 | 30.16 |
| 60 and above | 437 | 38.54 |
| Education | ||
| Primary and below | 193 | 17.02 |
| Junior school | 337 | 29.72 |
| High School | 377 | 33.25 |
| College and above | 227 | 20.02 |
| Marital status | ||
| Never married | 96 | 8.47 |
| Divorced/widowed | 154 | 13.58 |
| Married/remarried | 884 | 77.95 |
| Ethnicity | ||
| Han nationality | 1116 | 99.47 |
| Others | 6 | 0.53 |
| 2-week prevalence | ||
| Yes | 303 | 26.72 |
| No | 831 | 73.28 |
| Hypertension | ||
| Yes | 283 | 25.00 |
| No | 849 | 75.00 |
Descriptive statistics of the primary variables (n = 1134)
| Variables . | N . | % . |
|---|---|---|
| Dependent variables | ||
| Usefulness of CHS | ||
| Not useful | 296 | 26.10 |
| Neither useful nor not useful | 235 | 20.72 |
| Useful | 603 | 53.17 |
| Utilization wishes of CHS | ||
| Not willing | 428 | 37.74 |
| Neither willing nor unwilling | 115 | 10.14 |
| Willing | 591 | 52.12 |
| Independent variables | ||
| Duration of residence | ||
| 0–4 | 190 | 16.75 |
| 5–9 | 173 | 15.26 |
| 10 years and above | 771 | 67.99 |
| Previous treatment experience | ||
| Yes | 356 | 31.39 |
| No | 778 | 68.61 |
| The number of the health staff known | ||
| 0 | 726 | 64.02 |
| 1–2 | 260 | 22.93 |
| 3–4 | 105 | 9.26 |
| 5 and above | 43 | 3.79 |
| Self-reported family economic status | ||
| Bad | 167 | 14.73 |
| Fair | 653 | 57.58 |
| Good | 314 | 27.69 |
| Health insurance | ||
| Yes | 877 | 77.82 |
| No | 250 | 22.18 |
| Potential confounding variables | ||
| Gender | ||
| Male | 423 | 37.30 |
| Female | 711 | 62.70 |
| Age | ||
| 15–44 | 355 | 31.31 |
| 45–59 | 342 | 30.16 |
| 60 and above | 437 | 38.54 |
| Education | ||
| Primary and below | 193 | 17.02 |
| Junior school | 337 | 29.72 |
| High School | 377 | 33.25 |
| College and above | 227 | 20.02 |
| Marital status | ||
| Never married | 96 | 8.47 |
| Divorced/widowed | 154 | 13.58 |
| Married/remarried | 884 | 77.95 |
| Ethnicity | ||
| Han nationality | 1116 | 99.47 |
| Others | 6 | 0.53 |
| 2-week prevalence | ||
| Yes | 303 | 26.72 |
| No | 831 | 73.28 |
| Hypertension | ||
| Yes | 283 | 25.00 |
| No | 849 | 75.00 |
| Variables . | N . | % . |
|---|---|---|
| Dependent variables | ||
| Usefulness of CHS | ||
| Not useful | 296 | 26.10 |
| Neither useful nor not useful | 235 | 20.72 |
| Useful | 603 | 53.17 |
| Utilization wishes of CHS | ||
| Not willing | 428 | 37.74 |
| Neither willing nor unwilling | 115 | 10.14 |
| Willing | 591 | 52.12 |
| Independent variables | ||
| Duration of residence | ||
| 0–4 | 190 | 16.75 |
| 5–9 | 173 | 15.26 |
| 10 years and above | 771 | 67.99 |
| Previous treatment experience | ||
| Yes | 356 | 31.39 |
| No | 778 | 68.61 |
| The number of the health staff known | ||
