-
PDF
- Split View
-
Views
-
Cite
Cite
Stephany M Cox, Jennifer L Butcher, Anjali Sadhwani, Renee Sananes, Jacqueline H Sanz, Elizabeth Blumenfeld, Adam R Cassidy, Jessica C Cowin, Dawn Ilardi, Nadine A Kasparian, Joslyn Kenowitz, Kristin Kroll, Thomas A Miller, Kelly R Wolfe, from the Telehealth Task Force of the Cardiac Neurodevelopmental Outcome Collaborative, Integrating Telehealth Into Neurodevelopmental Assessment: A Model From the Cardiac Neurodevelopmental Outcome Collaborative, Journal of Pediatric Psychology, Volume 47, Issue 6, July 2022, Pages 707–713, https://doi.org/10.1093/jpepsy/jsac003
Close - Share Icon Share
Abstract
In the wake of the COVID-19 pandemic, psychologists were pushed to look beyond traditional in-person models of neurodevelopmental assessment to maintain continuity of care. A wealth of data demonstrates that telehealth is efficacious for pediatric behavioral intervention; however, best practices for incorporating telehealth into neurodevelopmental assessment are yet to be developed. In this topical review, we propose a conceptual model to demonstrate how telehealth can be incorporated into various components of neurodevelopmental assessment.
Harnessing existing literature and expertise from a multidisciplinary task force comprised of clinicians, researchers, and patient/parent representatives from the subspecialty of cardiac neurodevelopmental care, a conceptual framework for telehealth neurodevelopmental assessment was developed. Considerations for health equity and access to care are discussed, as well as general guidelines for clinical implementation and gaps in existing literature.
There are opportunities to integrate telehealth within each stage of neurodevelopmental assessment, from intake to testing, through to follow-up care. Further research is needed to determine whether telehealth mitigates or exacerbates disparities in access to care for vulnerable populations as well as to provide evidence of validity for a wider range of neurodevelopmental measures to be administered via telehealth.
While many practices are returning to traditional, face-to-face neurodevelopmental assessment services, psychologists have a unique opportunity to harness the momentum for telehealth care initiated during the pandemic to optimize the use of clinical resources, broaden service delivery, and increase access to care for pediatric neurodevelopmental assessment.
While research in telehealth dates back to the 1970s, a dramatic acceleration in clinical practice occurred in response to the COVID-19 pandemic (Doraiswamy et al., 2020). Research in adult teleneuropsychology demonstrates validity for remote administration of certain standardized measures such as digit span, list learning, and verbal fluency tasks as well as the Repeatable Battery for the Assessment of Neuropsychological Status (Brearly et al., 2017; Galusha-Glasscock et al., 2016). Nascent research on the feasibility and validity of leveraging telehealth for neurodevelopmental assessment is also promising, including successful utilization of telehealth for triage, consultation (Ransom et al., 2020; Sherwood & MacDonald, 2020), and targeted assessments (Harder et al., 2020; Salinas et al., 2020). Given the seismic shift in clinical practice, development of best practices for incorporating telehealth into neurodevelopmental assessment is needed.
In June 2020, a subgroup of clinicians, clinical researchers, and patient/parent representatives from the Cardiac Neurodevelopmental Outcome Collaborative (CNOC; www.cardiacneuro.org) formed a Telehealth Task Force to facilitate best practices for telehealth cardiac neurodevelopmental care. Extant models have proposed tiers of pediatric assessment based on the patient’s individual risk level (Baum et al., 2017; Hardy et al., 2017). This task force sought to expand this literature by introducing a new model demonstrating how telehealth can be incorporated into neurodevelopmental assessment, understanding that resources, insurance coverage, and legalities vary by practice and location. We present considerations for telehealth neurodevelopmental assessment from infancy through adolescence, illustrated within the subspecialty of cardiac neurodevelopmental care, with the goal of applying this framework to other pediatric specialties. Issues related to establishing standard operating procedures (SOPs) for practice, as well as concerns for equity and health disparities are presented along with discussion of the limitations of telehealth neurodevelopmental care.
