-
PDF
- Split View
-
Views
-
Cite
Cite
Marie-Louise Sharp, Nicola T. Fear, Roberto J. Rona, Simon Wessely, Neil Greenberg, Norman Jones, Laura Goodwin, Stigma as a Barrier to Seeking Health Care Among Military Personnel With Mental Health Problems, Epidemiologic Reviews, Volume 37, Issue 1, 2015, Pages 144–162, https://doi.org/10.1093/epirev/mxu012
Close - Share Icon Share
Abstract
Approximately 60% of military personnel who experience mental health problems do not seek help, yet many of them could benefit from professional treatment. Across military studies, one of the most frequently reported barriers to help-seeking for mental health problems is concerns about stigma. It is, however, less clear how stigma influences mental health service utilization. This review will synthesize existing research on stigma, focusing on those in the military with mental health problems. We conducted a systematic review and meta-analysis of studies between 2001 and 2014 to examine the prevalence of stigma for seeking help for a mental health problem and its association with help-seeking intentions/mental health service utilization. Twenty papers met the search criteria. Weighted prevalence estimates for the 2 most endorsed stigma concerns were 44.2% (95% confidence interval: 37.1, 51.4) for “My unit leadership might treat me differently” and 42.9% (95% confidence interval: 36.8, 49.0) for “I would be seen as weak.” Nine studies found no association between anticipated stigma and help-seeking intentions/mental health service use and 4 studies found a positive association. One study found a negative association between self-stigma and intentions to seek help. Counterintuitively, those that endorsed high anticipated stigma still utilized mental health services or were interested in seeking help. We propose that these findings may be related to intention-behavior gaps or methodological issues in the measurement of stigma. Positive associations may be influenced by modified labeling theory. Additionally, other factors such as self-stigma and negative attitudes toward mental health care may be worth further attention in future investigation.
INTRODUCTION
The mental health needs of serving and veteran/former service personnel have been the focus of current research since the recent military deployments of troops to Iraq and Afghanistan (1–4). Numerous studies have shown that the prevalence of any mental health disorders, including post-traumatic stress disorder (PTSD) and alcohol disorders in United Kingdom, United States, and Canadian military personnel, is approximately 37%, 43%, and 15%, respectively (2, 5–9). Across all nations, a large proportion of military personnel who experience mental health problems do not seek help (1, 9–13). Typically 40%–60% of those who could benefit from professional treatment do not access help or services (1, 14, 15). Of those that do access help in the United Kingdom, most help sought is from nonmedical/informal sources (13, 16). There are also concerns, especially in the United States, that up to 60%–70% of veterans with a mental health diagnosis do not receive adequate treatment (8 or more sessions) within a year of their diagnosis (17, 18). As a result of these findings, there has been much research examining barriers that impede help-seeking behavior and engagement with treatment, which has aimed to understand the substantial unmet need of mental health care in military populations.
Contemporary studies have identified many different barriers to help-seeking in military populations, including stigma (14, 19–21), practical/logistic barriers to care (14, 22), negative attitudes related to mental health treatment (23, 24), and poor recognition of the need for treatment (21, 25). However, a large proportion of this research has primarily examined the impact of stigma on help-seeking behaviors and the role that it plays in decisions to seek help (10, 14, 18–21, 23, 24, 26–32).
Stigma is a complex and contested construct with many theoretical facets. Although there are competing definitions, we describe some of the most relevant and most often used terms below. Stigma is often conceptualized as a belief relating to an “attribute that is deeply discrediting,” that reduces the target, whether it be the self or other, “from a whole and usual person to a tainted, discounted one” (33, p. 265). Theoretically stigma can occur at individual, interpersonal (interactions among dyads or groups), and sociocultural levels (across societies or cultures) (34). Stigma that occurs at the sociocultural and interpersonal levels has often been termed public stigma or enacted stigma. The process of stigmatization follows when groups with power stereotype hold prejudice and discriminate against a group that has been labeled as separate or different (35–37). This stigmatization is related to shared cultural beliefs held by the general public or, in this case, the military organization about the attributes of those with mental illness that can lead to explicit acts of discrimination and hostility resulting in enacted stigma (38). At the individual level, a facet of stigma has been described as felt normative stigma, which is the individual's belief about the prevalence of stigmatizing views among people in their community (38). Additionally, anticipated stigma has been termed the extent to which people believe they personally will be viewed or treated in a stigmatizing way if their mental health problem or related help-seeking becomes known (39, 40). Internalized stigma for an individual, not in a stigmatized group, results in prejudice toward the stigmatized or stigma endorsement (38, 41). However, self-stigma reflects a stigmatized individual's internalization of actual or perceived negative societal beliefs toward those who have mental health problems. Self-stigmatization can lead to feelings of shame and inadequacy, which may affect an individual's self-worth and confidence to seek help (42, 43). Stigma types at all of these levels interact with each other and can act as barriers to help-seeking (34, 44).
Military organizations may engender certain stigmatizing beliefs in relation to help-seeking for mental health problems that may also persist into civilian life (27, 45, 46). These beliefs may be related to military culture, rules, and conduct learned and experienced in service. For example, the value placed on the actions of the group to achieve military objectives above all else, the cultures of reliance upon each other, masculinity, self-sufficiency, and the stigmas of going sick or shirking work have been noted to affect help-seeking behaviors (11, 20, 47). The requirement for operational readiness through good health conflicts with the direct availability of mental health care provided by the military for service personnel. In this sense, personnel are faced with a choice between disclosure of health problems in order to access care and the potential negative effect upon their operational effectiveness and, thus, their careers. Hence, military objectives, health care, structures, and cultures may interact to create barriers to seeking help for mental health problems, and personnel may therefore elect not to disclose mental health problems (27, 48).
Across the literature when considering mental health help-seeking from formal/professional or medical sources, stigmatizing beliefs are reported at consistently greater levels than practical or logistical barriers to care, irrespective of whether personnel are full-time regular military, reserves, or veterans/former service members (1, 14, 19, 39, 49). Research has also consistently found that personnel reporting more mental health symptoms perceive greater levels of stigma and barriers to care than those with subthreshold symptoms (1, 14, 23, 49–52).
The aims of this review were to address the following: This review is important as there is a need to systematically assess and collate the available evidence about stigma and its relationship with medical/formal help-seeking and mental health service use in military populations with mental health problems. We are not aware of any review that has previously brought this literature together. There is a need to review the methods, methodologies, and research designs used in the military studies in this research area to allow an assessment of the robustness and quality of results in this field of research.
What types of stigma have been explored in military studies that examine medical/formal help-seeking behaviors for those with mental health problems?
What is the prevalence of stigma measured in military populations of those experiencing mental health problems?
What is the direction and strength of association between stigma and medical/formal help-seeking intentions and mental health service use among those with mental health problems?
This review focuses on those in military populations who have probable mental health problems as they are the group most in need of mental health care. Their help-seeking behaviors are important to understand in terms of their need to access mental health care and the associated evidence that they experience a higher stigma prevalence compared with healthy military populations (1, 14, 23, 49–52). Questions regarding (hypothetical) help-seeking will also be more salient for individuals with a mental health problem than for those without. This review focuses upon medical or formal help-seeking rather than support from family and friends or welfare officers/chaplains/charities with no associated medical/formal input. This is to assess access to medical/formal services for those who are unwell who could most benefit from that access. Additionally, this review focuses on recent military populations, primarily those who have been active during the Afghanistan and Iraq conflicts, from 2001 onward. By conflating international stigma data from these groups who may be negotiating present-day health-care systems, we believe that it may be possible to assess the most relevant contemporary military mental health-care barriers.
METHODS
Search strategy
The literature search was conducted in February 2014. Relevant studies published since 2001 in peer-reviewed journals were identified through electronic searches on MEDLINE, PsycINFO, Embase, Web of Science, and Scopus databases.
Key search terms were combined with Boolean operators. These included the following: Duplicate papers were removed, and the reference lists of all eligible studies were checked for additional studies. Dissertation abstracts were reviewed to check whether the authors' work had been published in peer-reviewed journals. Authors were also asked to view the reference list and indicate any other possible missing studies.
“mental health” OR “mental illness” OR “mental disorder” OR “psychological distress” OR “common mental health disorders” OR “anxiety” OR “stress disorders” OR “acute stress” OR “posttraumatic stress disorder” OR “PTSD” OR “depression” OR “alcohol” OR “substance misuse” OR “substance abuse,” combined with
“help-seeking” OR “help-seeking behaviour” OR “help-seeking attitudes” OR “help-seeking intentions” OR “barriers to healthcare” OR “healthcare seeking” OR “treatment seeking” OR “healthcare utilisation” OR “healthcare utilization” OR “service utilisation” OR “service utilization,” combined with
“stigma” OR “self-stigma,” combined with
“military personnel” OR “military” OR “service personnel” OR “armed forces” OR “armed services” OR “veterans” OR “ex-service personnel” OR “reserves” OR “national guard” OR “navy” OR “marines” OR “air force” OR “soldiers,” using the AND operator.
After full-text articles were accessed to assess eligibility, authors of any studies that were deemed eligible but did not report the relevant data were followed up. Additional data were received from Iversen et al. (14), Jones et al. (53), Kehle et al. (15), Osório et al. (49), and Pietrzak et al. (32).
Inclusion criteria
Studies using quantitative methodologies.
All studies published in peer-reviewed journals.
Populations including international military populations (regular military, reserves (or international equivalents), National Guard, and veteran/former service personnel).
Recent military populations studied since 2001.
Studies that measured mental health; this included common mental health disorders (depression and anxiety disorders), PTSD, and alcohol problems (hazardous drinking, misuse, abuse, dependence).
Studies that measured the association between stigma and medical/formal help-seeking for those in the military experiencing mental health problems. This included attitudes/intentions to seek medical/formal help and actual mental health service use. Medical/formal help-seeking was defined as medical/formal help-seeking for mental health problems resulting in service use (in-service and ex-service mental health services) such as primary care, secondary mental health services, psychotherapy, psychologist, psychiatrist, and counseling.
Studies that used stigma as measured on a scale or subscale utilizing established and/or validated measures of stigma.
Exclusion criteria
Papers were excluded that
Addressed stigma as a help-seeking barrier in other populations such as the general population, nonmilitary occupational studies, military contractors, military spouses, prisoners, and homeless individuals.
Measured help-seeking intentions or service use but did not measure stigma.
Measured stigma and help-seeking intentions but did not stratify their sample by mental health status or control for mental health status in statistical models (unless data could be obtained from authors).
Where prevalence of stigma OR association of stigma and help-seeking intentions/service use was not reported and data could not be obtained from the authors.
Data extraction and analysis
Data extraction was conducted by one researcher (M. L. S.). Data from 20 papers were extracted, which included information on author, title and date of publication, overall sample size, sample size of those with mental health problems, country the study originated from, study design, sample selection criteria, and service status (i.e., regular military, reserves, National Guard, veteran/former service personnel), when data were gathered in relation to deployment, empirical measurement of stigma including associated stem questions and Likert scale treatment, internal reliability of stigma scale used (Cronbach's α scores), and key variables measured (Web Table 1 available at http://aje.oxfordjournals.org/).
Data were also extracted including information on the prevalence of stigma items of those with mental health problems (Web Table 2). The numerator (the number of individuals endorsing stigma items) and the denominator (the sample size or number of participants who had mental health problems and responded to the item) were entered into the review database. Studies did not, however, consistently report numerators, denominators, or prevalence; hence, these data were calculated from available data in the paper, or additional data were obtained from the authors.
Prevalence expressed as the percentage of endorsed stigma items, standard errors, and 95% confidence intervals were calculated for meta-analyses to produce weighted averages for the 6 most common stigma items measured in samples across the 20 studies. Stata statistical software, Release 11 (StataCorp LP, College Station, Texas), was used for the meta-analyses.