| 0 | 726 | 64.02 |
| 1–2 | 260 | 22.93 |
| 3–4 | 105 | 9.26 |
| 5 and above | 43 | 3.79 |
| Self-reported family economic status | ||
| Bad | 167 | 14.73 |
| Fair | 653 | 57.58 |
| Good | 314 | 27.69 |
| Health insurance | ||
| Yes | 877 | 77.82 |
| No | 250 | 22.18 |
| Potential confounding variables | ||
| Gender | ||
| Male | 423 | 37.30 |
| Female | 711 | 62.70 |
| Age | ||
| 15–44 | 355 | 31.31 |
| 45–59 | 342 | 30.16 |
| 60 and above | 437 | 38.54 |
| Education | ||
| Primary and below | 193 | 17.02 |
| Junior school | 337 | 29.72 |
| High School | 377 | 33.25 |
| College and above | 227 | 20.02 |
| Marital status | ||
| Never married | 96 | 8.47 |
| Divorced/widowed | 154 | 13.58 |
| Married/remarried | 884 | 77.95 |
| Ethnicity | ||
| Han nationality | 1116 | 99.47 |
| Others | 6 | 0.53 |
| 2-week prevalence | ||
| Yes | 303 | 26.72 |
| No | 831 | 73.28 |
| Hypertension | ||
| Yes | 283 | 25.00 |
| No | 849 | 75.00 |
Table 2 displays the odds ratios (OR) for associations between the independent variables and the usefulness of and willingness to use the CHS. Model 1 shows that previous treatment experience and familiarity with health staff were statistically significant (OR: 0.57, CI: 0.44–0.75; OR: 0.31, CI: 0.21–0.47, respectively) and had a negative influence on participants’ views of the usefulness of CHS. In Model 2, previous treatment experience, familiarity with health staff and education remained statistically significant, showing a negative influence (OR: 0.53, CI: 0.41–0.70; OR: 0.30, CI: 0.20–0.46; OR: 2.23, CI: 1.40–3.53; respectively). Similarly, previous treatment experience and familiarity with health staff were significantly associated with willingness to use CHS in both models. The potential confounding variables, education and illness in the previous 2 weeks, were found to be statistically significant regarding views on the usefulness of CHS, as were age and illness in the previous 2 weeks on willingness to use CHS (OR: 1.68, 95% CI: 1.12–2.52; OR: 1.44, 95% CI: 1.07–1.93; respectively).
The effects of societal determination on usefulness and utilization wishes of CHS (OR, 95% CI; n = 1134)
| Variables . | Usefulness of CHS . | Utilization wishes of CHS . | ||
|---|---|---|---|---|
| Model 1 . | Model 2 . | Model 1 . | Model 2 . | |
| Independent variables | ||||
| Duration of residence | ||||
| 10 years and above | 1.14(0.83,1.56) | 1.16(0.83,1.64) | 0.92(0.66,1.29) | 0.85(0.59,1.22) |
| 5–9 | 1.22(0.82,1.84) | 1.28(0.85,1.91) | 1.08(0.70,1.66) | 1.05(0.68,1.62) |
| 0–4 | 1.00 | 1.00 | 1.00 | 1.00 |
| Previous treatment experience | ||||
| Yes | 0.57(0.44,0.75)*** | 0.53(0.41,0.70)*** | 0.19(0.14,0.26)*** | 0.17(0.13,0.24)*** |