Introduction to Neurodevelopmental Assessment
Neurodevelopmental assessment is considered a standard part of comprehensive care for children with medical conditions and/or treatment that impacts central nervous system functioning. It typically involves an intake interview with the family/patient, testing, feedback about the results, and follow-up. The primary goal of these assessments is to help families, medical teams, and schools better understand a child’s neurocognitive strengths and weaknesses. They also provide ongoing monitoring of a child’s developmental trajectory and tailored recommendations to facilitate access to and inform early intervention, outpatient, and school-based services. CNOC was developed to determine and implement best practices of neurodevelopmental and psychosocial services for individuals with pediatric and congenital heart disease and their families through clinical, quality improvement, and research initiatives (Marino et al., 2021). CNOC has developed specific batteries (Ilardi et al., 2020, Ware et al., 2020) to assess domains of functioning that are particularly impacted in this population (Marino et al., 2012) and recommends assessment of cognitive/intellectual functioning, language, visual-spatial skills, attention, executive function, learning/memory, fine and gross motor skills, academics, and adaptive skills, as well as social/emotional/behavioral functioning.
Model Integrating Telehealth Within Neurodevelopmental Assessment
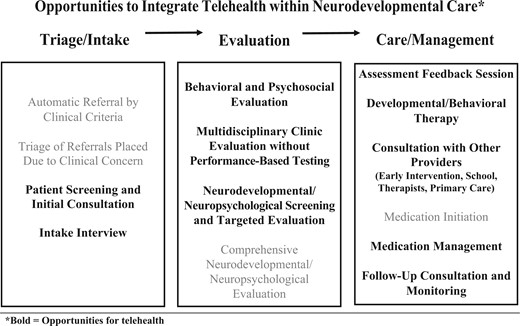
Opportunities for utilizing telehealth exist at all stages of neurodevelopmental care, from intake to follow-up (Figure 1); however, implementation will vary based on the workflow, resources, and organization of each program. Many clinics utilize a risk-based approach (Baum et al., 2017; Hardy et al., 2017), which, as described below, can also be adapted for telehealth. For example, monitoring and screening can be conducted via telehealth to indicate when a more comprehensive, in-person assessment is needed.
Opportunities to integrate telehealth within neurodevelopmental care*.
Referrals for neurodevelopmental assessment are often based on clinical criteria; a telehealth intake interview is ideal to identify primary concerns and determine the extent of testing needed. The intake can also serve as a consultation, providing preliminary recommendations and referrals while patients await a comprehensive assessment. Screening and consultation using telehealth may improve the allocation of limited resources, which may reduce costs and improve efficiency for providers, families, and health systems. It may also reduce delays in accessing interventions.
Based on information gathered during the intake, an assessment can be conducted via telehealth, in person, or with components of both. For patients with prior neurodevelopmental diagnoses, previous assessments, or established intervention services, a targeted telehealth test battery with a comprehensive caregiver/patient interview and record review may be sufficient to update recommendations for clinical management. For patients requiring in-person testing, an initial telehealth screening may inform the testing needed for the in-person session, reducing the length, and resources required for, this visit.
Telehealth lends itself to behavioral/psychosocial assessment using questionnaires, and some performance-based tests have been adapted to telehealth (Harder et al., 2020). Although telehealth does not replace a comprehensive in-person assessment, many neurodevelopmental domains can be assessed. Table I illustrates feasibility, validity, and technology required to administer CNOC’s recommended core clinical battery via telehealth as an exemplar (Ilardi et al., 2020; Ware et al., 2020). Generally, expressive language, verbal reasoning, and verbal memory can be easily measured via telehealth; receptive language and academic screening can be assessed with the use of a third camera (e.g., smart phone or tablet); and visual-motor integration can be measured if materials are mailed beforehand.