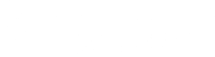
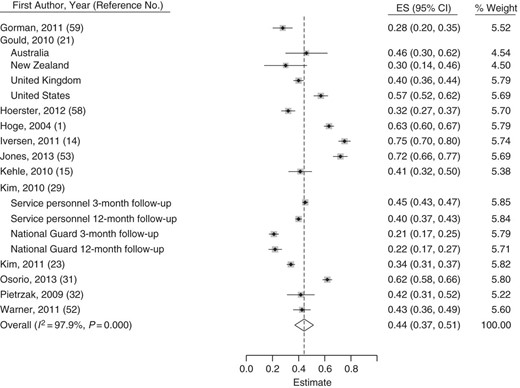
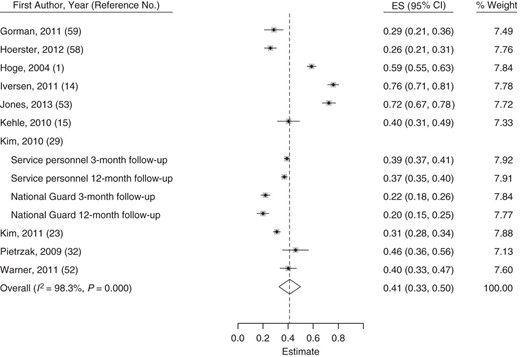
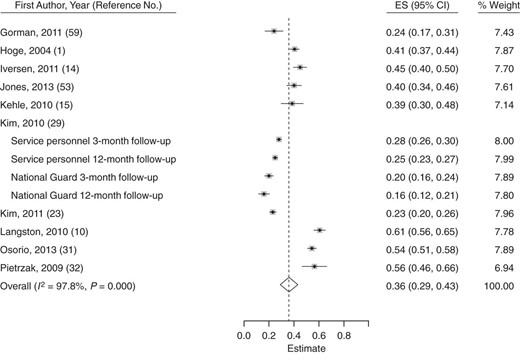
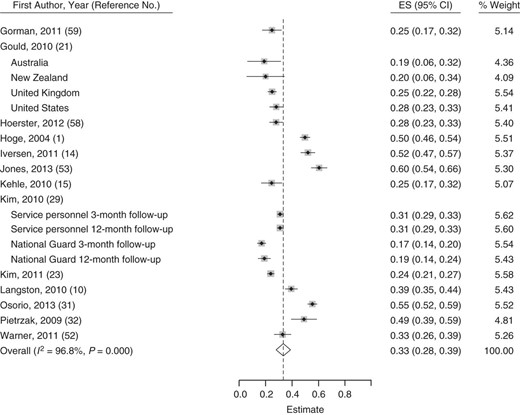
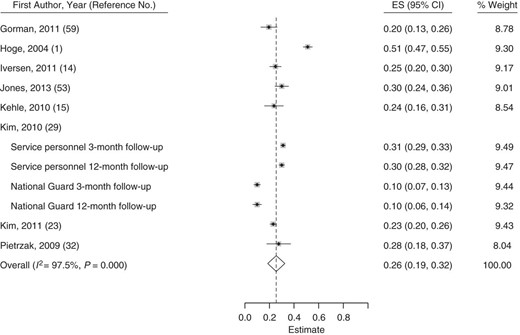
The metan command was used to produce forest plots (Figures 1–6), displaying the prevalence of endorsed stigma items, 95% confidence intervals, and weights for each sample, as well as the overall weighted average and 95% confidence interval.
Fixed-effects models were initially run for each stigma item; however, random-effects models were then fitted to account for high heterogeneity among study samples after assessment of I2, which is an estimate of the variability in results across studies that can be attributed to heterogeneity as opposed to chance (54). Heterogeneity measured through I2 ranges from 0% to 100% and benchmarks high heterogeneity at greater than 50%.
Meta-analyses for each stigma item were stratified by the country (United States and United Kingdom) to assess sources of heterogeneity further.
Forest plot displaying the prevalence for each study and an overall weighted prevalence for the stigma item from the Perceived Stigma and Barriers to Care for Psychological Problems-Stigma Subscale (PSBCPP-SS), “My unit leadership might treat me differently,” across studies from 2004 to 2014. Weights are from random-effects analysis. CI, confidence interval; ES, estimate.
Forest plot displaying the prevalence for each study and an overall weighted prevalence for the stigma item from the Perceived Stigma and Barriers to Care for Psychological Problems-Stigma Subscale (PSBCPP-SS), “I would be seen as weak,” across studies from 2004 to 2014. Weights are from random-effects analysis. CI, confidence interval; ES, estimate.
Forest plot displaying the prevalence for each study and an overall weighted prevalence for the stigma item from the Perceived Stigma and Barriers to Care for Psychological Problems-Stigma Subscale (PSBCPP-SS), “Members of my unit might have less confidence in me,” across studies from 2004 to 2014. Weights are from random-effects analysis. CI, confidence interval; ES, estimate.
Forest plot displaying the prevalence for each study and an overall weighted prevalence for the stigma item from the Perceived Stigma and Barriers to Care for Psychological Problems-Stigma Subscale (PSBCPP-SS), “It would be too embarrassing,” across studies from 2004 to 2014. Weights are from random-effects analysis. CI, confidence interval; ES, estimate.
Forest plot displaying the prevalence for each study and an overall weighted prevalence for the stigma item from the Perceived Stigma and Barriers to Care for Psychological Problems-Stigma Subscale (PSBCPP-SS), “It would harm my career,” across studies from 2004 to 2014. Weights are from random-effects analysis. CI, confidence interval; ES, estimate.
Forest plot displaying the prevalence for each study and an overall weighted prevalence for the stigma item from the Perceived Stigma and Barriers to Care for Psychological Problems-Stigma Subscale (PSBCPP-SS), “My leaders would blame me for the problem,” across studies from 2004 to 2014. Weights are from random-effects analysis. CI, confidence interval; ES, estimate.
Additional data were also extracted from papers on measures of association between stigma scores and help-seeking intentions/mental health service utilization including other key findings of note (Tables 1 and 2).
Association Between Stigma and Health Service Use From Studies Published in 2004–2014
| First Author, Year (Reference No.) . | Study Location . | Population Type . | Study Type . | Study Size . | Association Between Stigma and Mental Health Service Use . | Other Relevant Findings . |
|---|---|---|---|---|---|---|
| Harpaz-Rotem, 2014 (57) | United States | Veterans | Prospective | 137 | No significant difference in anticipated stigma between those that did not receive mental health treatment (mean = 3.18, SD, 0.87) and those that did receive mental health treatment (mean = 2.94, SD, 1.04; t = 1.224; P = 0.223; df = 134). | Veterans in this study who endorsed greater stigma were not deterred from utilizing mental health services. Multivariate logistic regression revealed that only greater unit support (OR = 1.06, 95% CI: 1.02, 1.10; P = 0.006) and severity of PTSD symptoms (OR = 1.05, 95% CI: 1.02, 1.09; P = 0.002) were associated with initiation of use of mental health services. Study investigates specific symptom clusters and effect on treatment-seeking. Post hoc analysis—PTSD reexperiencing symptoms associated with increased odds of initiating treatment (OR = 1.13, 95% CI: 1.05, 1.23; P = 0.02), numbing symptoms associated with increased odds of retention in treatment (12 or more mental health visits) (OR = 1.15, 95% CI: 1.06, 1.24; P = 0.001). Likelihood of retention in treatment positively associated with greater severity of PTSD symptoms (OR = 1.09, 95% CI: 1.04, 1.15; P > 0.001). |
| Kehle, 2010 (15) | United States | National Guard | Cross-sectional | 424 overall; 117 with mental health problems | Stigma did not significantly predict mental health service utilization when using number of positive stigma items as the predictor (AOR = 1.017, 95% CI: 0.921, 1.122; P > 0.05) or stigma as measured in a high/low median split (AOR = 1.24, 95% CI: 0.745, 2.065; P > 0.05) (model adjusted for mental health status). | Models unadjusted for mental health status found positive attitudes toward mental health treatment (AOR = 1.40, 95% CI: 1.10, 1.79; P < 0.05), receiving therapy in theater (AOR = 2.21, 95% CI: 1.12, 4.33; P < 0.05), severity of illness (need factor score) (AOR = 1.52, 95% CI: 1.18, 1.96; P < 0.01), and in-theater injuries (AOR = 1.98, 95% CI: 1.13, 3.47; P < 0.05) all positively associated with mental health service use. |
| Rosen, 2011 (18) | United States | Veterans | Cross-sectional | 482 | No association of stigma with retrospective reports of initiating therapy (AOR = 1.12, 95% CI: 0.82, 1.52; P > 0.05) or prospectively (after survey time 1) (AOR = 1.07, 95% CI: 0.73, 1.57; P > 0.05). Positive association of stigma and completing 8 or more PTSD psychotherapy visits (AOR = 1.51, 95% CI: 1.00, 2.28; P < 0.05). Positive association between reporting stigma and retrospective reports of use of Veteran Centre counseling services (AOR = 1.69, 95% CI: 1.24, 2.30; P < 0.01). | One in 3 veterans endorsed moderate/high stigma concerns as barriers to care; however, stigma was not retrospectively or prospectively associated with initiating psychotherapy. Those that reported higher levels of stigma concerns were more likely to complete treatment and have used Veteran Centre counseling. Retrospective initiation (prior to survey) and prospective use of PTSD psychotherapy services were positively associated with severity of mental health problem/impairment (AOR = 1.44, 95% CI: 1.01, 1.89; P < 0.01; and AOR = 1.73, 95% CI: 1.21, 2.47; P < 0.01). Retrospective initiation (prior to survey) of PTSD psychotherapy was positively associated with an individual's being diagnosed in a veteran association mental health-care setting rather than a medical setting (AOR = 2.68, 95% CI: 1.65, 4.35; P < 0.01). Prospective initiation of PTSD psychotherapy was associated with being part of a male Iraq/Afghan group (reference, male Vietnam era group) (AOR = 2.95, 95% CI: 1.37, 6.36; P < 0.01). Patients with greater impairment or desire for help did not receive more sessions of psychotherapy. Hence, the amount of care used was not determined by need or desire for help. |
| Pietrzak, 2009 (32) | United States | Veterans | Cross-sectional | 272 overall; 102 with mental health problems | Stigma was not associated with counseling visits (AOR = 0.92, 95% CI: 0.53, 1.59; P = 0.76). Stigma was not associated with medication use (AOR = 1.11, 95% CI: 0.54, 2.27; P = 0.78). | Group who screened positive for a mental health problem scored higher on the stigma scale compared with those without a diagnosis (score = 2.89, SD, 1.0 vs. score = 2.31, SD, 0.9; F = 17.7; df = 1 and 247; P < 0.001; Cohen's d = 0.54) and were more likely to endorse nearly all of the stigma items (ORs = 2.10–4.15). PTSD was positively associated with counseling and medication visits (AOR = 10.69, 95% CI: 2.97, 38.39; P < 0.05). Negative beliefs about mental health care were negatively associated with counseling and medication visits (AOR = 0.83, 95% CI: 0.72, 0.95; P < 0.05; and AOR = 0.69, 95% CI: 0.56, 0.85; P < 0.05). |
| Kim, 2011 (23) | United States | In-service personnel (regular military) | Cross-sectional | 2,623 overall; 881 with mental health problems | Stigma not associated with treatment utilization for any type of care. Association of anticipated stigma with any type of care/treatment (AOR = 1.09, 95% CI: 0.84, 1.41; P = 0.502). Mental health professional—military (AOR = 1.16, 95% CI: 0.87, 1.54; P = 0.308). Mental health professional—civilian (AOR = 0.93, 95% CI: 0.58, 1.49; P = 0.772). | Top 3 concerns about barriers to care for those with and without mental health problems were all stigma related; however, this did not predict service use. Negative attitudes toward treatment predicted decreased treatment utilization from: Any type of care/treatment (AOR = 0.63, 95% CI: 0.45, 0.87; P = 0.005). Mental health professional—military (AOR = 0.58, 95% CI: 0.41, 0.84; P = 0.004) (nonsignificant result for mental health professional—civilian (AOR = 0.70, 95% CI: 0.39, 1.24; P = 0.219)). |
| Hoerster, 2012 (58) | United States | Veterans | Prospective | 305 | Stigma was not associated with receipt of adequate mental health treatment (9 or more mental health visits) (odds ratios not reported). Receipt of treatment as a continuous variable was not associated with stigma (odds ratios not reported). | Stigma barriers were most commonly endorsed (111 veterans, 37% endorsed at least 1 stigma-related barrier). Those with greater symptom severity and females were more likely to receive adequate treatment after adjustment for either PTSD symptom severity or depression symptom severity and sex, military branch, endorsement of stigma- related barriers, and endorsement of trust-related barriers. PTSD symptom severity (AOR = 1.03, 95% CI: 1.01, 1.05; P = 0.003) and being female (AOR = 4.82, 95% CI: 1.37, 16.99; P = 0.014) were associated with receiving adequate treatment. Depression symptom severity (AOR = 1.06, 95% CI: 1.01, 1.11; P = 0.01) and being female (AOR = 3.98, 95% CI: 1.17, 13.49; P = 0.027) were associated with receiving adequate treatment. |