| No | 1.00 | 1.00 | 1.00 | 1.00 |
| Number of the health staff known | ||||
| 3 and above | 0.31(0.21,0.47)*** | 0.30(0.20,0.46)*** | 0.25(0.16,0.40)*** | 0.24(0.15,0.38)*** |
| 1–2 | 0.46(0.34,0.61)*** | 0.44(0.32,0.59)*** | 0.34(0.25,0.47)*** | 0.32(0.23,0.45)*** |
| 0 | 1.00 | 1.00 | 1.00 | 1.00 |
| Self-reported family economic status | ||||
| Good | 1.04(0.72,1.50) | 1.04(0.71,1.52) | 0.91(0.61,1.36) | 0.92(0.61,1.39) |
| Fair | 1.04(0.74,1.46) | 1.09(0.77,1.54) | 0.98(0.68,1.41) | 1.02(0.70,1.47) |
| Bad | 1.00 | 1.00 | 1.00 | 1.00 |
| Health insurance | ||||
| Yes | 1.07(0.81,1.41) | 0.99(0.74,1.32) | 1.18(0.88,1.59) | 1.08(0.79,1.47) |
| No | 1.00 | 1.00 | 1.00 | 1.00 |
| Potential confounding variables | ||||
| Gender | ||||
| Male | 0.95(0.74,1.22) | 0.84(0.64,1.10) | ||
| Female | 1.00 | 1.00 | ||
| Age | ||||
| 60 and above | 1.44(0.99,2.08) | 1.68(1.12,2.52)* | ||
| 45–59 | 0.951(0.670,1.350) | 1.30(0.90,1.89) | ||
| 15–44 | 1.00 | 1.00 | ||
| Education | ||||
| College and above | 2.23(1.40,3.53)* | 1.64(0.99,2.69) | ||
| High school | 1.86(1.23,2.83)** | 1.23(0.79,1.92) | ||
| Junior school | 1.55(1.05,2.30)*** | 0.93(0.61,1.42) | ||
| Primary and below | 1.00 | 1.00 | ||
| Marital status | ||||
| Married/remarried | 0.74(0.47,1.17) | 1.17(0.62,2.20) | ||
| Divorced/widowed | 0.89(0.50,1.60) | 0.96(0.59,1.560) | ||
| Never married | 1.00 | 1.00 | ||
| 2-week prevalence | ||||
| Yes | 1.64(1.25,2.15)*** | 1.44(1.07,1.93)* | ||
| No | 1.00 | 1.00 | ||
| Hypertension | ||||
| Yes | 1.11(0.82,1.48) | 1.04(0.76,1.43) | ||
| No | 1.00 | 1.00 | ||
| Variables . | Usefulness of CHS . | Utilization wishes of CHS . | ||
|---|---|---|---|---|
| Model 1 . | Model 2 . | Model 1 . | Model 2 . | |
| Independent variables | ||||
| Duration of residence | ||||
| 10 years and above | 1.14(0.83,1.56) | 1.16(0.83,1.64) | 0.92(0.66,1.29) | 0.85(0.59,1.22) |
| 5–9 | 1.22(0.82,1.84) | 1.28(0.85,1.91) | 1.08(0.70,1.66) | 1.05(0.68,1.62) |
| 0–4 | 1.00 | 1.00 | 1.00 | 1.00 |
| Previous treatment experience | ||||
| Yes | 0.57(0.44,0.75)*** | 0.53(0.41,0.70)*** | 0.19(0.14,0.26)*** | 0.17(0.13,0.24)*** |
| No | 1.00 | 1.00 | 1.00 | 1.00 |
| Number of the health staff known | ||||
| 3 and above | 0.31(0.21,0.47)*** | 0.30(0.20,0.46)*** | 0.25(0.16,0.40)*** | 0.24(0.15,0.38)*** |
| 1–2 | 0.46(0.34,0.61)*** | 0.44(0.32,0.59)*** | 0.34(0.25,0.47)*** | 0.32(0.23,0.45)*** |
| 0 | 1.00 | 1.00 | 1.00 | 1.00 |
| Self-reported family economic status | ||||
| Good | 1.04(0.72,1.50) | 1.04(0.71,1.52) | 0.91(0.61,1.36) | 0.92(0.61,1.39) |
| Fair | 1.04(0.74,1.46) | 1.09(0.77,1.54) | 0.98(0.68,1.41) | 1.02(0.70,1.47) |
| Bad | 1.00 | 1.00 | 1.00 | 1.00 |
| Health insurance | ||||