Telehealth Feasibility Overview of CNOC Neurodevelopmental Assessment Batteries
| Neurodevelopmental tests . | Recommendation for telehealth administration . |
|---|---|
| Zero-to-five battery | |
| Bayley Scales of Infant and Toddler Development, Fourth Edition (BSID-4) | Not recommended |
| Wechsler Preschool and Primary Scales of Intelligence, Fourth Edition (WPPSI-IV) | Select subtests feasible |
| Bracken Basic Concepts Scales, Third Edition | Feasible with third camera |
| Beery-Buktenica Visual-Motor Integration Test (VMI) | Feasible with mailing materials |
| School-age battery | |
| Wechsler Intelligence Scale for Children, Fifth Edition (WISC-V) | Select subtests feasible |
| Wechsler Adult Intelligence Scale, Fourth Edition (WAIS-IV) | Select subtests feasible |
| Wechsler Abbreviated Scale of Intelligence, Second Edition (WASI-II) | Select subtests feasible |
| Wechsler Individual Achievement Test, Third or Fourth Edition (WIAT-III/IV) | Select subtests feasible |
| Woodcock Johnson Tests of Achievement, Third Edition (WJ-III) | Select subtests feasible |
| Wide Range Assessment of Memory and Learning, Second Edition (WRAML-2) | Select subtests feasible |
| California Verbal Learning Test, Children’s Version or Third Edition (CVLT-C/3) | Feasible |
| Delis-Kaplan Executive Function System (D-KEFS) | Select subtests feasible |
| Beery-Buktenica VMI | Feasible with mailing materials |
| Grooved Pegboard Test | Not recommended |
| Neurodevelopmental tests . | Recommendation for telehealth administration . |
|---|---|
| Zero-to-five battery | |
| Bayley Scales of Infant and Toddler Development, Fourth Edition (BSID-4) | Not recommended |
| Wechsler Preschool and Primary Scales of Intelligence, Fourth Edition (WPPSI-IV) | Select subtests feasible |
| Bracken Basic Concepts Scales, Third Edition | Feasible with third camera |
| Beery-Buktenica Visual-Motor Integration Test (VMI) | Feasible with mailing materials |
| School-age battery | |
| Wechsler Intelligence Scale for Children, Fifth Edition (WISC-V) | Select subtests feasible |
| Wechsler Adult Intelligence Scale, Fourth Edition (WAIS-IV) | Select subtests feasible |
| Wechsler Abbreviated Scale of Intelligence, Second Edition (WASI-II) | Select subtests feasible |
| Wechsler Individual Achievement Test, Third or Fourth Edition (WIAT-III/IV) | Select subtests feasible |
| Woodcock Johnson Tests of Achievement, Third Edition (WJ-III) | Select subtests feasible |
| Wide Range Assessment of Memory and Learning, Second Edition (WRAML-2) | Select subtests feasible |
| California Verbal Learning Test, Children’s Version or Third Edition (CVLT-C/3) | Feasible |
| Delis-Kaplan Executive Function System (D-KEFS) | Select subtests feasible |
| Beery-Buktenica VMI | Feasible with mailing materials |
| Grooved Pegboard Test | Not recommended |
Telehealth Feasibility Overview of CNOC Neurodevelopmental Assessment Batteries
| Neurodevelopmental tests . | Recommendation for telehealth administration . |
|---|---|
| Zero-to-five battery | |
| Bayley Scales of Infant and Toddler Development, Fourth Edition (BSID-4) | Not recommended |
| Wechsler Preschool and Primary Scales of Intelligence, Fourth Edition (WPPSI-IV) | Select subtests feasible |
| Bracken Basic Concepts Scales, Third Edition | Feasible with third camera |
| Beery-Buktenica Visual-Motor Integration Test (VMI) | Feasible with mailing materials |
| School-age battery | |
| Wechsler Intelligence Scale for Children, Fifth Edition (WISC-V) | Select subtests feasible |
| Wechsler Adult Intelligence Scale, Fourth Edition (WAIS-IV) | Select subtests feasible |
| Wechsler Abbreviated Scale of Intelligence, Second Edition (WASI-II) | Select subtests feasible |
| Wechsler Individual Achievement Test, Third or Fourth Edition (WIAT-III/IV) | Select subtests feasible |
| Woodcock Johnson Tests of Achievement, Third Edition (WJ-III) | Select subtests feasible |