| Jones, 2013 (53) | United Kingdom | Regular military/reserves | Cross-sectional | 484 overall; 262 with mental health problems | Stigma was not associated with utilization of mental health services for those with mental health problems after adjustment for rank, age, service length, sex, relationship status, and deployment in the last year (AOR = 2.27, 95% CI: 0.57, 3.82; P > 0.05). | Those with common mental health disorders or PTSD symptoms had increased odds of endorsing stigma (AOR = 3.07, 95% CI: 1.95, 4.84; P < 0.05) but not among those drinking alcohol at potentially harmful levels (AOR = 1.08, 95% CI: 0.68, 1.70; P > 0.05). A statistically significant trend was observed for increasing levels of stigma reported from the lowest levels among non–help-seekers who screened negative for mental health problems, through moderate levels among negative screening help-seekers and positive screening help-seekers, to the highest levels among positive screening non–help-seekers (χ2 test for trend = 25.23, P ≤ 0.0001). Over 90% of those that screened positive for a mental health problem endorsed that “Mental health support can be useful for those who need it.” Eighty percent of those that screened positive for a mental health problem endorsed that “It takes courage or strength to get treatment for a psychological problem.” Those that expressed potentially discriminatory views about other people with mental health problems were also more likely to report higher levels of stigma (AOR = 2.66, 95% CI: 1.47, 4.82; P < 0.05). |
| Elnitsky, 2013 (63) | United States | Regular military (Army combat medics) | Cross-sectional | 799 overall; 54 with mental health problems | Positive association of anticipated stigma and utilization of mental health services by combat medics (AOR = 1.61, 95% CI: not reported; P = 0.01). Positive association of anticipated stigma and mental health service utilization by males (AOR = 1.58, 95% CI: 1.09, 2.30). | A nonsignificant association was observed between stigma and mental health service use by female combat medics (AOR = 1.46, 95% CI: 0.78, 2.76). |
| First Author, Year (Reference No.) . | Study Location . | Population Type . | Study Type . | Study Size . | Association Between Stigma and Mental Health Service Use . | Other Relevant Findings . |
|---|---|---|---|---|---|---|
| Harpaz-Rotem, 2014 (57) | United States | Veterans | Prospective | 137 | No significant difference in anticipated stigma between those that did not receive mental health treatment (mean = 3.18, SD, 0.87) and those that did receive mental health treatment (mean = 2.94, SD, 1.04; t = 1.224; P = 0.223; df = 134). | Veterans in this study who endorsed greater stigma were not deterred from utilizing mental health services. Multivariate logistic regression revealed that only greater unit support (OR = 1.06, 95% CI: 1.02, 1.10; P = 0.006) and severity of PTSD symptoms (OR = 1.05, 95% CI: 1.02, 1.09; P = 0.002) were associated with initiation of use of mental health services. Study investigates specific symptom clusters and effect on treatment-seeking. Post hoc analysis—PTSD reexperiencing symptoms associated with increased odds of initiating treatment (OR = 1.13, 95% CI: 1.05, 1.23; P = 0.02), numbing symptoms associated with increased odds of retention in treatment (12 or more mental health visits) (OR = 1.15, 95% CI: 1.06, 1.24; P = 0.001). Likelihood of retention in treatment positively associated with greater severity of PTSD symptoms (OR = 1.09, 95% CI: 1.04, 1.15; P > 0.001). |
| Kehle, 2010 (15) | United States | National Guard | Cross-sectional | 424 overall; 117 with mental health problems | Stigma did not significantly predict mental health service utilization when using number of positive stigma items as the predictor (AOR = 1.017, 95% CI: 0.921, 1.122; P > 0.05) or stigma as measured in a high/low median split (AOR = 1.24, 95% CI: 0.745, 2.065; P > 0.05) (model adjusted for mental health status). | Models unadjusted for mental health status found positive attitudes toward mental health treatment (AOR = 1.40, 95% CI: 1.10, 1.79; P < 0.05), receiving therapy in theater (AOR = 2.21, 95% CI: 1.12, 4.33; P < 0.05), severity of illness (need factor score) (AOR = 1.52, 95% CI: 1.18, 1.96; P < 0.01), and in-theater injuries (AOR = 1.98, 95% CI: 1.13, 3.47; P < 0.05) all positively associated with mental health service use. |
| Rosen, 2011 (18) | United States | Veterans | Cross-sectional | 482 | No association of stigma with retrospective reports of initiating therapy (AOR = 1.12, 95% CI: 0.82, 1.52; P > 0.05) or prospectively (after survey time 1) (AOR = 1.07, 95% CI: 0.73, 1.57; P > 0.05). Positive association of stigma and completing 8 or more PTSD psychotherapy visits (AOR = 1.51, 95% CI: 1.00, 2.28; P < 0.05). Positive association between reporting stigma and retrospective reports of use of Veteran Centre counseling services (AOR = 1.69, 95% CI: 1.24, 2.30; P < 0.01). | One in 3 veterans endorsed moderate/high stigma concerns as barriers to care; however, stigma was not retrospectively or prospectively associated with initiating psychotherapy. Those that reported higher levels of stigma concerns were more likely to complete treatment and have used Veteran Centre counseling. Retrospective initiation (prior to survey) and prospective use of PTSD psychotherapy services were positively associated with severity of mental health problem/impairment (AOR = 1.44, 95% CI: 1.01, 1.89; P < 0.01; and AOR = 1.73, 95% CI: 1.21, 2.47; P < 0.01). Retrospective initiation (prior to survey) of PTSD psychotherapy was positively associated with an individual's being diagnosed in a veteran association mental health-care setting rather than a medical setting (AOR = 2.68, 95% CI: 1.65, 4.35; P < 0.01). Prospective initiation of PTSD psychotherapy was associated with being part of a male Iraq/Afghan group (reference, male Vietnam era group) (AOR = 2.95, 95% CI: 1.37, 6.36; P < 0.01). Patients with greater impairment or desire for help did not receive more sessions of psychotherapy. Hence, the amount of care used was not determined by need or desire for help. |
| Pietrzak, 2009 (32) | United States | Veterans | Cross-sectional | 272 overall; 102 with mental health problems | Stigma was not associated with counseling visits (AOR = 0.92, 95% CI: 0.53, 1.59; P = 0.76). Stigma was not associated with medication use (AOR = 1.11, 95% CI: 0.54, 2.27; P = 0.78). | Group who screened positive for a mental health problem scored higher on the stigma scale compared with those without a diagnosis (score = 2.89, SD, 1.0 vs. score = 2.31, SD, 0.9; F = 17.7; df = 1 and 247; P < 0.001; Cohen's d = 0.54) and were more likely to endorse nearly all of the stigma items (ORs = 2.10–4.15). PTSD was positively associated with counseling and medication visits (AOR = 10.69, 95% CI: 2.97, 38.39; P < 0.05). Negative beliefs about mental health care were negatively associated with counseling and medication visits (AOR = 0.83, 95% CI: 0.72, 0.95; P < 0.05; and AOR = 0.69, 95% CI: 0.56, 0.85; P < 0.05). |
| Kim, 2011 (23) | United States | In-service personnel (regular military) | Cross-sectional | 2,623 overall; 881 with mental health problems | Stigma not associated with treatment utilization for any type of care. Association of anticipated stigma with any type of care/treatment (AOR = 1.09, 95% CI: 0.84, 1.41; P = 0.502). Mental health professional—military (AOR = 1.16, 95% CI: 0.87, 1.54; P = 0.308). Mental health professional—civilian (AOR = 0.93, 95% CI: 0.58, 1.49; P = 0.772). | Top 3 concerns about barriers to care for those with and without mental health problems were all stigma related; however, this did not predict service use. Negative attitudes toward treatment predicted decreased treatment utilization from: Any type of care/treatment (AOR = 0.63, 95% CI: 0.45, 0.87; P = 0.005). Mental health professional—military (AOR = 0.58, 95% CI: 0.41, 0.84; P = 0.004) (nonsignificant result for mental health professional—civilian (AOR = 0.70, 95% CI: 0.39, 1.24; P = 0.219)). |
| Hoerster, 2012 (58) | United States | Veterans | Prospective | 305 | Stigma was not associated with receipt of adequate mental health treatment (9 or more mental health visits) (odds ratios not reported). Receipt of treatment as a continuous variable was not associated with stigma (odds ratios not reported). | Stigma barriers were most commonly endorsed (111 veterans, 37% endorsed at least 1 stigma-related barrier). Those with greater symptom severity and females were more likely to receive adequate treatment after adjustment for either PTSD symptom severity or depression symptom severity and sex, military branch, endorsement of stigma- related barriers, and endorsement of trust-related barriers. PTSD symptom severity (AOR = 1.03, 95% CI: 1.01, 1.05; P = 0.003) and being female (AOR = 4.82, 95% CI: 1.37, 16.99; P = 0.014) were associated with receiving adequate treatment. Depression symptom severity (AOR = 1.06, 95% CI: 1.01, 1.11; P = 0.01) and being female (AOR = 3.98, 95% CI: 1.17, 13.49; P = 0.027) were associated with receiving adequate treatment. |
| Jones, 2013 (53) | United Kingdom | Regular military/reserves | Cross-sectional | 484 overall; 262 with mental health problems | Stigma was not associated with utilization of mental health services for those with mental health problems after adjustment for rank, age, service length, sex, relationship status, and deployment in the last year (AOR = 2.27, 95% CI: 0.57, 3.82; P > 0.05). | Those with common mental health disorders or PTSD symptoms had increased odds of endorsing stigma (AOR = 3.07, 95% CI: 1.95, 4.84; P < 0.05) but not among those drinking alcohol at potentially harmful levels (AOR = 1.08, 95% CI: 0.68, 1.70; P > 0.05). A statistically significant trend was observed for increasing levels of stigma reported from the lowest levels among non–help-seekers who screened negative for mental health problems, through moderate levels among negative screening help-seekers and positive screening help-seekers, to the highest levels among positive screening non–help-seekers (χ2 test for trend = 25.23, P ≤ 0.0001). Over 90% of those that screened positive for a mental health problem endorsed that “Mental health support can be useful for those who need it.” Eighty percent of those that screened positive for a mental health problem endorsed that “It takes courage or strength to get treatment for a psychological problem.” Those that expressed potentially discriminatory views about other people with mental health problems were also more likely to report higher levels of stigma (AOR = 2.66, 95% CI: 1.47, 4.82; P < 0.05). |
| Elnitsky, 2013 (63) | United States | Regular military (Army combat medics) | Cross-sectional | 799 overall; 54 with mental health problems | Positive association of anticipated stigma and utilization of mental health services by combat medics (AOR = 1.61, 95% CI: not reported; P = 0.01). Positive association of anticipated stigma and mental health service utilization by males (AOR = 1.58, 95% CI: 1.09, 2.30). | A nonsignificant association was observed between stigma and mental health service use by female combat medics (AOR = 1.46, 95% CI: 0.78, 2.76). |
Abbreviations: AOR, adjusted odds ratio; CI, confidence interval; OR, odds ratio; PTSD, post-traumatic stress disorder; SD, standard deviation.