| Yes | 1.07(0.81,1.41) | 0.99(0.74,1.32) | 1.18(0.88,1.59) | 1.08(0.79,1.47) |
| No | 1.00 | 1.00 | 1.00 | 1.00 |
| Potential confounding variables | ||||
| Gender | ||||
| Male | 0.95(0.74,1.22) | 0.84(0.64,1.10) | ||
| Female | 1.00 | 1.00 | ||
| Age | ||||
| 60 and above | 1.44(0.99,2.08) | 1.68(1.12,2.52)* | ||
| 45–59 | 0.951(0.670,1.350) | 1.30(0.90,1.89) | ||
| 15–44 | 1.00 | 1.00 | ||
| Education | ||||
| College and above | 2.23(1.40,3.53)* | 1.64(0.99,2.69) | ||
| High school | 1.86(1.23,2.83)** | 1.23(0.79,1.92) | ||
| Junior school | 1.55(1.05,2.30)*** | 0.93(0.61,1.42) | ||
| Primary and below | 1.00 | 1.00 | ||
| Marital status | ||||
| Married/remarried | 0.74(0.47,1.17) | 1.17(0.62,2.20) | ||
| Divorced/widowed | 0.89(0.50,1.60) | 0.96(0.59,1.560) | ||
| Never married | 1.00 | 1.00 | ||
| 2-week prevalence | ||||
| Yes | 1.64(1.25,2.15)*** | 1.44(1.07,1.93)* | ||
| No | 1.00 | 1.00 | ||
| Hypertension | ||||
| Yes | 1.11(0.82,1.48) | 1.04(0.76,1.43) | ||
| No | 1.00 | 1.00 | ||
Note: <0.05, *; <0.01, **; <0.001, ***.
The effects of societal determination on usefulness and utilization wishes of CHS (OR, 95% CI; n = 1134)
| Variables . | Usefulness of CHS . | Utilization wishes of CHS . | ||
|---|---|---|---|---|
| Model 1 . | Model 2 . | Model 1 . | Model 2 . | |
| Independent variables | ||||
| Duration of residence | ||||
| 10 years and above | 1.14(0.83,1.56) | 1.16(0.83,1.64) | 0.92(0.66,1.29) | 0.85(0.59,1.22) |
| 5–9 | 1.22(0.82,1.84) | 1.28(0.85,1.91) | 1.08(0.70,1.66) | 1.05(0.68,1.62) |
| 0–4 | 1.00 | 1.00 | 1.00 | 1.00 |
| Previous treatment experience | ||||
| Yes | 0.57(0.44,0.75)*** | 0.53(0.41,0.70)*** | 0.19(0.14,0.26)*** | 0.17(0.13,0.24)*** |
| No | 1.00 | 1.00 | 1.00 | 1.00 |
| Number of the health staff known | ||||
| 3 and above | 0.31(0.21,0.47)*** | 0.30(0.20,0.46)*** | 0.25(0.16,0.40)*** | 0.24(0.15,0.38)*** |
| 1–2 | 0.46(0.34,0.61)*** | 0.44(0.32,0.59)*** | 0.34(0.25,0.47)*** | 0.32(0.23,0.45)*** |
| 0 | 1.00 | 1.00 | 1.00 | 1.00 |
| Self-reported family economic status | ||||
| Good | 1.04(0.72,1.50) | 1.04(0.71,1.52) | 0.91(0.61,1.36) | 0.92(0.61,1.39) |
| Fair | 1.04(0.74,1.46) | 1.09(0.77,1.54) | 0.98(0.68,1.41) | 1.02(0.70,1.47) |
| Bad | 1.00 | 1.00 | 1.00 | 1.00 |
| Health insurance | ||||
| Yes | 1.07(0.81,1.41) | 0.99(0.74,1.32) | 1.18(0.88,1.59) | 1.08(0.79,1.47) |
| No | 1.00 | 1.00 | 1.00 | 1.00 |
| Potential confounding variables | ||||
| Gender | ||||
| Male | 0.95(0.74,1.22) | 0.84(0.64,1.10) | ||
| Female | 1.00 | 1.00 | ||
| Age | ||||
| 60 and above | 1.44(0.99,2.08) | 1.68(1.12,2.52)* | ||
| 45–59 | 0.951(0.670,1.350) | 1.30(0.90,1.89) | ||
| 15–44 | 1.00 | 1.00 | ||
| Education | ||||
| College and above | 2.23(1.40,3.53)* | 1.64(0.99,2.69) | ||