| Wide Range Assessment of Memory and Learning, Second Edition (WRAML-2) | Select subtests feasible |
| California Verbal Learning Test, Children’s Version or Third Edition (CVLT-C/3) | Feasible |
| Delis-Kaplan Executive Function System (D-KEFS) | Select subtests feasible |
| Beery-Buktenica VMI | Feasible with mailing materials |
| Grooved Pegboard Test | Not recommended |
| Neurodevelopmental tests . | Recommendation for telehealth administration . |
|---|---|
| Zero-to-five battery | |
| Bayley Scales of Infant and Toddler Development, Fourth Edition (BSID-4) | Not recommended |
| Wechsler Preschool and Primary Scales of Intelligence, Fourth Edition (WPPSI-IV) | Select subtests feasible |
| Bracken Basic Concepts Scales, Third Edition | Feasible with third camera |
| Beery-Buktenica Visual-Motor Integration Test (VMI) | Feasible with mailing materials |
| School-age battery | |
| Wechsler Intelligence Scale for Children, Fifth Edition (WISC-V) | Select subtests feasible |
| Wechsler Adult Intelligence Scale, Fourth Edition (WAIS-IV) | Select subtests feasible |
| Wechsler Abbreviated Scale of Intelligence, Second Edition (WASI-II) | Select subtests feasible |
| Wechsler Individual Achievement Test, Third or Fourth Edition (WIAT-III/IV) | Select subtests feasible |
| Woodcock Johnson Tests of Achievement, Third Edition (WJ-III) | Select subtests feasible |
| Wide Range Assessment of Memory and Learning, Second Edition (WRAML-2) | Select subtests feasible |
| California Verbal Learning Test, Children’s Version or Third Edition (CVLT-C/3) | Feasible |
| Delis-Kaplan Executive Function System (D-KEFS) | Select subtests feasible |
| Beery-Buktenica VMI | Feasible with mailing materials |
| Grooved Pegboard Test | Not recommended |
Following the assessment, telehealth offers a convenient format to present assessment results and recommendations. Further, some neurobehavioral interventions can be implemented with telehealth. A wealth of data demonstrate that telehealth is efficacious for pediatric behavioral intervention (Ros-DeMarize et al., 2021), and many behavioral health and rehabilitation providers now offer telehealth services (Tanner et al., 2020). Telehealth can also be used to communicate with other providers, family members, and school teams. Follow-up monitoring via telehealth between assessment appointments can reduce the burden of care for families. This may, in turn, increase adherence to assessment recommendations and improve overall access to and quality of care.
Telehealth Assessment: Infancy Through Preschool
Standardized assessment of infants and young children via telehealth is challenging, but play-based observations in conjunction with a detailed caregiver interview have utility for screening. Screening should target areas of known risk and can aid in making initial recommendations and inform future/further assessments. Following a caregiver interview, neurodevelopmental screening can be completed by adapting standardized measures into a structured play-based observation of the child’s cognitive, language, and motor skills (Table I). During assessment, the examiner can guide a caregiver in administering tasks, often using materials in the child’s environment (e.g., pointing to pictures in books, stacking blocks, drawing/copying shapes). Assessing a young child in their home environment via telehealth may present a more accurate depiction of their typical functioning through observed spontaneous behaviors and skills (e.g., behavioral outbursts, eating, and speech). To maximize the success of the telehealth session, families should be prepared beforehand, ideally in writing (Figure S1), and the duration of observation should be kept brief, with breaks. Preparation recommendations may include availability of certain toys, and the use of a handheld device with camera that can easily follow the child.