Association Between Stigma and Health Service Use From Studies Published in 2004–2014
| First Author, Year (Reference No.) . | Study Location . | Population Type . | Study Type . | Study Size . | Association Between Stigma and Mental Health Service Use . | Other Relevant Findings . |
|---|---|---|---|---|---|---|
| Harpaz-Rotem, 2014 (57) | United States | Veterans | Prospective | 137 | No significant difference in anticipated stigma between those that did not receive mental health treatment (mean = 3.18, SD, 0.87) and those that did receive mental health treatment (mean = 2.94, SD, 1.04; t = 1.224; P = 0.223; df = 134). | Veterans in this study who endorsed greater stigma were not deterred from utilizing mental health services. Multivariate logistic regression revealed that only greater unit support (OR = 1.06, 95% CI: 1.02, 1.10; P = 0.006) and severity of PTSD symptoms (OR = 1.05, 95% CI: 1.02, 1.09; P = 0.002) were associated with initiation of use of mental health services. Study investigates specific symptom clusters and effect on treatment-seeking. Post hoc analysis—PTSD reexperiencing symptoms associated with increased odds of initiating treatment (OR = 1.13, 95% CI: 1.05, 1.23; P = 0.02), numbing symptoms associated with increased odds of retention in treatment (12 or more mental health visits) (OR = 1.15, 95% CI: 1.06, 1.24; P = 0.001). Likelihood of retention in treatment positively associated with greater severity of PTSD symptoms (OR = 1.09, 95% CI: 1.04, 1.15; P > 0.001). |
| Kehle, 2010 (15) | United States | National Guard | Cross-sectional | 424 overall; 117 with mental health problems | Stigma did not significantly predict mental health service utilization when using number of positive stigma items as the predictor (AOR = 1.017, 95% CI: 0.921, 1.122; P > 0.05) or stigma as measured in a high/low median split (AOR = 1.24, 95% CI: 0.745, 2.065; P > 0.05) (model adjusted for mental health status). | Models unadjusted for mental health status found positive attitudes toward mental health treatment (AOR = 1.40, 95% CI: 1.10, 1.79; P < 0.05), receiving therapy in theater (AOR = 2.21, 95% CI: 1.12, 4.33; P < 0.05), severity of illness (need factor score) (AOR = 1.52, 95% CI: 1.18, 1.96; P < 0.01), and in-theater injuries (AOR = 1.98, 95% CI: 1.13, 3.47; P < 0.05) all positively associated with mental health service use. |
| Rosen, 2011 (18) | United States | Veterans | Cross-sectional | 482 | No association of stigma with retrospective reports of initiating therapy (AOR = 1.12, 95% CI: 0.82, 1.52; P > 0.05) or prospectively (after survey time 1) (AOR = 1.07, 95% CI: 0.73, 1.57; P > 0.05). Positive association of stigma and completing 8 or more PTSD psychotherapy visits (AOR = 1.51, 95% CI: 1.00, 2.28; P < 0.05). Positive association between reporting stigma and retrospective reports of use of Veteran Centre counseling services (AOR = 1.69, 95% CI: 1.24, 2.30; P < 0.01). | One in 3 veterans endorsed moderate/high stigma concerns as barriers to care; however, stigma was not retrospectively or prospectively associated with initiating psychotherapy. Those that reported higher levels of stigma concerns were more likely to complete treatment and have used Veteran Centre counseling. Retrospective initiation (prior to survey) and prospective use of PTSD psychotherapy services were positively associated with severity of mental health problem/impairment (AOR = 1.44, 95% CI: 1.01, 1.89; P < 0.01; and AOR = 1.73, 95% CI: 1.21, 2.47; P < 0.01). Retrospective initiation (prior to survey) of PTSD psychotherapy was positively associated with an individual's being diagnosed in a veteran association mental health-care setting rather than a medical setting (AOR = 2.68, 95% CI: 1.65, 4.35; P < 0.01). Prospective initiation of PTSD psychotherapy was associated with being part of a male Iraq/Afghan group (reference, male Vietnam era group) (AOR = 2.95, 95% CI: 1.37, 6.36; P < 0.01). Patients with greater impairment or desire for help did not receive more sessions of psychotherapy. Hence, the amount of care used was not determined by need or desire for help. |
| Pietrzak, 2009 (32) | United States | Veterans | Cross-sectional | 272 overall; 102 with mental health problems | Stigma was not associated with counseling visits (AOR = 0.92, 95% CI: 0.53, 1.59; P = 0.76). Stigma was not associated with medication use (AOR = 1.11, 95% CI: 0.54, 2.27; P = 0.78). | Group who screened positive for a mental health problem scored higher on the stigma scale compared with those without a diagnosis (score = 2.89, SD, 1.0 vs. score = 2.31, SD, 0.9; F = 17.7; df = 1 and 247; P < 0.001; Cohen's d = 0.54) and were more likely to endorse nearly all of the stigma items (ORs = 2.10–4.15). PTSD was positively associated with counseling and medication visits (AOR = 10.69, 95% CI: 2.97, 38.39; P < 0.05). Negative beliefs about mental health care were negatively associated with counseling and medication visits (AOR = 0.83, 95% CI: 0.72, 0.95; P < 0.05; and AOR = 0.69, 95% CI: 0.56, 0.85; P < 0.05). |
| Kim, 2011 (23) | United States | In-service personnel (regular military) | Cross-sectional | 2,623 overall; 881 with mental health problems | Stigma not associated with treatment utilization for any type of care. Association of anticipated stigma with any type of care/treatment (AOR = 1.09, 95% CI: 0.84, 1.41; P = 0.502). Mental health professional—military (AOR = 1.16, 95% CI: 0.87, 1.54; P = 0.308). Mental health professional—civilian (AOR = 0.93, 95% CI: 0.58, 1.49; P = 0.772). | Top 3 concerns about barriers to care for those with and without mental health problems were all stigma related; however, this did not predict service use. Negative attitudes toward treatment predicted decreased treatment utilization from: Any type of care/treatment (AOR = 0.63, 95% CI: 0.45, 0.87; P = 0.005). Mental health professional—military (AOR = 0.58, 95% CI: 0.41, 0.84; P = 0.004) (nonsignificant result for mental health professional—civilian (AOR = 0.70, 95% CI: 0.39, 1.24; P = 0.219)). |
| Hoerster, 2012 (58) | United States | Veterans | Prospective | 305 | Stigma was not associated with receipt of adequate mental health treatment (9 or more mental health visits) (odds ratios not reported). Receipt of treatment as a continuous variable was not associated with stigma (odds ratios not reported). | Stigma barriers were most commonly endorsed (111 veterans, 37% endorsed at least 1 stigma-related barrier). Those with greater symptom severity and females were more likely to receive adequate treatment after adjustment for either PTSD symptom severity or depression symptom severity and sex, military branch, endorsement of stigma- related barriers, and endorsement of trust-related barriers. PTSD symptom severity (AOR = 1.03, 95% CI: 1.01, 1.05; P = 0.003) and being female (AOR = 4.82, 95% CI: 1.37, 16.99; P = 0.014) were associated with receiving adequate treatment. Depression symptom severity (AOR = 1.06, 95% CI: 1.01, 1.11; P = 0.01) and being female (AOR = 3.98, 95% CI: 1.17, 13.49; P = 0.027) were associated with receiving adequate treatment. |
| Jones, 2013 (53) | United Kingdom | Regular military/reserves | Cross-sectional | 484 overall; 262 with mental health problems | Stigma was not associated with utilization of mental health services for those with mental health problems after adjustment for rank, age, service length, sex, relationship status, and deployment in the last year (AOR = 2.27, 95% CI: 0.57, 3.82; P > 0.05). | Those with common mental health disorders or PTSD symptoms had increased odds of endorsing stigma (AOR = 3.07, 95% CI: 1.95, 4.84; P < 0.05) but not among those drinking alcohol at potentially harmful levels (AOR = 1.08, 95% CI: 0.68, 1.70; P > 0.05). A statistically significant trend was observed for increasing levels of stigma reported from the lowest levels among non–help-seekers who screened negative for mental health problems, through moderate levels among negative screening help-seekers and positive screening help-seekers, to the highest levels among positive screening non–help-seekers (χ2 test for trend = 25.23, P ≤ 0.0001). Over 90% of those that screened positive for a mental health problem endorsed that “Mental health support can be useful for those who need it.” Eighty percent of those that screened positive for a mental health problem endorsed that “It takes courage or strength to get treatment for a psychological problem.” Those that expressed potentially discriminatory views about other people with mental health problems were also more likely to report higher levels of stigma (AOR = 2.66, 95% CI: 1.47, 4.82; P < 0.05). |
| Elnitsky, 2013 (63) | United States | Regular military (Army combat medics) | Cross-sectional | 799 overall; 54 with mental health problems | Positive association of anticipated stigma and utilization of mental health services by combat medics (AOR = 1.61, 95% CI: not reported; P = 0.01). Positive association of anticipated stigma and mental health service utilization by males (AOR = 1.58, 95% CI: 1.09, 2.30). | A nonsignificant association was observed between stigma and mental health service use by female combat medics (AOR = 1.46, 95% CI: 0.78, 2.76). |
| First Author, Year (Reference No.) . | Study Location . | Population Type . | Study Type . | Study Size . | Association Between Stigma and Mental Health Service Use . | Other Relevant Findings . |
|---|---|---|---|---|---|---|
| Harpaz-Rotem, 2014 (57) | United States | Veterans | Prospective | 137 | No significant difference in anticipated stigma between those that did not receive mental health treatment (mean = 3.18, SD, 0.87) and those that did receive mental health treatment (mean = 2.94, SD, 1.04; t = 1.224; P = 0.223; df = 134). | Veterans in this study who endorsed greater stigma were not deterred from utilizing mental health services. Multivariate logistic regression revealed that only greater unit support (OR = 1.06, 95% CI: 1.02, 1.10; P = 0.006) and severity of PTSD symptoms (OR = 1.05, 95% CI: 1.02, 1.09; P = 0.002) were associated with initiation of use of mental health services. Study investigates specific symptom clusters and effect on treatment-seeking. Post hoc analysis—PTSD reexperiencing symptoms associated with increased odds of initiating treatment (OR = 1.13, 95% CI: 1.05, 1.23; P = 0.02), numbing symptoms associated with increased odds of retention in treatment (12 or more mental health visits) (OR = 1.15, 95% CI: 1.06, 1.24; P = 0.001). Likelihood of retention in treatment positively associated with greater severity of PTSD symptoms (OR = 1.09, 95% CI: 1.04, 1.15; P > 0.001). |
| Kehle, 2010 (15) | United States | National Guard | Cross-sectional | 424 overall; 117 with mental health problems | Stigma did not significantly predict mental health service utilization when using number of positive stigma items as the predictor (AOR = 1.017, 95% CI: 0.921, 1.122; P > 0.05) or stigma as measured in a high/low median split (AOR = 1.24, 95% CI: 0.745, 2.065; P > 0.05) (model adjusted for mental health status). | Models unadjusted for mental health status found positive attitudes toward mental health treatment (AOR = 1.40, 95% CI: 1.10, 1.79; P < 0.05), receiving therapy in theater (AOR = 2.21, 95% CI: 1.12, 4.33; P < 0.05), severity of illness (need factor score) (AOR = 1.52, 95% CI: 1.18, 1.96; P < 0.01), and in-theater injuries (AOR = 1.98, 95% CI: 1.13, 3.47; P < 0.05) all positively associated with mental health service use. |
| Rosen, 2011 (18) | United States | Veterans | Cross-sectional | 482 | No association of stigma with retrospective reports of initiating therapy (AOR = 1.12, 95% CI: 0.82, 1.52; P > 0.05) or prospectively (after survey time 1) (AOR = 1.07, 95% CI: 0.73, 1.57; P > 0.05). Positive association of stigma and completing 8 or more PTSD psychotherapy visits (AOR = 1.51, 95% CI: 1.00, 2.28; P < 0.05). Positive association between reporting stigma and retrospective reports of use of Veteran Centre counseling services (AOR = 1.69, 95% CI: 1.24, 2.30; P < 0.01). | One in 3 veterans endorsed moderate/high stigma concerns as barriers to care; however, stigma was not retrospectively or prospectively associated with initiating psychotherapy. Those that reported higher levels of stigma concerns were more likely to complete treatment and have used Veteran Centre counseling. Retrospective initiation (prior to survey) and prospective use of PTSD psychotherapy services were positively associated with severity of mental health problem/impairment (AOR = 1.44, 95% CI: 1.01, 1.89; P < 0.01; and AOR = 1.73, 95% CI: 1.21, 2.47; P < 0.01). Retrospective initiation (prior to survey) of PTSD psychotherapy was positively associated with an individual's being diagnosed in a veteran association mental health-care setting rather than a medical setting (AOR = 2.68, 95% CI: 1.65, 4.35; P < 0.01). Prospective initiation of PTSD psychotherapy was associated with being part of a male Iraq/Afghan group (reference, male Vietnam era group) (AOR = 2.95, 95% CI: 1.37, 6.36; P < 0.01). Patients with greater impairment or desire for help did not receive more sessions of psychotherapy. Hence, the amount of care used was not determined by need or desire for help. |
| Pietrzak, 2009 (32) | United States | Veterans | Cross-sectional | 272 overall; 102 with mental health problems | Stigma was not associated with counseling visits (AOR = 0.92, 95% CI: 0.53, 1.59; P = 0.76). Stigma was not associated with medication use (AOR = 1.11, 95% CI: 0.54, 2.27; P = 0.78). | Group who screened positive for a mental health problem scored higher on the stigma scale compared with those without a diagnosis (score = 2.89, SD, 1.0 vs. score = 2.31, SD, 0.9; F = 17.7; df = 1 and 247; P < 0.001; Cohen's d = 0.54) and were more likely to endorse nearly all of the stigma items (ORs = 2.10–4.15). PTSD was positively associated with counseling and medication visits (AOR = 10.69, 95% CI: 2.97, 38.39; P < 0.05). Negative beliefs about mental health care were negatively associated with counseling and medication visits (AOR = 0.83, 95% CI: 0.72, 0.95; P < 0.05; and AOR = 0.69, 95% CI: 0.56, 0.85; P < 0.05). |
| Kim, 2011 (23) | United States | In-service personnel (regular military) | Cross-sectional | 2,623 overall; 881 with mental health problems | Stigma not associated with treatment utilization for any type of care. Association of anticipated stigma with any type of care/treatment (AOR = 1.09, 95% CI: 0.84, 1.41; P = 0.502). Mental health professional—military (AOR = 1.16, 95% CI: 0.87, 1.54; P = 0.308). Mental health professional—civilian (AOR = 0.93, 95% CI: 0.58, 1.49; P = 0.772). | Top 3 concerns about barriers to care for those with and without mental health problems were all stigma related; however, this did not predict service use. Negative attitudes toward treatment predicted decreased treatment utilization from: Any type of care/treatment (AOR = 0.63, 95% CI: 0.45, 0.87; P = 0.005). Mental health professional—military (AOR = 0.58, 95% CI: 0.41, 0.84; P = 0.004) (nonsignificant result for mental health professional—civilian (AOR = 0.70, 95% CI: 0.39, 1.24; P = 0.219)). |
| Hoerster, 2012 (58) | United States | Veterans | Prospective | 305 | Stigma was not associated with receipt of adequate mental health treatment (9 or more mental health visits) (odds ratios not reported). Receipt of treatment as a continuous variable was not associated with stigma (odds ratios not reported). | Stigma barriers were most commonly endorsed (111 veterans, 37% endorsed at least 1 stigma-related barrier). Those with greater symptom severity and females were more likely to receive adequate treatment after adjustment for either PTSD symptom severity or depression symptom severity and sex, military branch, endorsement of stigma- related barriers, and endorsement of trust-related barriers. PTSD symptom severity (AOR = 1.03, 95% CI: 1.01, 1.05; P = 0.003) and being female (AOR = 4.82, 95% CI: 1.37, 16.99; P = 0.014) were associated with receiving adequate treatment. Depression symptom severity (AOR = 1.06, 95% CI: 1.01, 1.11; P = 0.01) and being female (AOR = 3.98, 95% CI: 1.17, 13.49; P = 0.027) were associated with receiving adequate treatment. |
| Jones, 2013 (53) | United Kingdom | Regular military/reserves | Cross-sectional | 484 overall; 262 with mental health problems | Stigma was not associated with utilization of mental health services for those with mental health problems after adjustment for rank, age, service length, sex, relationship status, and deployment in the last year (AOR = 2.27, 95% CI: 0.57, 3.82; P > 0.05). | Those with common mental health disorders or PTSD symptoms had increased odds of endorsing stigma (AOR = 3.07, 95% CI: 1.95, 4.84; P < 0.05) but not among those drinking alcohol at potentially harmful levels (AOR = 1.08, 95% CI: 0.68, 1.70; P > 0.05). A statistically significant trend was observed for increasing levels of stigma reported from the lowest levels among non–help-seekers who screened negative for mental health problems, through moderate levels among negative screening help-seekers and positive screening help-seekers, to the highest levels among positive screening non–help-seekers (χ2 test for trend = 25.23, P ≤ 0.0001). Over 90% of those that screened positive for a mental health problem endorsed that “Mental health support can be useful for those who need it.” Eighty percent of those that screened positive for a mental health problem endorsed that “It takes courage or strength to get treatment for a psychological problem.” Those that expressed potentially discriminatory views about other people with mental health problems were also more likely to report higher levels of stigma (AOR = 2.66, 95% CI: 1.47, 4.82; P < 0.05). |
| Elnitsky, 2013 (63) | United States | Regular military (Army combat medics) | Cross-sectional | 799 overall; 54 with mental health problems | Positive association of anticipated stigma and utilization of mental health services by combat medics (AOR = 1.61, 95% CI: not reported; P = 0.01). Positive association of anticipated stigma and mental health service utilization by males (AOR = 1.58, 95% CI: 1.09, 2.30). | A nonsignificant association was observed between stigma and mental health service use by female combat medics (AOR = 1.46, 95% CI: 0.78, 2.76). |
Abbreviations: AOR, adjusted odds ratio; CI, confidence interval; OR, odds ratio; PTSD, post-traumatic stress disorder; SD, standard deviation.