| High school | 1.86(1.23,2.83)** | 1.23(0.79,1.92) | ||
| Junior school | 1.55(1.05,2.30)*** | 0.93(0.61,1.42) | ||
| Primary and below | 1.00 | 1.00 | ||
| Marital status | ||||
| Married/remarried | 0.74(0.47,1.17) | 1.17(0.62,2.20) | ||
| Divorced/widowed | 0.89(0.50,1.60) | 0.96(0.59,1.560) | ||
| Never married | 1.00 | 1.00 | ||
| 2-week prevalence | ||||
| Yes | 1.64(1.25,2.15)*** | 1.44(1.07,1.93)* | ||
| No | 1.00 | 1.00 | ||
| Hypertension | ||||
| Yes | 1.11(0.82,1.48) | 1.04(0.76,1.43) | ||
| No | 1.00 | 1.00 | ||
| Variables . | Usefulness of CHS . | Utilization wishes of CHS . | ||
|---|---|---|---|---|
| Model 1 . | Model 2 . | Model 1 . | Model 2 . | |
| Independent variables | ||||
| Duration of residence | ||||
| 10 years and above | 1.14(0.83,1.56) | 1.16(0.83,1.64) | 0.92(0.66,1.29) | 0.85(0.59,1.22) |
| 5–9 | 1.22(0.82,1.84) | 1.28(0.85,1.91) | 1.08(0.70,1.66) | 1.05(0.68,1.62) |
| 0–4 | 1.00 | 1.00 | 1.00 | 1.00 |
| Previous treatment experience | ||||
| Yes | 0.57(0.44,0.75)*** | 0.53(0.41,0.70)*** | 0.19(0.14,0.26)*** | 0.17(0.13,0.24)*** |
| No | 1.00 | 1.00 | 1.00 | 1.00 |
| Number of the health staff known | ||||
| 3 and above | 0.31(0.21,0.47)*** | 0.30(0.20,0.46)*** | 0.25(0.16,0.40)*** | 0.24(0.15,0.38)*** |
| 1–2 | 0.46(0.34,0.61)*** | 0.44(0.32,0.59)*** | 0.34(0.25,0.47)*** | 0.32(0.23,0.45)*** |
| 0 | 1.00 | 1.00 | 1.00 | 1.00 |
| Self-reported family economic status | ||||
| Good | 1.04(0.72,1.50) | 1.04(0.71,1.52) | 0.91(0.61,1.36) | 0.92(0.61,1.39) |
| Fair | 1.04(0.74,1.46) | 1.09(0.77,1.54) | 0.98(0.68,1.41) | 1.02(0.70,1.47) |
| Bad | 1.00 | 1.00 | 1.00 | 1.00 |
| Health insurance | ||||
| Yes | 1.07(0.81,1.41) | 0.99(0.74,1.32) | 1.18(0.88,1.59) | 1.08(0.79,1.47) |
| No | 1.00 | 1.00 | 1.00 | 1.00 |
| Potential confounding variables | ||||
| Gender | ||||
| Male | 0.95(0.74,1.22) | 0.84(0.64,1.10) | ||
| Female | 1.00 | 1.00 | ||
| Age | ||||
| 60 and above | 1.44(0.99,2.08) | 1.68(1.12,2.52)* | ||
| 45–59 | 0.951(0.670,1.350) | 1.30(0.90,1.89) | ||
| 15–44 | 1.00 | 1.00 | ||
| Education | ||||
| College and above | 2.23(1.40,3.53)* | 1.64(0.99,2.69) | ||
| High school | 1.86(1.23,2.83)** | 1.23(0.79,1.92) | ||
| Junior school | 1.55(1.05,2.30)*** | 0.93(0.61,1.42) | ||
| Primary and below | 1.00 | 1.00 | ||
| Marital status | ||||
| Married/remarried | 0.74(0.47,1.17) | 1.17(0.62,2.20) | ||
| Divorced/widowed | 0.89(0.50,1.60) | 0.96(0.59,1.560) | ||
| Never married | 1.00 | 1.00 | ||
| 2-week prevalence | ||||
| Yes | 1.64(1.25,2.15)*** | 1.44(1.07,1.93)* | ||
| No | 1.00 | 1.00 | ||
| Hypertension | ||||
| Yes | 1.11(0.82,1.48) | 1.04(0.76,1.43) | ||
| No | 1.00 | 1.00 | ||
Note: <0.05, *; <0.01, **; <0.001, ***.
