-
PDF
- Split View
-
Views
-
Cite
Cite
Alvisa Palese, Lucia Lesa, Giulia Stroppolo, Giulia Lupieri, Stefano Tardivo, Silvio Brusaferro, on behalf of Aspiration Research Team, Factors precipitating the risk of aspiration in hospitalized patients: findings from a multicentre critical incident technique study, International Journal for Quality in Health Care, Volume 29, Issue 2, April 2017, Pages 194–199, https://doi.org/10.1093/intqhc/mzw148
Close - Share Icon Share
Abstract
To elucidate factors, other than those clinical, precipitating the risk of aspiration in hospitalized patients.
The Critical Incident Technique was adopted for this study in 2015.
Three departments located in two academic hospitals in the northeast of Italy, equipped with 800 and 1500 beds, respectively.
A purposeful sample of 12 registered nurses (RN), all of whom (i) had reported one or more episodes of aspiration during the longitudinal survey, (ii) had worked ≥3 years in the department, and (iii) were willing to participate, were included.
Antecedent factors involved in episodes of aspiration as experienced by RNs were collected through an open-ended interview, and qualitatively analysed.
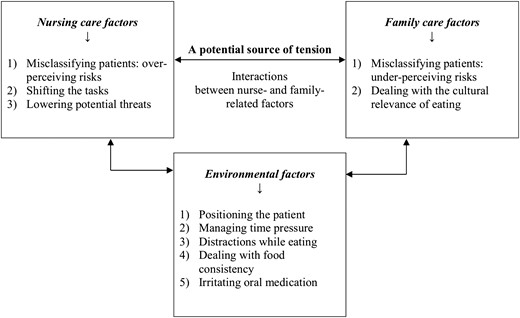
In addition to clinical factors, other factors interacting with each other may precipitate the risk of aspiration episodes during hospitalization: at the nursing care level (misclassifying patients, transferring tasks to other healthcare professionals and standardizing processes to remove potential threats); at the family level (misclassifying patients, dealing with the cultural relevance of eating) and at the environmental level (positioning the patient, managing time pressures, distracting patient while eating, dealing with food consistency and irritating oral medication).
At the hospital level, an adequate nursing workforce and models of care delivery, as well as time for initial and continuing patient and family assessment are required. At the unit level, patient-centred models of care aimed at reducing care standardization are also recommended; in addition, nursing, family and environmental factors should be recorded in the incident reports documenting episodes of aspiration.
Aspiration is defined as the inhalation of oropharyngeal or gastric contents into the larynx and lower respiratory tract [1]. Patients could remain asymptomatic or may develop different symptoms such as dyspnoea, bronchospasm, regurgitation and acute respiratory distress syndrome [2]. Depending on the amount (large or micro-aspiration), nature (food, gastric content) and frequency (acute or chronic), an inhalation event may develop into aspiration pneumonitis or aspiration pneumonia. The first is a chemical injury caused by the inhalation of sterile gastric fluids; the second occurs when a large aspirated volume of oropharyngeal secretions colonized by pathogenic bacteria cause an acute bacterial lung infection [1, 3]. Other aspiration syndromes may occur such as lung abscess or exogenous lipoid pneumonia.
Pulmonary aspiration is recognized as an important cause of serious illness and death [4] and it is considered as the prevalent form of community-acquired pneumonia and healthcare-associated pneumonia (HCAP) [1, 5]. From 0.15 to 2.27 cases of aspiration pneumonia every 10 000 patient days in public hospitals [6] have been reported recently.
Comorbidities in the elderly, increased functional dependence, dementia and dysphagia, are all risk factors for aspiration pneumonia [7–9]. Moreover, given that coughing prevents aspiration, both dysphagia and dystussia have recently been recognized as causal factors of aspiration pneumonia. Therefore, in some patients, aspiration may be silent because of atussia [10, 11].