Association Between Stigma and Care-Seeking Propensity From Studies Published in 2004–2014
| First Author, Year (Reference No.) . | Study Location . | Population Type . | Study Type . | Study Size . | Association Between Stigma and Care-Seeking Propensity . | Other Relevant Findings . |
|---|---|---|---|---|---|---|
| Sudom, 2012 (24) | Canada | Regular military/reserves | Cross-sectional | 2,437 overall; 196 with mental health problems | Stigma was not associated with care-seeking propensity (interest in receiving help) (AOR = 1.1, 95% CI: 0.8, 1.3; P = 0.588). | The top 3 barriers to care were all stigma related (includes those without a mental health problem); however, stigma was not associated with care-seeking propensity after adjustment for mental health status. Those with a mental health problem (and increased severity of mental health problem) were more likely to be interested in care currently: less severe mental health problem (AOR = 5.7, 95% CI: 2.3, 14.2; P = 0.000); more severe mental health problem (AOR = 10.0, 95% CI: 5.3, 18.7; P = 0.000). Those with past mental health service use were more likely to be interested in care currently (AOR = 3.4, 95% CI: 1.9, 6.0; P = 0.000). Structural barriers were associated with greater interest in care (AOR = 1.5, 95% CI: 1.1, 1.8; P = 0.002). Negative attitudes toward mental health care were associated with less interest in care (AOR = 0.6, 95% CI: 0.5, 0.8; P = 0.000). |
| Brown, 2011 (22) | United States | In-service personnel (regular military) | Cross-sectional | 577 | Positive association of anticipated stigma with care-seeking propensity (interest in receiving help) (AOR = 2.29, 95% CI: 1.46, 3.59; P < 0.05). | Recognition of current problem was positively associated with interest in receiving help (AOR = 6.69, 95% CI: 3.66, 12.24; P < 0.05). Past-year care from health-care provider was positively associated with interest in receiving help (AOR = 1.78, 95% CI: 1.11, 2.86; P < 0.05). Negative attitudes to mental health care were associated with lower likelihood of interest in receiving help (AOR = 0.58, 95% CI: 0.38, 0.89; P < 0.05). |
| Jones, 2013 (53) | United Kingdom | Regular military/reserves | Cross-sectional | 484 overall; 262 with mental health problems | Positive association of stigma with care-seeking propensity (interest in receiving help) (AOR = 3.19, 95% CI: 1.80, 5.65; P < 0.05). | Refer to Table 1 for other relevant findings. |
| Blais, 2013 (4) | United States | National Guard/reserves | Cross-sectional | 165 overall; those with mental health problems, not reported. | Nonsignificant correlations of anticipated stigma (measured through PSBCPP-SS and PSOSH) and help-seeking from mental health professional or physician/advanced practice registered nurse. PSBCPP-SS anticipated stigma correlation with help-seeking intention from a mental health professional (r = −0.05, P > 0.05). PSBCPP-SS anticipated stigma correlation with help-seeking intention from physician/advanced practice registered nurse (r = 0.01, P > 0.05). PSOSH anticipated stigma from unit leader, unit members, and family/friends and correlation with help-seeking from mental health professional (r = −0.13, P > 0.05; r = −0.01, P > 0.05; r = 0.03, P > 0.05, respectively). Self-stigma negatively correlated with help-seeking intentions from a mental health professional or physician/advanced practice registered nurse (r = −0.41, P < 0.001; r = −0.24, P < 0.01, respectively). Structural equation modeling was conducted to test the overarching model of help-seeking. Paths were specified from a latent variable of anticipated stigma created from the PSOSH variables with the additional variables of self-stigma, marital status, PTSD severity, history of previous mental health care, and perceived likelihood of redeployment to help-seeking from a mental health professional or physician/advanced practice registered nurse. Paths from self-stigma to help-seeking intentions from both a mental health professional and physician were significantly negative (standardized coefficient = −0.34, P < 0.001; standardized coefficient = −0.20, P < 0.01, respectively). The path from the latent variable of anticipated stigma was nonsignificant (standardized coefficient = −0.01, P > 0.05). | Self-stigma was negatively related to help-seeking intentions; however, anticipated stigma was not related to help-seeking intention (only bivariate correlations). Anticipated stigma from unit leaders was significantly higher than anticipated enacted stigma from unit members (t(147) = 3.66, P = 0.001) and family/friends (t(146) = 9.88, P = 0.001), and anticipated enacted stigma from unit members was significantly higher than anticipated enacted stigma from family/friends (t(149) = 6.92, P = 0.001). Those married (mean = 3.51, SD, 1.88) reported a greater intention to seek mental health care from a mental health professional (F(1, 162) = 7.40, P = 0.01) than those unmarried (mean = 2.72, SD, 1.74). Those married (mean = 3.04, SD, 1.73) reported a greater intention to seek help from a physician/advanced practice nurse (F(1, 162) = 10.90, P = 0.001) than those unmarried (mean = 2.18, SD, 1.51). Those reporting a history of mental health care (mean = 4.35, SD, 1.76) reported a greater intention to seek help from a mental health professional (F(1, 154) = 15.74, P = 0.001) than those without a history of mental health care (mean = 2.92, SD, 1.81). |
| First Author, Year (Reference No.) . | Study Location . | Population Type . | Study Type . | Study Size . | Association Between Stigma and Care-Seeking Propensity . | Other Relevant Findings . |
|---|---|---|---|---|---|---|
| Sudom, 2012 (24) | Canada | Regular military/reserves | Cross-sectional | 2,437 overall; 196 with mental health problems | Stigma was not associated with care-seeking propensity (interest in receiving help) (AOR = 1.1, 95% CI: 0.8, 1.3; P = 0.588). | The top 3 barriers to care were all stigma related (includes those without a mental health problem); however, stigma was not associated with care-seeking propensity after adjustment for mental health status. Those with a mental health problem (and increased severity of mental health problem) were more likely to be interested in care currently: less severe mental health problem (AOR = 5.7, 95% CI: 2.3, 14.2; P = 0.000); more severe mental health problem (AOR = 10.0, 95% CI: 5.3, 18.7; P = 0.000). Those with past mental health service use were more likely to be interested in care currently (AOR = 3.4, 95% CI: 1.9, 6.0; P = 0.000). Structural barriers were associated with greater interest in care (AOR = 1.5, 95% CI: 1.1, 1.8; P = 0.002). Negative attitudes toward mental health care were associated with less interest in care (AOR = 0.6, 95% CI: 0.5, 0.8; P = 0.000). |
| Brown, 2011 (22) | United States | In-service personnel (regular military) | Cross-sectional | 577 | Positive association of anticipated stigma with care-seeking propensity (interest in receiving help) (AOR = 2.29, 95% CI: 1.46, 3.59; P < 0.05). | Recognition of current problem was positively associated with interest in receiving help (AOR = 6.69, 95% CI: 3.66, 12.24; P < 0.05). Past-year care from health-care provider was positively associated with interest in receiving help (AOR = 1.78, 95% CI: 1.11, 2.86; P < 0.05). Negative attitudes to mental health care were associated with lower likelihood of interest in receiving help (AOR = 0.58, 95% CI: 0.38, 0.89; P < 0.05). |
| Jones, 2013 (53) | United Kingdom | Regular military/reserves | Cross-sectional | 484 overall; 262 with mental health problems | Positive association of stigma with care-seeking propensity (interest in receiving help) (AOR = 3.19, 95% CI: 1.80, 5.65; P < 0.05). | Refer to Table 1 for other relevant findings. |
| Blais, 2013 (4) | United States | National Guard/reserves | Cross-sectional | 165 overall; those with mental health problems, not reported. | Nonsignificant correlations of anticipated stigma (measured through PSBCPP-SS and PSOSH) and help-seeking from mental health professional or physician/advanced practice registered nurse. PSBCPP-SS anticipated stigma correlation with help-seeking intention from a mental health professional (r = −0.05, P > 0.05). PSBCPP-SS anticipated stigma correlation with help-seeking intention from physician/advanced practice registered nurse (r = 0.01, P > 0.05). PSOSH anticipated stigma from unit leader, unit members, and family/friends and correlation with help-seeking from mental health professional (r = −0.13, P > 0.05; r = −0.01, P > 0.05; r = 0.03, P > 0.05, respectively). Self-stigma negatively correlated with help-seeking intentions from a mental health professional or physician/advanced practice registered nurse (r = −0.41, P < 0.001; r = −0.24, P < 0.01, respectively). Structural equation modeling was conducted to test the overarching model of help-seeking. Paths were specified from a latent variable of anticipated stigma created from the PSOSH variables with the additional variables of self-stigma, marital status, PTSD severity, history of previous mental health care, and perceived likelihood of redeployment to help-seeking from a mental health professional or physician/advanced practice registered nurse. Paths from self-stigma to help-seeking intentions from both a mental health professional and physician were significantly negative (standardized coefficient = −0.34, P < 0.001; standardized coefficient = −0.20, P < 0.01, respectively). The path from the latent variable of anticipated stigma was nonsignificant (standardized coefficient = −0.01, P > 0.05). | Self-stigma was negatively related to help-seeking intentions; however, anticipated stigma was not related to help-seeking intention (only bivariate correlations). Anticipated stigma from unit leaders was significantly higher than anticipated enacted stigma from unit members (t(147) = 3.66, P = 0.001) and family/friends (t(146) = 9.88, P = 0.001), and anticipated enacted stigma from unit members was significantly higher than anticipated enacted stigma from family/friends (t(149) = 6.92, P = 0.001). Those married (mean = 3.51, SD, 1.88) reported a greater intention to seek mental health care from a mental health professional (F(1, 162) = 7.40, P = 0.01) than those unmarried (mean = 2.72, SD, 1.74). Those married (mean = 3.04, SD, 1.73) reported a greater intention to seek help from a physician/advanced practice nurse (F(1, 162) = 10.90, P = 0.001) than those unmarried (mean = 2.18, SD, 1.51). Those reporting a history of mental health care (mean = 4.35, SD, 1.76) reported a greater intention to seek help from a mental health professional (F(1, 154) = 15.74, P = 0.001) than those without a history of mental health care (mean = 2.92, SD, 1.81). |
Abbreviations: AOR, adjusted odds ratio; CI, confidence interval; PSBCPP-SS, Perceived Stigma and Barriers to Care for Psychological Problems-Stigma Subscale; PSOSH, Perceived Stigma of Seeking Help Scale; PTSD, post-traumatic stress disorder; SD, standard deviation.