Telehealth Assessment: School-Age Through Adolescence
Many components of school-age neurodevelopmental assessments can be completed using telehealth (Table I). Certain measures lend themselves easily to telehealth administration (e.g., verbal tasks on Wechsler Intelligence Scale for Children, Fifth Edition [WISC-V] (Wechsler, 2014)), while innovative methods are needed to facilitate telehealth assessment of other domains, such as visual-motor integration and visual-spatial skills. For example, assessors can mail a visual-motor integration test booklet in a sealed envelope beforehand and have the caregiver administer on camera. Alternate measures such as the Block Design multiple-choice task from the WISC-V Integrated can be used to compute a Visual Spatial Index. Unfortunately, performance-based measures of attention, executive functioning, and processing speed (e.g., computerized tests of sustained attention) generally cannot be administered via telehealth due to validity threats associated with patient-specific factors and technological limitations.
Some children or referral questions are not well suited for a telehealth assessment session, including concerns about significant developmental delays, language limitations, sensory or motor impairments, or behavioral/attention challenges. Even when completing all testing in person is necessary, the opportunity to obtain a comprehensive history and understanding of presenting concerns, gather behavioral observations, and provide feedback using telehealth remains valuable.
Practice and Clinical Considerations
While guidelines and procedures are well-established for in-person neurodevelopmental assessments, standard practice recommendations for telehealth assessment are limited, especially for pediatric populations (Bilder et al., 2020). Therefore, each practice should establish SOPs for telehealth neurodevelopmental assessment to maintain high standards of care. Practice-specific considerations include number of clinicians, administrative and technological resources, patient volume, and patient population (ages, developmental levels, medical diagnoses, cultures, languages, and socioeconomic factors). SOPs can be especially helpful during triage and intake (Figure 1), guiding decisions about the type of testing needed, including appropriateness of telehealth assessment.
While these individual clinic characteristics will influence implementation, there are some general recommendations for clinicians considering integrating telehealth into their neurodevelopmental practice. A recommended first step is to start by utilizing telehealth for intake and/or feedback appointments so that practitioners become familiar with using telehealth and identify any barriers for their practice or their patients (e.g., access to telehealth interpreters, internet connection, video/audio quality, or connecting to the telehealth platform). The next step could entail progressing to a hybrid model, whereby some components of the assessment are conducted via telehealth and others completed in person. As discussed above, specific domains can be easily assessed via telehealth with minimal changes to standardization (e.g., vocabulary, verbal reasoning, and verbal memory). Additionally, some test publishers have released guidelines for how to modify standardization for telehealth administration which can help clinicians select which measures to administer remotely based on their patient population (MHS, 2020; PAR, 2020; Pearson, 2020).
Clinical tools needed to successfully implement telehealth services include consent forms, templates, and protocols related to providing and billing for neurodevelopmental care via telehealth. Additionally, as the field continues to develop and refine best practices, ongoing education and training should be incorporated into SOPs. Especially for practices with a large number of clinicians, trainees, and/or psychometrists, technical training and continuously monitoring fidelity of telehealth test administration will be needed to ensure provider consistency. Routine quality assurance will be particularly critical if data are used to develop population-based estimates.
Telehealth Application to a Clinical Data Registry
Neurodevelopmental assessment via telehealth can be leveraged for clinical registries. A frequent criticism of pediatric research is that samples lack diversity and may not be representative of broader and vulnerable populations(Mendoza et al., 2019). Telehealth might allow research groups to engage more culturally and geographically diverse populations by expanding access to participation (Shore et al., 2007). As with clinical assessments, telehealth data collection will not entirely replace in-person collection. Instead, it could provide supplemental data to support generalizability or highlight key similarities and differences between samples.
As one example, CNOC launched its clinical registry shortly before the COVID-19 pandemic. Although a comprehensive in-person assessment was preferred, telehealth provided a means to at least partially overcome the barriers to data collection posed by COVID-19. Data collection remains ongoing, and CNOC adapted its registry to track whether assessment was in person or via telehealth. Large clinical registries could be leveraged, independently or collaboratively, to investigate whether telehealth improves access to care for pediatric medical populations. This presents a unique opportunity to systematically study the comparability of telehealth and in-person assessment.