Nurses play a key role in preventing aspiration and HCAP has been defined as a safety issue depending upon nursing care quality [12, 13]. However, while clinical factors that increase the risk of aspiration have been identified [9] no knowledge to date has been developed with regard to other factors, if any, which may precipitate the clinical risk factors of aspiration. Therefore, the aim of this study is to elucidate the role of other factors in increasing the risk of aspiration in hospitalized patients.
Methods
Study design and setting
A qualitative study based on the Critical Incident Technique (CIT, Table 1) [14, 15] was performed in 2015 after Ethics Committee approval. Three departments admitting elderly patients and located in two Italian Academic Hospitals (800 and 1500 beds, respectively) were approached. In these departments, a strategy aimed at preventing the risk of aspiration pneumonia was implemented by including also a longitudinal survey on aspiration episodes as observed by registered nurses (RNs) responsible for the patients’ care.
The CIT is based upon the concept of
|
The CIT is based upon the concept of
|
The CIT is based upon the concept of
|
The CIT is based upon the concept of
|
Participants
A purposeful sample [16] of RNs who (i) had reported one or more episodes during the longitudinal survey, (ii) had worked ≥3 years in the department [17], and (iii) were willing to participate, were identified. The potential participants were informed regarding the study aims and the confidentiality of the data collected. RN involvement began progressively and their inclusion was completed when data saturation was achieved [18], as judged independently by two researchers. Twelve RNs were interviewed with an average of 8.4 years of nursing experience in the unit (SD [Standard Deviation] 3.9) and an average of 9.2 years in nursing (SD 3.4).
Data collection process, analysis and rigour
An open-ended interview was designed (Table 2); the interviewer was given preliminary training on how to help participants to share their experiences. Each interview was audio-recorded and performed at a time desired by each RN. A comfortable department room was also identified capable of ensuring confidentiality. The duration of the interviews varied between 25 and 40 minutes, 30 minutes on average.
Open-ended questions guiding the interview
1) Introductory statement
|
1) Introductory statement
|
Open-ended questions guiding the interview
1) Introductory statement
|
1) Introductory statement
|
All interviews were transcribed in written format. Each episode was analysed to achieve an in-depth understanding of the significance of antecedents in a given context [14]. Then, an inductive analysis [19] was performed by identifying the mechanism underlying each episode; and comparing all mechanisms emerged, aimed at identifying differences and similarities between the episodes under study. Each researcher developed a descriptive list of elements emerged which was subsequently revised to eliminate redundancies. Then, the list of descriptive elements was collapsed into themes. Researchers agreed on the final list of themes and developed the relationships between them. For each, exemplary quotes were collegially identified and included in an anonymous fashion (e.g. RN 1). Methodological rigour was assured, as reported in Table 3.
|
|
|
|
Findings
Nursing care factors
Misclassifying patients: over-perceiving risks
At ward admission, among other risks (e.g. falls), RNs assess the risk of aspiration, identifying through clinical judgment, whether patients are at risk or not. The majority of patients are diagnosed at risk for aspiration due to their clinical condition (confused, cognitively impaired, affected by neurological disorders or having reported similar difficulties at home) and also due to the fear of nurses that this adverse event might occur. For those patients at risk, RNs decide a specific plan of care, incorporating thickening agents, pill crushing and a specific diet. Patients who are classified as not at risk receive a diet free from these restrictions.
The risk of aspiration as judged at admission is not assessed over time either for those at risk or for those not at risk, because of nursing workloads
‘we are not able to catch the evolution of the risk over time’ (RN 1)
Therefore, their care plan aimed (or not) at preventing aspiration, remains stable over time and preventive strategies are directed only at patients considered at risk. Those patients not diagnosed at risk are the most complex, since their early conditions do not presume a potential risk of aspiration, and a second risk assessment is not always possible. They may develop variations due to clinical evolution and also hospitalization itself may increase the risk of aspiration
‘Patients’ disorientation can be worsened by the hospital environment, by the different pace or by being unfamiliar with healthcare personnel’ (RN 2)
Task shifting
Mealtime is the most critical moment in which aspiration events could occur. Mealtime also represents an important chance for the RNs to come into contact with the patient and to perform continuing surveillance; however, since these tasks are usually delegated to nurse assistants (NAs) who have received brief training, the chances to assess the patient and his/her trajectory actually decreases. Moreover, handovers between NAs and RNs are conditioned by intense workloads and the likelihood of communicating patients’ swallowing abilities or other clinical data may be threatened.