Association Between Stigma and Care-Seeking Propensity From Studies Published in 2004–2014
| First Author, Year (Reference No.) . | Study Location . | Population Type . | Study Type . | Study Size . | Association Between Stigma and Care-Seeking Propensity . | Other Relevant Findings . |
|---|---|---|---|---|---|---|
| Sudom, 2012 (24) | Canada | Regular military/reserves | Cross-sectional | 2,437 overall; 196 with mental health problems | Stigma was not associated with care-seeking propensity (interest in receiving help) (AOR = 1.1, 95% CI: 0.8, 1.3; P = 0.588). | The top 3 barriers to care were all stigma related (includes those without a mental health problem); however, stigma was not associated with care-seeking propensity after adjustment for mental health status. Those with a mental health problem (and increased severity of mental health problem) were more likely to be interested in care currently: less severe mental health problem (AOR = 5.7, 95% CI: 2.3, 14.2; P = 0.000); more severe mental health problem (AOR = 10.0, 95% CI: 5.3, 18.7; P = 0.000). Those with past mental health service use were more likely to be interested in care currently (AOR = 3.4, 95% CI: 1.9, 6.0; P = 0.000). Structural barriers were associated with greater interest in care (AOR = 1.5, 95% CI: 1.1, 1.8; P = 0.002). Negative attitudes toward mental health care were associated with less interest in care (AOR = 0.6, 95% CI: 0.5, 0.8; P = 0.000). |
| Brown, 2011 (22) | United States | In-service personnel (regular military) | Cross-sectional | 577 | Positive association of anticipated stigma with care-seeking propensity (interest in receiving help) (AOR = 2.29, 95% CI: 1.46, 3.59; P < 0.05). | Recognition of current problem was positively associated with interest in receiving help (AOR = 6.69, 95% CI: 3.66, 12.24; P < 0.05). Past-year care from health-care provider was positively associated with interest in receiving help (AOR = 1.78, 95% CI: 1.11, 2.86; P < 0.05). Negative attitudes to mental health care were associated with lower likelihood of interest in receiving help (AOR = 0.58, 95% CI: 0.38, 0.89; P < 0.05). |
| Jones, 2013 (53) | United Kingdom | Regular military/reserves | Cross-sectional | 484 overall; 262 with mental health problems | Positive association of stigma with care-seeking propensity (interest in receiving help) (AOR = 3.19, 95% CI: 1.80, 5.65; P < 0.05). | Refer to Table 1 for other relevant findings. |
| Blais, 2013 (4) | United States | National Guard/reserves | Cross-sectional | 165 overall; those with mental health problems, not reported. | Nonsignificant correlations of anticipated stigma (measured through PSBCPP-SS and PSOSH) and help-seeking from mental health professional or physician/advanced practice registered nurse. PSBCPP-SS anticipated stigma correlation with help-seeking intention from a mental health professional (r = −0.05, P > 0.05). PSBCPP-SS anticipated stigma correlation with help-seeking intention from physician/advanced practice registered nurse (r = 0.01, P > 0.05). PSOSH anticipated stigma from unit leader, unit members, and family/friends and correlation with help-seeking from mental health professional (r = −0.13, P > 0.05; r = −0.01, P > 0.05; r = 0.03, P > 0.05, respectively). Self-stigma negatively correlated with help-seeking intentions from a mental health professional or physician/advanced practice registered nurse (r = −0.41, P < 0.001; r = −0.24, P < 0.01, respectively). Structural equation modeling was conducted to test the overarching model of help-seeking. Paths were specified from a latent variable of anticipated stigma created from the PSOSH variables with the additional variables of self-stigma, marital status, PTSD severity, history of previous mental health care, and perceived likelihood of redeployment to help-seeking from a mental health professional or physician/advanced practice registered nurse. Paths from self-stigma to help-seeking intentions from both a mental health professional and physician were significantly negative (standardized coefficient = −0.34, P < 0.001; standardized coefficient = −0.20, P < 0.01, respectively). The path from the latent variable of anticipated stigma was nonsignificant (standardized coefficient = −0.01, P > 0.05). | Self-stigma was negatively related to help-seeking intentions; however, anticipated stigma was not related to help-seeking intention (only bivariate correlations). Anticipated stigma from unit leaders was significantly higher than anticipated enacted stigma from unit members (t(147) = 3.66, P = 0.001) and family/friends (t(146) = 9.88, P = 0.001), and anticipated enacted stigma from unit members was significantly higher than anticipated enacted stigma from family/friends (t(149) = 6.92, P = 0.001). Those married (mean = 3.51, SD, 1.88) reported a greater intention to seek mental health care from a mental health professional (F(1, 162) = 7.40, P = 0.01) than those unmarried (mean = 2.72, SD, 1.74). Those married (mean = 3.04, SD, 1.73) reported a greater intention to seek help from a physician/advanced practice nurse (F(1, 162) = 10.90, P = 0.001) than those unmarried (mean = 2.18, SD, 1.51). Those reporting a history of mental health care (mean = 4.35, SD, 1.76) reported a greater intention to seek help from a mental health professional (F(1, 154) = 15.74, P = 0.001) than those without a history of mental health care (mean = 2.92, SD, 1.81). |
| First Author, Year (Reference No.) . | Study Location . | Population Type . | Study Type . | Study Size . | Association Between Stigma and Care-Seeking Propensity . | Other Relevant Findings . |
|---|---|---|---|---|---|---|
| Sudom, 2012 (24) | Canada | Regular military/reserves | Cross-sectional | 2,437 overall; 196 with mental health problems | Stigma was not associated with care-seeking propensity (interest in receiving help) (AOR = 1.1, 95% CI: 0.8, 1.3; P = 0.588). | The top 3 barriers to care were all stigma related (includes those without a mental health problem); however, stigma was not associated with care-seeking propensity after adjustment for mental health status. Those with a mental health problem (and increased severity of mental health problem) were more likely to be interested in care currently: less severe mental health problem (AOR = 5.7, 95% CI: 2.3, 14.2; P = 0.000); more severe mental health problem (AOR = 10.0, 95% CI: 5.3, 18.7; P = 0.000). Those with past mental health service use were more likely to be interested in care currently (AOR = 3.4, 95% CI: 1.9, 6.0; P = 0.000). Structural barriers were associated with greater interest in care (AOR = 1.5, 95% CI: 1.1, 1.8; P = 0.002). Negative attitudes toward mental health care were associated with less interest in care (AOR = 0.6, 95% CI: 0.5, 0.8; P = 0.000). |
| Brown, 2011 (22) | United States | In-service personnel (regular military) | Cross-sectional | 577 | Positive association of anticipated stigma with care-seeking propensity (interest in receiving help) (AOR = 2.29, 95% CI: 1.46, 3.59; P < 0.05). | Recognition of current problem was positively associated with interest in receiving help (AOR = 6.69, 95% CI: 3.66, 12.24; P < 0.05). Past-year care from health-care provider was positively associated with interest in receiving help (AOR = 1.78, 95% CI: 1.11, 2.86; P < 0.05). Negative attitudes to mental health care were associated with lower likelihood of interest in receiving help (AOR = 0.58, 95% CI: 0.38, 0.89; P < 0.05). |
| Jones, 2013 (53) | United Kingdom | Regular military/reserves | Cross-sectional | 484 overall; 262 with mental health problems | Positive association of stigma with care-seeking propensity (interest in receiving help) (AOR = 3.19, 95% CI: 1.80, 5.65; P < 0.05). | Refer to Table 1 for other relevant findings. |
| Blais, 2013 (4) | United States | National Guard/reserves | Cross-sectional | 165 overall; those with mental health problems, not reported. | Nonsignificant correlations of anticipated stigma (measured through PSBCPP-SS and PSOSH) and help-seeking from mental health professional or physician/advanced practice registered nurse. PSBCPP-SS anticipated stigma correlation with help-seeking intention from a mental health professional (r = −0.05, P > 0.05). PSBCPP-SS anticipated stigma correlation with help-seeking intention from physician/advanced practice registered nurse (r = 0.01, P > 0.05). PSOSH anticipated stigma from unit leader, unit members, and family/friends and correlation with help-seeking from mental health professional (r = −0.13, P > 0.05; r = −0.01, P > 0.05; r = 0.03, P > 0.05, respectively). Self-stigma negatively correlated with help-seeking intentions from a mental health professional or physician/advanced practice registered nurse (r = −0.41, P < 0.001; r = −0.24, P < 0.01, respectively). Structural equation modeling was conducted to test the overarching model of help-seeking. Paths were specified from a latent variable of anticipated stigma created from the PSOSH variables with the additional variables of self-stigma, marital status, PTSD severity, history of previous mental health care, and perceived likelihood of redeployment to help-seeking from a mental health professional or physician/advanced practice registered nurse. Paths from self-stigma to help-seeking intentions from both a mental health professional and physician were significantly negative (standardized coefficient = −0.34, P < 0.001; standardized coefficient = −0.20, P < 0.01, respectively). The path from the latent variable of anticipated stigma was nonsignificant (standardized coefficient = −0.01, P > 0.05). | Self-stigma was negatively related to help-seeking intentions; however, anticipated stigma was not related to help-seeking intention (only bivariate correlations). Anticipated stigma from unit leaders was significantly higher than anticipated enacted stigma from unit members (t(147) = 3.66, P = 0.001) and family/friends (t(146) = 9.88, P = 0.001), and anticipated enacted stigma from unit members was significantly higher than anticipated enacted stigma from family/friends (t(149) = 6.92, P = 0.001). Those married (mean = 3.51, SD, 1.88) reported a greater intention to seek mental health care from a mental health professional (F(1, 162) = 7.40, P = 0.01) than those unmarried (mean = 2.72, SD, 1.74). Those married (mean = 3.04, SD, 1.73) reported a greater intention to seek help from a physician/advanced practice nurse (F(1, 162) = 10.90, P = 0.001) than those unmarried (mean = 2.18, SD, 1.51). Those reporting a history of mental health care (mean = 4.35, SD, 1.76) reported a greater intention to seek help from a mental health professional (F(1, 154) = 15.74, P = 0.001) than those without a history of mental health care (mean = 2.92, SD, 1.81). |
Abbreviations: AOR, adjusted odds ratio; CI, confidence interval; PSBCPP-SS, Perceived Stigma and Barriers to Care for Psychological Problems-Stigma Subscale; PSOSH, Perceived Stigma of Seeking Help Scale; PTSD, post-traumatic stress disorder; SD, standard deviation.
Quality analysis
The review assessed the quality of the eligible papers utilizing the following guideline question areas: method of sample recruitment/selection, response rates, clarity of aims, appropriateness of design to stated objectives, sample size justification, measurement validity and reliability, adequate description of statistical methods, adequate description of basic data, assessment of statistical significance, serendipitous findings, adequate discussion of main findings, selection basis, interpretation of null findings, reporting of all important results, generalization of results, comparison with results to previous literature, and implications of the study for policy and practice (55). Issues of quality are noted in the study characteristics (Web Table 1) and commented upon in the Discussion.
