-
PDF
- Split View
-
Views
-
Cite
Cite
Gina Åsbø, Torill Ueland, Beathe Haatveit, Thomas Bjella, Camilla Bärthel Flaaten, Kristin Fjelnseth Wold, Line Widing, Magnus Johan Engen, Siv Hege Lyngstad, Erlend Gardsjord, Kristin Lie Romm, Ingrid Melle, Carmen Simonsen, The Time is Ripe for a Consensus Definition of Clinical Recovery in First-episode Psychosis: Suggestions Based on a 10-Year Follow-up Study, Schizophrenia Bulletin, Volume 48, Issue 4, July 2022, Pages 839–849, https://doi.org/10.1093/schbul/sbac035
Close - Share Icon Share
Abstract
A consensus definition of clinical recovery in first-episode psychosis (FEP) is required to improve knowledge about recovery rates in this population. To propose criteria for a future consensus definition, this study aims to investigate rates of clinical recovery when using a standard definition (full psychotic symptom remission and adequate functioning for minimum one year) across both affective and nonaffective FEP groups (bipolar spectrum and schizophrenia spectrum disorders). Second, we aim to explore changes in rates when altering the standard definition criteria. Third, to examine the extent to which healthy controls meet the functioning criteria.
In total, 142 FEP participants and 117 healthy controls preselected with strict criteria, were re-assessed with structured clinical interviews at 10-year follow-up.
A total of 31.7% were in clinical recovery according to the standard definition, with significantly higher recovery rates in bipolar (50.0%) than in schizophrenia spectrum disorders (22.9%). Both groups’ recovery rates decreased equally when extending duration and adding affective symptom remission criteria and increased with looser functioning criteria. In healthy controls, 18.8% did not meet the standard criteria for adequate functioning, decreasing to 4.3% with looser criteria.
Findings suggest that clinical recovery is common in FEP, although more in bipolar than in schizophrenia spectrum disorders, also when altering the recovery criteria. We call for a future consensus definition of clinical recovery for FEP, and suggest it should include affective symptom remission and more reasonable criteria for functioning that are more in line with the general population.
Introduction
Psychotic disorders continue to be viewed as chronic,1 although it has been firmly established that many will fully recover.2–4 As hope is important for recovery, this pessimism is potentially detrimental.5–7 What the definition of “recovery” should entail for people with psychotic disorders remains unclear.8–10 A distinction has been made between personal recovery, a process of finding subjective quality of life regardless of symptoms, and clinical recovery, an observer-rated outcome of symptomatic remission and adequate functioning for a given duration.10 There is no consensus definition for clinical recovery or adequate functioning in psychotic disorders, despite the Remission in Schizophrenia Working Group’s (RSWG) consensus definition of symptomatic remission.11
Reviews of clinical recovery in psychotic disorders12–14 have included studies with varied illness durations and follow-up periods, precluding a conclusion regarding long-term outcome. A few long-term (7.5–20 years) follow-up studies have recruited participants within the first year of either onset or treatment of psychosis, known as first-episode psychosis (FEP).15–19 These studies have established that individuals with FEP can gain stable symptomatic remission,18 adequate functioning,15 and clinical recovery with rates ranging from 14% to 35.2%.16,17,19
This variance in clinical recovery rates across these FEP studies is partly due to methodological differences.13 First, the majority defined FEP as nonaffective psychosis (schizophrenia spectrum disorders), excluding affective psychoses (bipolar and major depressive disorder with psychosis).15,16,20 This reduces the observed clinical recovery rates13,21 as nonaffective psychosis studies demonstrate lower rates (13.5%)12 than those including affective psychosis (37.9%).13 In FEP studies that included affective psychoses17–19 and in studies within the framework of first-episode affective psychosis (FEAP),22 the affective samples are rarely divided into unipolar or bipolar disorders. Thus, with the exception of a few studies including first-episode mania (FEM),23 there is a dearth of knowledge about the long-term course of first-episode psychotic bipolar disorder.