Task shifting also involves nursing students: they are rarely engaged in feeding patients; therefore, they are less experienced in detecting patients at risk; in recognizing early aspiration signs and symptoms, as well as in promptly recognizing the emerging new risks due to changes in patient clinical conditions.
In addition, the high number of patients who require help is often unmanageable for NAs, since providing feeding help requires a certain amount of time. Thus, family members are often involved in the process
‘We delegate nutrition to relatives, giving some advice such as “be careful, go slow”’ (RN 6)
Patients judged at risk are safeguarded, since their relatives are informed and trained. However, in those patients not diagnosed at risk at hospital admission, it is more difficult to inform relatives with regard to the need to continuously adapt their approach, when the clinical conditions change.
Lowering potential threats
Since it is difficult to assess patient risk evolution due to the excessive workload and task shifting, RNs standardize nutrition and hydration with patients considered at risk, using different methods such as thickening agents and soft diets. These strategies remain stable during the whole duration of hospital stay, even in the case of patients who could manage a meal plan free from restrictions because their clinical condition has improved. Nurses are aware that they enact a protective strategy instead of a proactive one; however, changing the consistency of food would imply managing patients’ first meal in order to supervise them, but nurses are always constrained by time shortages
‘I would definitively love to manage the patient's first meal, just to see how it goes, but this is not always possible’ (RN 6)
Family care factors
Misclassifying patients: under-perceiving risks
It is a challenge for patients and caregivers to understand the relationship existing between the unpredictable clinical condition and the risk of aspiration. In the first assessment performed at admission, patients and family caregivers are used to reporting their nutritional habits at home which are expected to be maintained.
‘He has been eating normally so far, so he has to do it here as well’ (RN 3)
Thus, they are surprised when the RNs tell them to be careful when eating or when they provide a soft diet. Moreover, relatives may not recognize gurgling or respiratory symptoms, which could also have occurred at home but have a different relevance at the hospital level. Therefore, it often happens that they feed the patient even when it is not appropriate
‘He was feeding the patient and he did not even notice he was gurgling’ (RN 4)
Patients also consider their former habits as a fixed reference point
‘I used to do the same at home’ (RN 5)
Patients and families would rather return to their usual habits as soon as possible and sometimes violate nurses’ prescriptions by administering homemade food.
Dealing with the cultural relevance of eating
Nutrition represents an indicator of well-being and a strategy to recover health in the culture of both patients and caregivers. As soon as patients are hospital admitted, the caregivers’ first thoughts are typically about nutrition
‘Can we give him food?’ (RN 6)
Patients and relatives act according to this cultural pattern, in which food must be varied in type and consistency, as well as abundant in quantity in order to help coping with illness.
‘they believe that..if you don't eat you won't heal’ (RN 4)
The same cultural pattern influences family intervention also when patient clinical conditions are compromised
‘When the patient is sleepy and barely opens his mouth, you wait and try again later! Instead, families wake him up, they stress him until he opens his mouth, and it typically ends up with him coughing’ (RN 4)
Moreover, caregivers have the tendency to feed patients more than necessary because they do not know how else to be helpful throughout the caring and treatment process
‘They can't help… so they feel powerless, they try any way to feel useful’ (RN 5)
Paid caregivers who get a salary from looking after a patient by families, are perceived to be an increased risk for patients: they believe that they are evaluated by families in accordance with the amount of intake.
A potential source of tension
Interaction between nurse- and family-related factors
Nurses perceive the hidden tension surrounding patients’ nutrition. When they decide on a diet as a preventive strategy, relatives complain that patients are not getting enough food and that their nutritional plan is not satisfactory.