RESULTS
Study selection
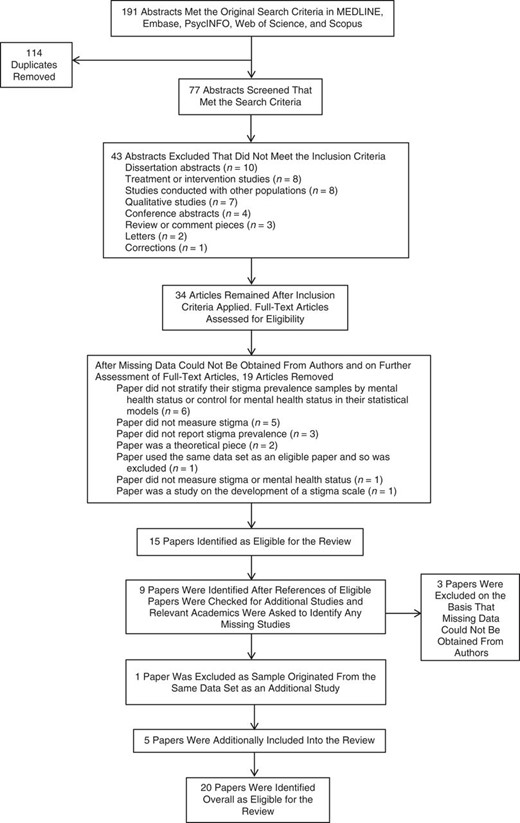
Initial searches returned 191 abstracts that met the initial search criteria (Figure 7). Of these, 114 duplicates were removed, leaving 77 abstracts. Forty-three abstracts were excluded that did not meet the inclusion criteria.
Thirty-four articles remained after the inclusion criteria were applied. The 34 full-text articles were then accessed for eligibility, and 19 articles were removed.
Fifteen papers were eligible for inclusion. After reviewing the references of the 15 eligible papers and sharing the list with other authors (N. F., L. G.), we identified a further 9 papers. After review of the full-text articles of the additional papers, 6 extra papers were considered eligible for inclusion into the study, the other 3 additional studies were excluded, and 1 further paper (56) was removed as it originated from the same data set as a newly included paper that had a larger study sample (15).
Overview of studies
Twenty papers met the review inclusion criteria. Eighteen of the 20 studies were cross-sectional, and 2 papers used a prospective design (57, 58). Out of the 20 eligible papers, those by Ouimette et al. (51) and Rosen et al. (18) utilized the same data set, but the former reports on stigma prevalence and the latter on the association of stigma with mental health service use. Similarly, Hoge et al. (1) and Brown et al. (22) used data sets that overlapped, but the former reports on stigma prevalence and the latter on the association of stigma and help-seeking intention.
The studies were carried out among the military populations of the United States (n = 14), United Kingdom (n = 4), and Canada (n = 1). One paper additionally assessed the militaries from the United Kingdom, the United States, Australia, and New Zealand in a comparative study. Five papers assessed samples in which all participants had probable mental health diagnoses, and 15 studies assessed broader samples including those with and without probable mental health problems. The largest study sample size of those with mental health problems was 2,520; the smallest was 30. In 1 paper, the sample size of those with mental health problems was not reported (4). Seven papers researched current service personnel/active-duty soldiers, 5 papers researched veteran/former service personnel, 3 papers reported on the National Guard, and 5 papers researched a mixture of service personnel, National Guard/reserves, and veteran/former service personnel. All papers contained research participants who were deployed to recent Iraq or Afghanistan conflicts, except 3 papers that also included as part of their sample those deployed to Timor Leste (New Zealand participants (21)) and veterans of the Vietnam era (18, 51).
Measurement of stigma
The majority of papers (n = 18) assessed anticipated stigma by using a core 6-item stigma subscale measuring anticipated stigma and its effect on decisions to seek treatment for psychological problems in military populations (Web Table 1). This was achieved through the use of the Perceived Stigma and Barriers to Care for Psychological Problems-Stigma Subscale (PSBCPP-SS), developed by Hoge et al. (1), Britt et al. (19), and Britt (39). Of these 18 papers, 7 added additional items to the scale (15, 22–24, 53, 59), and 5 of these papers selected and measured fewer items than the core measure (10, 21, 49, 52, 58). Blais and Renshaw (4) added “Perceptions of Stigmatization by Others for Seeking Psychological Help” (60) and “Self-Stigma Associated with Seeking Psychological Help” (43) in addition to the core measure of PSBCPP-SS. Jones et al. (53) also added items from the “Reported and Intended Behaviour Scale” (61). Rosen et al. (18) and Ouimette et al. (51) measured a mixture of stigma facets including discomfort with help-seeking and concerns for social consequences (anticipated stigma) by using a stigma subscale developed from Mansfield et al. (62) and Vogt (46).
The measurement of help-seeking intention was either through the endorsement of different stigma items and their effect on decisions to seek treatment (i.e., “Rate each of the possible concerns that might affect your decision to seek treatment for a psychological problem (e.g., a stress or emotional problem such as depression or anxiety attacks) from a mental health professional (e.g., a psychologist or counselor)”) or through questions assessing care-seeking propensity (e.g., “Are you currently interested in receiving help for a stress, emotional, alcohol, or family problem?”). Additional measurement of help-seeking intention was through self-report of mental health service utilization (e.g., respondents were asked to indicate whether they had received help for a stress, emotional, alcohol, or family-related problem from a treatment provider in the last “x” months) or alternatively by assessing medical records. Three studies assessed “adequate” service utilization or “completion of treatment” (by reporting the count of visits to mental health services with 8–12 visits representing adequate treatment) (18, 57, 58).
Prevalence of anticipated stigma and intentions to seek help
Fourteen studies reported anticipated stigma prevalence per endorsed stigma item. Ouimette et al. (51) used a different stigma measure assessing discomfort with help-seeking and concerns about social consequences and so cannot be directly compared with other studies' prevalence findings; however, the study found that these stigma-related barriers were more salient than institutional factors (not fitting into Department of Veterans Affairs care, staff skill and sensitivity, logistic barriers, etc.). The 13 studies that were comparable by their use of items on the PSBCPP-SS had high levels of variability in the prevalence of endorsed stigma items. Across studies, over the 6 stigma items, I2 ranged from 96.8% to 98.3%. Studies were additionally stratified by country, grouping together studies from the United Kingdom and United States to investigate whether this accounted for heterogeneity. Stratification by country had little effect on the high heterogeneity. For example, the I2 for studies from the United States and United Kingdom for the stigma item, “It would be too embarrassing,” remained at 94.2% and 91.6%, respectively. Hence, meta-analyses here are reported across all studies and stigma items.
When rank ordered by weighted prevalence (Table 3) and forest plots (Figures 1–6), the most frequently endorsed of the core 6 stigma items was being treated differently by leaders and the least frequently endorsed was being blamed for having a mental health problem.
Item Weighted Prevalence From Studies Published in 2004–2014 Using the PSBCPP-SS
| Stigma Item . | Prevalence, % . | 95% Confidence Interval . |
|---|---|---|
| My unit leadership might treat me differently. | 44.2 | 37.1, 51.4 |
| I would be seen as weak. | 42.9 | 36.8, 49.0 |
| Members of my unit might have less confidence in me. | 41.3 | 32.6, 50.0 |
| It would be too embarrassing. | 36.1 | 29.0, 43.2 |
| It would harm my career. | 33.4 | 27.9, 38.9 |
| My leaders would blame me for the problem. | 25.5 | 18.6, 32.5 |
| Stigma Item . | Prevalence, % . | 95% Confidence Interval . |
|---|---|---|
| My unit leadership might treat me differently. | 44.2 | 37.1, 51.4 |
| I would be seen as weak. | 42.9 | 36.8, 49.0 |
| Members of my unit might have less confidence in me. | 41.3 | 32.6, 50.0 |
| It would be too embarrassing. | 36.1 | 29.0, 43.2 |
| It would harm my career. | 33.4 | 27.9, 38.9 |
| My leaders would blame me for the problem. | 25.5 | 18.6, 32.5 |
Abbreviation: PSBCPP-SS, Perceived Stigma and Barriers to Care for Psychological Problems-Stigma Subscale.
Item Weighted Prevalence From Studies Published in 2004–2014 Using the PSBCPP-SS
| Stigma Item . | Prevalence, % . | 95% Confidence Interval . |
|---|---|---|
| My unit leadership might treat me differently. | 44.2 | 37.1, 51.4 |
| I would be seen as weak. | 42.9 | 36.8, 49.0 |
| Members of my unit might have less confidence in me. | 41.3 | 32.6, 50.0 |
| It would be too embarrassing. | 36.1 | 29.0, 43.2 |
| It would harm my career. | 33.4 | 27.9, 38.9 |
| My leaders would blame me for the problem. | 25.5 | 18.6, 32.5 |
| Stigma Item . | Prevalence, % . | 95% Confidence Interval . |
|---|---|---|
| My unit leadership might treat me differently. | 44.2 | 37.1, 51.4 |
| I would be seen as weak. | 42.9 | 36.8, 49.0 |
| Members of my unit might have less confidence in me. | 41.3 | 32.6, 50.0 |
| It would be too embarrassing. | 36.1 | 29.0, 43.2 |
| It would harm my career. | 33.4 | 27.9, 38.9 |
| My leaders would blame me for the problem. | 25.5 | 18.6, 32.5 |
Abbreviation: PSBCPP-SS, Perceived Stigma and Barriers to Care for Psychological Problems-Stigma Subscale.
Association of anticipated stigma with mental health service utilization
Seven studies found no association between endorsed anticipated stigma and mental health-care service utilization, initiation, or completion of treatment (Table 1). Two studies found positive associations between endorsed anticipated stigma and mental health-care service utilization; however, the effects seen were small. For example, there was a positive association found between anticipated stigma and utilization of mental health services by combat medics in general (male and female) and male combat medics (adjusted odds ratio (AOR) = 1.61, 95% confidence interval (CI): not reported, P = 0.01, and AOR = 1.58, 95% CI: 1.09, 2.30, respectively) (63). In the paper by Rosen et al. (18), a positive association was found between stigma and completing 8 or more PTSD psychotherapy visits (AOR = 1.51, 95% CI: 1.00, 2.28, P < 0.05), and a positive association was also found between reporting stigma and retrospective reports of use of veteran center counseling services (AOR = 1.69, 95% CI: 1.24, 2.30, P < 0.01).
Association of anticipated stigma and self-stigma with mental health care-seeking propensity (interest in receiving help)
The findings with regard to this outcome were varied (Table 2). Two studies found no association between anticipated stigma and care-seeking propensity (i.e., stigma was not associated with interest in receiving help for mental health problems) (4, 24). Two studies found a positive association of anticipated stigma and care-seeking propensity—that is, those who endorsed stigma items were 2–3 times more likely to be interested in receiving help: Brown et al. (22) (AOR = 2.29, 95% CI: 1.46, 3.59, P < 0.05) and Jones et al. (53) (AOR = 3.19, 95% CI: 1.80, 5.65, P < 0.05). Finally, 1 study found a negative association between self-stigma and intentions to seek help: Blais and Renshaw (4), using structural equation modeling, reported that paths from self-stigma to individuals' help-seeking intentions from both a mental health professional and a medical doctor were significantly negative (standardized coefficient = −0.34, P < 0.001, and standardized coefficient = −0.20, P < 0.01, respectively).
DISCUSSION
Overall, after a systematic review of this literature, several key findings are apparent. There are a substantial number of studies on stigma and barriers to care with few studies examining how stigma is associated with actual mental health service utilization. A quarter to just over two-fifths of those in the military with mental health problems, across countries and across service/veterans/former service, endorse anticipated stigma as factors that might affect their decision to seek help for mental health problems. Despite the fairly high and consistent prevalence of anticipated stigma, the majority of studies found no association between anticipated stigma and mental health service use or intentions to seek help, and the minority of studies found a positive association. Hence, those that endorsed high anticipated stigma still utilized mental health services or were still interested in seeking help. These findings do not cohere with the majority of evidence in civilian literature, that is, that stigma negatively affects help-seeking from medical/formal sources for those with mental health problems (41). There could be several competing explanations for these findings; however, we discuss the results on stigma prevalence first.
Stigma prevalence
The prevalence of anticipated stigma concerns among those in the military with mental health problems is consistently highest in relation to concerns about unit leadership treating them differently, being seen as weak, and unit members having less confidence in them if they seek help for a mental health problem. These results highlight the importance of individuals' perceptions, be they correct or not, and the influence of prevailing military culture that may dissuade them from seeking help or disclosing mental health problems (27, 52). Individuals in the military can be medically downgraded and taken off weapon handling, particularly if they are put on medication for mental health problems. This can act as a barrier to help-seeking and may be reflected in the anticipated stigma concerns associated with leadership and unit members. However, these stigma concerns may also be a result of safety critical industries similar to those of the fire service, police, or airline pilots, where team safety may rely on the high performance and health of other team members and where mental ill health may be perceived to affect this functioning (64–66). Additionally, the stigma concern that individuals may be seen as weak for seeking help may be an extremely ingrained stigmatizing belief associated with the masculine culture of militaries. Studies have noted this masculine culture in military populations and its negative effects on help-seeking behaviors for mental health problems (11, 14, 45, 47). These concerns persist even after individuals have left service. We propose that cultures, beliefs, and behaviors learned in service may be pervasive into civilian life and continue to affect stigmatizing beliefs (46).