Discussion
To our knowledge, this study is the first to provide empirical data about the societal determinations of views on usefulness of and willingness to use CHS in China. This study shows that 26.10% of participants reported that the CHS are not useful and 37.74% reported they did not want to use their CHS. After adjusting for potential confounding variables, the results of the factors influencing views on usefulness of and willingness to use CHS consistently showed that the effect of both familiarity with health staff and previous experience of the service was negative. That is, the greater the familiarity with health staff at CHS, the more negative the evaluation of usefulness of and willingness to use the service. Compared with participants with no previous experience of CHS, those with prior experience were less willing to use CHS. The aim of CHS to see ‘minor illnesses treated in the community and serious illness treated in hospital’ is not being fully realized.
It is interesting to note the negative effects of familiarity with health staff and previous experience of the services. It is often assumed that familiarity with health staff and previous experience of the services would have a positive effect. However, this was not the case here. Although this study did not investigate how residents perceived the quality of the CHS, existing studies and the media almost unanimously suggest that the poor quality of care and technical capacity of health staff are key barriers in the development of CHS (Yang et al. 2008; Yang and Yang 2009; Hu et al. 2010; Huang and Guo 2011; Zhou et al. 2013). The health staff in CHS in China mainly come from secondary specialized school and lower levels of university. In general, medical students graduating from university would not go to CHS and rural primary hospitals, because these do not offer good economic compensation, career development or social status. These problems are difficult to solve in the short term, which may help us to interpret the negative effect of familiarity with health staff and previous experience of the service. Because participants consider the quality of CHS, and the technical capacity of health staff to be low, they felt that CHSs were not useful and did not want to use them. These results suggest the importance of effective training for health staff and recruitment of talented personnel to increase the use of CHS and its development in China.
There are two possible reasons that duration of residence showed no significant effect on perceptions of CHS. First, the concept of CHS is relatively new in China (the development process started ∼10 years ago), and its progress differs across provinces, largely because of their economic development and urbanization (Pan et al. 2006; Liu and David 2007; Liu et al. 2007; Yang et al. 2008; Hu et al. 2010; Huang and Guo 2011). Although CHSs were first officially implemented in China in 1997, these services in many provinces have a shorter history of CHS. However, duration of residence was often much longer than a decade (67.99% have lived in their community for 10 years or more). In other words, there is a history associated with residency, yet the establishment of CHS is a new concept. It is therefore easy to understand why the impact of duration of residence on the use of CHS is not significant. Second, CHS in China are set by geographical location. Although residents may live in one community, they often work in industries and institutions located in a different community. It could therefore be difficult for health staff and residents to get to know each other. This is another reason why duration of residence has little effect on residents’ use of CHS. It is worth noting that the ‘Hukou’ (household registration system) was not included in this study. Before the Chinese reform and opening-up (since 1979), Hukou was a very important issue, especially for urban residents, and could be linked to employment opportunities and welfare. It was very difficult for rural residents to move from rural to urban Hukou. However, since the reforms and opening-up, especially in the last 10–20 years, the importance of Hukou has been greatly reduced. Nowadays, urban Hukou is related to where someone lives, and a rural resident would get urban Hukou if they bought a house in the city. More importantly, the current rural Hukou is more valuable than its urban equivalent, because residents with rural Hukou can get farm subsidies from the government and rural land use rights. The levels of stigma, prejudice and discrimination from Hukou are therefore weak. We have not found empirical data that shows any association between Hukou and how residents perceive the CHS. The effect of Hukou on the use of CHS would be expected to be weak, because health service usage in China is directly related to money. Patients, whether urban or rural, can freely choose CHS and hospital, as long as they have enough money.