‘He sad that he hasn't been eating for an entire week’ (RN 8)
On the other hand, for relatives it is difficult to understand the prescriptions, even when RNs provide appropriate information. Cultural patterns regarding nutrition prevail
‘They persist and persist!’ (RN 4)
The interactions between nursing care- and family care-factors result in mutual misunderstandings which may increase the risk of aspiration episodes.
Environmental factors
Positioning the patient
Nurses stress the importance of proper patient positioning during oral intake, since an adequate sitting position minimizes the risk of aspiration. However, hospital beds are not sufficiently adjustable to ensure a proper position; RNs and relatives have to position the patient manually and two healthcare workers are required to prevent musculoskeletal injuries, but most of the times staff members have to move the patient alone. When RNs provide medication they also think about guaranteeing patient safety during meals, especially if nobody can help the patient consume the meal because of staff shortages.
‘I tend to start placing patients while already administering medication, saying “breakfast is coming!”’ (RN 5)
Managing time pressure
It is important to comply with the patient's pace during mealtime; however, relatives, volunteers or NAs, feel time pressures thus increasing the risk of aspiration.
‘volunteers and caregivers are usually in a hurry’ (RN 1)
Due to the intense workloads of NAs in charge of feeding patients, they care for patients hastily, sometimes without matching their pace or taking the breaks they need
‘He has to provide 40 breakfasts, then go around again and help feed 20 patients who are not able to self-feed’ (RN 1, RN 5, RN 6)
Distraction while eating
The patient must focus on the action of mastication and swallowing to fulfil proper nourishment; especially the elderly should not carry out multiple tasks at the same time
‘they must take one thing at a time’ (RN 4)
A noiseless and interference-free environment should be ensured. Instead, patients are exposed to many distractions due to the chaotic environment: RNs have reported episodes in which caregivers kept talking to the patient during mealtime, asking them to answer while swallowing; other episodes in which NAs came into the patient room asking them to do something while eating.
Dealing with food consistency
It is difficult for patients to adapt their mastication and swallowing habits to the consistency of the food served in hospital, since it is different from the consistency they are used at home or in nursing homes. Patients have to deal with a food thickness they are not used to, which make them confused. When tea is served with dry biscuits or broth with pasta, patients are not able to deal with the two coexisting consistencies—the liquid and solid—thus, they cannot control swallowing efficiently.
‘It's like a double concept, they don't comprehend if they have to inhale or chew. In the elderly, the process fails at a cognitive level, because they are used to drinking the broth, therefore they drink the broth. When they suck the liquid, the pasta comes as a surprise!’ (RN 5)
The appropriate consistency is also affected by the centralized management processes of the hospital, which ends up dehydrating and drying the meals. On the other hand, when the semi-solid food ordered for patients does not have the right consistency, RNs have to add thickening agents in order to get the creamy consistency which helps the patient become familiar with it as well as controlling it in the mouth before swallowing. Blended foods and semi-solid foods sometimes lack taste and patients express their dissatisfaction
‘Patients usually say “I always eat the same foods”’ (RN 7)
Irritating oral medication
Nurses report that medication administration may play a role in some episodes: when there is a need to crush pills, the resulting powder can be easily inhaled by patients if not properly mixed into the preparation. The powder tends to irritate oral mucosa triggering the cough reflex, which could expose the patient to the risk of adverse events; the cough could also be confused with a case of aspiration, resulting in the activation of unnecessary preventive strategies such as an inappropriate diet. Three medications are reported by RNs as increasing the risk
‘Paracetamol-Codein, its smell is really strong’ (RN 7)
‘Oral lactulose, its oily consistency’ (RN 6)
‘Potassium syrup, it can irritate’ (RN 8)
Discussion
This is the first study aimed at exploring factors, other than those clinical based upon pathophysiology mechanisms [7, 9, 11], which may increase the occurrence of aspiration in hospitalized patients. In accordance with the findings, the potential source of harm and the underlying mechanisms [20–22] rely on nursing and family care, interacting with each other and with the environment, that may moderate the risk of aspiration.