Discussion
Neurodevelopmental assessment is an integral component of comprehensive care to identify a child’s strengths and limitations and provide recommendations to inform treatment. Individual assessment is especially important for children with complex medical conditions who are at increased risk for neurodevelopmental difficulties. There is often a long waitlist for these assessments, and caregivers may experience barriers to attending lengthy in-person appointments. Telehealth offers an avenue to streamline triage, intake, and assessment processes and thereby connect more patients with needed services and supports, more quickly.
Telehealth assessment can improve access to neurodevelopmental care for patients and families who do not have reliable transportation, are not able to take time off work, are unable to find childcare for siblings, are immune-compromised, or live a far distance from the clinic. Telehealth eliminates many of the inconveniences required to attend an in-person appointment (e.g., driving, travel costs), allowing families to access care promptly from home. Additional benefits include increased flexibility in scheduling for families and clinicians, and the option to easily involve caregivers from multiple households. Indeed, our patient/family task force members shared that telehealth is frequently their preferred choice for many types of healthcare appointments. Given that 93% of American adults routinely access the internet (“Internet/Broadband Fact Sheet,” 2021), telehealth services are likely to be accessible to most families. To further reduce barriers to accessing telehealth care, it has been recommended to utilize technology that the patient/family already owns and is familiar with, such as a smart phone (Anaya et al., 2021).
Despite multiple advantages, there are several limitations to telehealth assessment. Although telehealth is potentially a tool to address health disparities related to access to care or research, there is minimal information on cultural considerations in the use of telehealth. For instance, telehealth may amplify certain aspects of the environment that can be uncomfortable for those with non-Western values (e.g., prolonged eye contact, punctuality, variations in communication norms) (Yellowlees et al., 2008). Additionally, there is a higher probability for boundary violations during telehealth sessions located in the family’s home and at times, in the practitioner’s home. For clinics, increased access to care via telehealth may require more resources to serve a larger patient population. In a recent review, cost, insurance reimbursement, and technical issues were cited as the top barriers for healthcare centers to adopt telehealth (Lin et al., 2018). The long-term viability of telehealth for neurodevelopmental assessment is also dependent upon legislators and insurance companies establishing plans for appropriate reimbursement beyond the COVID-19 pandemic.
Finally, there are important challenges related to keeping the testing environment controlled. The clinician and family may have less control of distractions (particularly in multi-generational homes), and greater difficulty ensuring confidentiality. Furthermore, there is little research available on disparities in access to the technology and electronic devices needed for telehealth assessment. Racial minorities and low-income families are less likely to have broadband internet and computer access at home (Katzow et al., 2020). Therefore, those who experience challenges accessing in-person care may also be those who have the greatest difficulty accessing telehealth. Providers may address this divide by partnering with community clinics, schools, and public libraries (Wicklund, 2021) to provide local settings for patients to complete telehealth assessments. A community-based approach may also improve continuity of care and communication across settings, such as between psychologists, schools, and community mental health providers.
Future Directions
In the wake of the COVID-19 pandemic, clinicians rapidly transitioned to telehealth neurodevelopmental assessment services, pushing the field beyond traditional in-person assessment models. There was a clear, immediate benefit to providing crucial services to patients in the context of infection-control restrictions and social distancing. While many practices have returned to traditional, face-to-face neurodevelopmental assessment services, telehealth will continue to provide opportunities to broaden service delivery and access to care. Further work is needed to establish how standardized testing conducted via telehealth compares to in-person testing. Additionally, further investigation is needed to determine whether a telehealth or hybrid service model improves or exacerbates existing healthcare disparities for low-resource populations. Clinicians, researchers, institutions, and policymakers have the unique opportunity to harness the momentum initiated by necessity during the pandemic to meaningfully expand the accessibility, adaptability, and continuity of neurodevelopmental care for children.
Supplementary Data
Supplementary data can be found at: https://academic.oup.com/jpepsy.
Conflicts of Interest
None declared.
References
Internet/Broadband Fact Sheet. (
MHS. (2020). Remote administration. https://mhs.com/info/remote-admin-collection/
Pearson. (2020). Staying connected through telepractice. https://www.pearsonassessments.com/professional-assessments/digital-solutions/telepractice/resources.html