When assessing studies that sat consistently above or below the overall weighted prevalences across the majority of stigma items, we can infer from high heterogeneity that different studies' sample structures and contexts may be factors that interact to affect prevalence outcomes. Prevalence in studies could be affected by service status. Active service personnel have been shown to endorse higher levels of anticipated stigma compared with National Guard or veteran/former service personnel samples (14, 29). Additionally, the National Guard samples of Gorman et al. (59) and Kehle et al. (15) (to a lesser extent) in this review sat consistently below the weighted average across stigma items. This difference in stigma may reflect differences in health-care provision and community cultures while in service between active service personnel and National Guard/reserves. National Guard or reserves may endorse fewer stigmas as they can access local mental health care when demobilized without the same visibility or anticipated stigma from their military community compared with those in active service. The type of mental health problem measured in the sample group could also affect high prevalence. Those with probable PTSD have been shown to endorse stigma items at higher levels than those with depression (14). Hence, studies that utilize more expansive measures for their group “screening positive” for mental health problems may lower their overall prevalence results. Stigma has also been evidenced to be a moving entity that changes over time, with service personnel reporting higher anticipated stigma while deployed compared with postdeployment; hence, studies may differ in stigma prevalence, related to when surveys were taken in relation to deployment (31). Prevalence could also be influenced by country. The majority of United Kingdom studies show consistently higher endorsed anticipated stigma than the majority of US samples. Further comparative work on stigma in the militaries from the United Kingdom and the United States may be worth investigation to explain these differences.
Finally, there is a lack of studies that measure the association of stigma with actual mental health-care service utilization. The majority of papers measure only the effect of stigma on help-seeking intentions, that is, whether a barrier to care “might” affect seeking mental health care, with an assumption that intention would lead to an action. However, we cannot say from these prevalence values whether potential barriers to help-seeking do transpose into help-seeking inaction (or action), and therefore the outcome of interest may not be adequately measured. Additionally, the use of self-report for measuring service utilization may not be a robust way to measure this outcome, as individuals with high levels of stigma may not disclose mental health service use (53).
Association of stigma and help-seeking intentions/service use
The findings that anticipated stigma in the majority of studies was not associated with help-seeking intentions or mental health service use and that in the minority of studies it was positively associated seem a nonintuitive outcome if considering stigma a barrier to help-seeking. Despite individuals in these studies endorsing anticipated stigma, it did not deter their intentions to seek help or affect their actual mental health service use. Several explanations could account for these findings.
It may be that there is an “intention gap” between the intention/nonintention to seek help and the subsequent action or inaction. When looking at intention-behavior relations, we found that Sheeran's empirical review (67) reports that it is the “inclined abstainers” that make up the large majority of the intention gap, that is, those that want to act but choose not to, rather than the “disinclined actors,” that is, those that do not want to perform an act but subsequently do so. However, in the case of individuals in these studies, they would be defined as “disinclined actors,” that is, individuals who note their anticipated stigma, but some of whom subsequently seek help. Other factors may uphold a theory of “disinclined actors” such as the repeated findings that the severity of mental health problems is positively related to help-seeking intentions and mental health service use (18, 24, 57, 58). Hence, it may be that individuals endorse anticipated stigma; however, the severity of their mental health problem, which may lead to crisis points in their lives or functional impairment, overrides the barrier to care of anticipated stigma, causing them to seek help as their mental health problem can no longer be ignored or coped with successfully (16, 68). Jones et al. (53) also uphold the notion that concealment of a mental health problem in service may be difficult because of close health supervision, and therefore individuals may be compelled to seek help by the chain of command when behavioral or psychological disturbances are present.
In addition to this, it may be that facilitators of help-seeking are more powerful than barriers to care (69, 70). Warner et al. (48) found one of the most influential factors in a US military sample for overcoming barriers to seeking care was having family and friends strongly encourage soldiers to get help. This is also supported by the “Theory of Reasoned Action/Planned Behavior,” that intentions to perform an action are shaped by the perceived social pressure to perform/not perform a behavior (71, 72). Indeed, some studies in this review found a positive association between greater unit support and utilization of mental health services (57) and found that decreased unit support predicted increased stigma and barriers to care (32). These findings have also been supported in research that found US commissioned and noncommissioned officers' positive leadership behaviors were predictive of individuals' positive decisions to seek mental health treatment (25). Hence, social support could explain how individuals who are disinclined to seek help subsequently seek help, and it could be an important variable to include in future analyses.
Additionally, it should be noted that stigma may simply not be associated with help-seeking intentions or service use if individuals have not recognized or linked their symptoms with the need for medical help. Fikretoglu et al. (73) showed that 80% of those who might have benefited from mental health treatment failed to recognize their own treatment needs and did not seek help. Equally, those with alcohol problems were the least likely in military studies to recognize their own treatment needs (9, 16, 53). Hence, the impact of stigma on mental health service utilization may not be truly measured if individuals do not perceive they have a problem that might require accessing mental health care.
Alternatively, a positive relationship between stigma and help-seeking intentions/service use could be related to “modified labeling theory,” that is, that having an interest in receiving mental health care makes respondents more aware of stigma from others (74). Hence, the process of thinking about or receiving help makes individuals think more acutely about or experience the repercussions of seeking help; thus, service use or interest in care causes higher stigma rather than stigma causing service use.
Finally, 3 studies found that negative attitudes toward care were negatively associated with help-seeking intentions/mental health service use (22, 24, 32). This finding is also supported by other research that found the most commonly endorsed barriers to care for non–help-seeking service personnel with PTSD were negative attitudes toward treatment (75). It may be that negative attitudes toward mental health care are more important barriers to help-seeking in the military than anticipated stigma and may need future focus in terms of interventions and policy decisions. However, it is not clear at present which intervention strategies will be successful in changing negative attitudes in the military. Previous randomized controlled trials aimed at targeting stigma and negative attitudes toward mental health care in the United Kingdom military found no effect in changing these attitudes (76, 77).
Stigma—types, measurement, and methodology
In these military studies, anticipated stigma was the most commonly assessed, with the majority of studies utilizing the same stigma scale (PSBCPP-SS). Intuitively, this form of stigma may be salient for military populations. Previous research has shown that disclosing a psychological problem in the military is perceived as more stigmatizing than having a physical medical problem (39) and that military personnel may choose not to disclose a mental health problem to avoid being labeled as different from so-called “normal” soldiers, as dictated by norms and cultures within their militaries (45, 78).
However, there have been recent methodological questions explored in the literature as to whether the PSBCPP-SS scale measures anticipated stigma effectively, with some authors utilizing alternative scales such as the “Perceived Stigma of Seeking Help” (4, 79) or “Endorsed and Anticipated Stigma Inventory” tool for military populations (80). Hence, the lack of association found between stigma and help-seeking intentions or service use may be a function of the PSBCPP-SS tool. Recent studies such as that by Blais et al. (79) (subsequently published after the systematic review) have found a negative association between anticipated stigma and intentions to seek help using the Perceived Stigma of Seeking Help tool. Some studies used the PSBCPP-SS tool on veteran/former service study samples with stigma items referencing “units members” and “unit leadership.” These points of reference may not be valid for individuals who have left service, which could have affected responses to these studies. Additional research assessing the comparative validity and utility of stigma scales in military populations would benefit the evidence available in this field.
In the studies included in this review, it is unclear why anticipated stigma was the main construct explored. Only 1 paper measured self-stigma and found a negative effect upon help-seeking (4). Self-stigma appears to be a discreet psychological construct that is unlike public stigma or anticipated stigma (81). For instance, individuals may endorse public stigma, but they may not then internalize this stigma. Self-stigma has been shown to be a considerable deterrent to receiving mental health care in general populations (43); it has also been linked to negative attitudes toward mental health services and to less intentions to seek different forms of mental health treatment (44, 82). Additionally, those who endorse greater self-stigma are less likely to return for further mental health treatment after an initial visit (83). However, from this review, it is largely unknown whether self-stigma has an impact on mental health service use or help-seeking intentions in the military, and it could potentially be an important facet of stigma that may act as a barrier to help-seeking that needs future exploration.
Finally, there are some methodological quality issues that may have affected studies' outcomes. Three papers that found no association of stigma and mental health service utilization drew their samples from treatment-seeking or help-seeking samples, that is, individuals who were able to be sampled because of an initial engagement with Veteran Affairs services or health screening events (18, 57, 58). These samples of help-seeking individuals may not be generalizable to the key population of interest, that is, military populations that do not seek help for mental health problems. Those who have taken the step to attend a health-screening event may be more likely in the future to use mental health services and at the same time endorse high anticipated stigma because of their interaction with mental health services. Hence, current (and future) military cohort studies are best placed to address recruitment of large enough samples of those experiencing mental health problems, who are non–help-seekers and help-seekers, selected on a random basis for ensuring robust results.
There is inconsistency in the use of language used to describe stigma. For example, some papers use the language “self-stigma” or “internal stigma” (10) when referring to items assessed using measures of anticipated stigma. Hence, there is a need within military studies for more clarity in stigma descriptions, definitions, and conceptual frameworks used to explain different forms of stigma (26, 84). The current study suggests that modified versions of the scales used to assess stigma are widely utilized. This may impact upon the validity and reliability of the scales, though many studies do report αs for the modified scales.
Strengths and weaknesses
This is the first systematic review and meta-analysis of the military literature that we are aware of that generates an overview of stigma prevalence, its relationship to mental health problems, and its association with help-seeking intention and service use. Weaknesses of this review include the fact that not all data could be obtained from authors and, therefore, data that could have contributed to findings may have been missed.
Implications and conclusions
This study's key findings have shown that, while anticipated stigma prevalence is high in military populations with mental health problems, the majority of studies found that anticipated stigma was not associated with help-seeking intentions or mental health service utilization, and the minority of studies found a positive association of this relationship.
We propose that these findings may be related to an intention-behavior gap where individuals who are disinclined to seek help are compelled when reaching a crisis point or enabled to seek help by positive facilitators of help-seeking, such as supportive family/friends/unit, to overcome stigma. More research on the role of social networks and their interaction with stigma in the help-seeking process would be valuable. From the information gathered in these studies, we cannot tell how long someone has been “disinclined” before he/she acts to seek help. Delays in treatment may create additional negative impacts on individuals' long-term health outcomes, relationships, or families. Further research could usefully address delays in treatment-seeking associated with stigma. Policies, therefore, could be aimed to encourage early help-seeking and sustained engagement with mental health services to avoid the high social and economic costs of individuals seeking help at crisis points.
It is evident that certain stigma concerns have remained prevalent to various degrees across studies, time periods, countries, for those in service, and for those who have left the military. It is also an issue for concern that individuals may experience stigma as a result of their help-seeking, as research indicates that the stigma of mental illness can often be more damaging than the mental illness itself (85). Questions must be asked regarding antistigma campaigns for military populations, whether they are able to have a large enough effect on stigma concerns, and additionally whether veteran/former service populations can be reached effectively in the promotion of antistigma messages. There may be a need to learn from successful antistigma campaigns aimed at general populations to then adapt these methods to the context of military populations.
We also suggest that the lack of association between stigma and help-seeking may be a result of methodology. This review highlights the different language, terms, and scales used in stigma research. While these terms, scales, and models of stigma are contested, it may be difficult for the field to progress in a cohesive fashion. It is suggested that future theoretical work is needed to inform methodological approaches and stigma scales, which would bear much utility in addressing these issues.
Finally, there may also be the need for research to focus on other potential barriers to help-seeking in military populations, such as self-stigma, negative attitudes toward mental health treatment, or individuals' own recognition of need for mental health care, to help further understand the low proportion of help-seekers for mental health problems in the military.
ACKNOWLEDGMENTS
Author affiliations: King's Centre for Military Health Research, Department of Psychological Medicine, Institute of Psychiatry, Psychology, and Neuroscience, King's College London, London, United Kingdom (Marie-Louise Sharp, Nicola T. Fear, Roberto J. Rona, Simon Wessely, Laura Goodwin); and Academic Department of Military Mental Health, Department of Psychological Medicine, Institute of Psychiatry, Psychology, and Neuroscience, King's College London, London, United Kingdom (Neil Greenberg, Norman Jones).
The King's Centre of Military Health Research receives grant funding from the Ministry of Defence (United Kingdom) and the Department of Defense (United States). Marie-Louise Sharp is funded by the Economic Social Research Council (United Kingdom) and The Royal British Legion.
Conflict of interest: none declared.
REFERENCES
Author notes
Abbreviations: AOR, adjusted odds ratio; CI, confidence interval; PSBCPP-SS, Perceived Stigma and Barriers to Care for Psychological Problems-Stigma Subscale; PTSD, post-traumatic stress disorder.