Clinical nurses play a key role in preventing aspiration given that they may recognize early disphagia and atussia, cognitive impairments or changes in the clinical condition; they may also help patients with feeding, tailoring specific interventions. However, in line with Kane et al. [12] who documented that 19% of variance in HCAP occurrence is associated with nursing care, nursing workloads, inadequate models of care delivery and care standardization, which have emerged as factors precipitating the risk of aspiration.
The likelihood of identifying and taking care of patients who are at risk of aspiration is affected by nursing education, given that students may have limited clinical experience [23]. In addition, on the basis of their clinical judgment, based mainly on observation, RNs tend to misclassify patients at admission and consider most of them at risk for aspiration due to fear of the occurrence of this adverse event [24]. They then seek to lower the risk by adopting specific care plans. In contrast, those patients not identified at risk, whose condition may change over time, receive standardized care in terms of nutrition and surveillance. Therefore, the escalation or de-escalation of preventive strategies aimed at protecting patients at different risks of aspiration is rejected in favour of a standardized approach, where those patients as at risk receive inappropriate care and nutrition, and those not at risk may be exposed to aspiration when their clinical condition changes.
Patient assessment has been recognized as a crucial factor for early detection of each variation of clinical condition [25] and accuracy is often threatened by the limited time available. In our study, the limited RN exposure to patients reduces the opportunity to observe their clinical evolution; nursing shortages, models of care based on task division performed under time pressures, and lack of implementation of tools estimating the risks, may reduce surveillance effectiveness [26, 27].
Relatives assume the role of ‘staff extenders’ in performing specific tasks such as feeding, due to a lack of resources; with the increased family participation [28] there is a need to redesign strategies for their appropriate involvement. Relatives are in a transition process during the length of stay of a patient in hospital; cultural beliefs, attitudes and previous knowledge may influence their capability of ensuring effective care. Therefore, developing a partnership between healthcare workers and relatives may result in increased safety and compliance [29].
Environmental factors have also emerged: some seem to be specific to the units involved (e.g. bed features), while others seem to be more common, such as negative distractions [30] and irritating medications that may precipitate the risk of aspiration. In addition, some are modifiable (e.g. distractions) while others are not (e.g. some irritating medications).
Nursing care-, family- and environmental-factors, in addition to clinical ones, may precipitate the risk of aspiration in patients admitted to hospital: situational awareness [31] as an individual perception, comprehension and the subsequent projection of what is going [24] play a key role in preventing aspiration by moderating surveillance, educating relatives and detecting early those environmental conditions which may increase the risk of aspiration.
Several limitations affect this study: only RNs who witnessed a food aspiration event were included and findings may not be valid for cases of gastric aspiration [1]. In addition, RNs reporting evident episodes were involved as clinically diagnosed at the bedside. Therefore, factors involved in silent aspiration occurring in patients with atussia [11] were not explored. Moreover, the study was developed inside of a small-scale project [32] and findings emerged should be validated on a larger scale.
However, at the hospital level, adequate nursing workforces and models of care delivery as well as time for initial and continuing patient and relatives assessment, is required. At the unit level, patient-centred models of care, aimed at reducing standardization are also recommended; in addition, nursing-, family- and environmental-factors should be recorded in the incident reports documenting episodes of aspiration. Tools capable of increasing the accuracy of diagnosing patients at risk for aspiration and in detecting changes over time, should be implemented in order to reduce misclassifications. Continuing to educate nurses in order to increase their situation awareness, capable of detecting over time the risk of aspiration, educating relatives in appropriate feeding and environmental assessment, are also recommended.
Acknowledgements
We thank the RNs who shared their experiences with researchers.
Funding
None
References
Author notes
Aspiration Research Team: Luigi Castriotta, Francesca Valent, Stefania Degan, Daniela De Corti, Fabrizio Bellomo, Academic Hospital Santa Maria della Misericordia Udine, Italy; Irene Aprili Andrea Strenghetto, Elisa Cametti, Post Graduation School of Hygiene and Preventive Medicine, University of Verona, Italy