The effect of family economic status was not significant, perhaps because it is related to the out-of-pocket costs of CHS. An important policy aim of CHS is to reduce the difficulties and expense associated with seeing a doctor; CHS fees are relatively low. Therefore, a family’s economic status will not have a significant impact on the use of CHS. It is also worth noting that the effect of health insurance had no statistical significance, which is consistent with the results from the Health Insurance Center of Zhejiang Province, eastern China (Fang 2008). There may be two reasons for this. The first is health insurance policies. Data from the Health Insurance Center in Zhejiang Province showed that 47.5% of participants had an ambiguous attitude towards their current health insurance policy and only 12% were satisfied with it. The second is the quality of CHS. As mentioned earlier, the poor quality of care and health staff are key barriers in the development of CHS. If the quality of CHS is not high, residents will not use CHS, regardless of whether they have health insurance. After all, the aim of seeing a doctor is to resolve health problems and not to reduce costs. In addition, although Hubei and Zhejiang are two different provinces (one in central China and the other in eastern China), they would be comparable, because all the provinces in China are under the unified management of the central government, and inter-provincial policy for health insurance and health service, including CHS, is relatively similar.
The effects of potential confounding variables may provide some valuable clues about how to increase the use of CHS. For example, the effects of 2-week prevalence may remind us that treatment of minor illnesses in the CHS is feasible. The willingness of older residents (aged 60 and above) to use CHS suggests that they could be targeted as the priority population, to increase CHS use in other groups. Policymakers could encourage this group to use CHS, use them as an example and let that guide others towards CHS use (Jiang et al. 2009). A similar effect could also be achieved by targeting those with higher levels of education.
There are a few limitations of this study that must be noted. First, our sample was confined to one city in a central province in China, which may reduce the generalizability of our findings. Second, the response rate was relatively low, which could produce selection bias. CHS staff advised us that the best time to conduct our door-to-door survey was during the weekend (Saturday and Sunday), rather than during the week (Monday to Friday) when people were more likely to be out. However, because of residents’ heightened awareness, it was difficult for us to improve the response rate. In terms of the representativeness of the sample, especially the high proportion not answering the door (62.46%) or refusing to participate (20.02%), we did a pilot survey about the differences of household types between respondents and non-respondents before the formal investigation. The results of the pilot survey are provided in the Supplementary Appendix, and the respondents were shown to be similar to non-respondents in terms of household types. Although the household type might not be the best indicator of whether the sample was representative, it is consistent with current practice for population-based surveys conducted door-to-door and face-to-face in Chinese urban areas, and we could not obtain any demographic characteristics for comparison from those who did not answer the door or refused to participate.
Conclusion
Despite these limitations, this study provides initial evidence of the societal determination of views about usefulness of and willingness to use CHS in China. It suggests two policy implications, which could also be applicable to other developing countries. First, the key to increasing the use of CHS may be improving the quality of services and health staff. The training of health staff may play an important role. Second, the policy aim of that treatment of minor illnesses in CHS is feasible, especially taking into account the effects of illness in the previous 2 weeks, and age and education. It may be helpful to adopt a policy of encourage older residents and those with higher education levels to use CHS, as they are generally more willing to do so. Increased usage from these two groups may encourage the rest of the community to seek services from the CHS for minor illnesses and complaints, which may be an effective and sustainable development mechanism for CHS.
Supplementary Data
Supplementary data are available at HEAPOL online.
Acknowledgements
Each of the listed authors meets each of the three authorship requirements as stated in the Uniform Requirements for Manuscripts Submitted to Biomedical Journals.
Funding
This study was supported by grants from Health Policy Research Fund of Health Bureau of Hubei Province, China (No. ZC2010-8). The funders had no role in study design, data collection and analysis, decision to publish or preparation of the manuscript.
Ethical Approval
The study was approved by the Ethics Committee of School of Public Health, Tongji Medical College, Huazhong University of Science and Technology, Wuhan, China [No. (2010) 02]. Informed consent was obtained from all participants. All residents provided written informed consent with signature or thumbprint.
Conflict of interest: None declared.