The reviewed FEP studies also differ in their definition of clinical recovery.12,13 The required duration of the period necessary for recovery varies from 6 months to 2 years across studies. Symptomatic remission of psychosis is generally well-defined and based on the RSWG consensus definition.11 However, the remission of affective symptoms that make up the diagnostic criteria are not examined in FEP-studies that include affective psychotic disorders, even though it logically should.17–19Adequate functioning lacks a unified definition, although consensus criteria have been suggested.24 Thus, studies differ in requiring any paid-, part-time- or full-time employment to meet functioning criteria.15,17,20 Establishing consensus criteria for adequate functioning is essential, as functional loss is the greatest barrier to clinical recovery in psychotic disorders.25 The majority will achieve symptomatic remission (50%–75%), yet half of them will remain functionally impaired,13 especially related to employment.17 These criteria do not consider that unemployment or poor occupational functioning could be due to systemic factors that are not illness-related, with full-time employment being particularly difficult to reach. Strict functioning criteria have been used to establish a proof-of-concept that many individuals with psychotic disorders without doubt achieve full clinical recovery. Still, we should consider whether these requirements exceed the functioning level in the general population,18 thus causing unwarranted pessimism. Investigating to what extent healthy controls meet strict functioning criteria could help evaluate whether they are an unduly stringent norm.
Due to the above unanswered questions we have the following aims: (1) Investigate the rate of clinical recovery in a 10-year follow-up across a sample of first-episode schizophrenia spectrum and psychotic bipolar spectrum disorders, using a standard definition of clinical recovery. (2) Examine how altering the recovery criteria influence recovery rates, by including the addition of affective symptomatic remission and the use of looser criteria for adequate functioning. (3) Investigate the rate of adequate functioning in a healthy control group using both standard and looser criteria. Finally, based on our findings, we will propose criteria for a potential future consensus definition of clinical recovery in psychotic disorders.
Methods
Participants
A sample of participants with FEP were recruited from 2004 to 2012 to the Thematically Organized Psychosis (TOP) study at the Norwegian Centre for Mental Disorders Research (NORMENT) from the majority of in- and outpatient psychiatric services in the Oslo area in Norway. Participants were invited to a 1-year follow-up assessment and a 10-year follow-up assessment that was completed between 2015 and 2021. FEP was for the purpose of the study defined as recruitment within the first 52 weeks after start of first adequate treatment (antipsychotic medication in adequate dosage for 12 weeks or until remission, or psychiatric hospitalization for a psychotic episode). Other inclusion criteria were meeting the criteria for a DSM-IV diagnosis of a psychotic disorder within the schizophrenia or bipolar spectrum (see below), adequate Scandinavian language skills, age 18–65 years and ability to give informed consent. Exclusion criteria were brain injury requiring hospitalization, neurological or other uncontrolled medical condition causing psychotic symptoms (organic psychosis) at baseline.
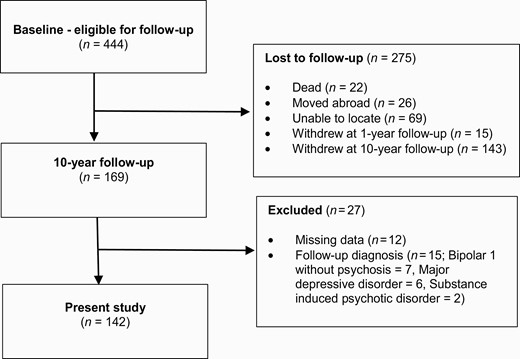
Among the 444 participants eligible for the TOP 10-year follow-up after baseline, 169 completed assessment at 10-year follow-up i.e. with a 38.1% retention rate. See figure 1 for a description of participants. Among our 10-year follow-up sample, 108 participants had also been assessed at 1-year follow-up. Participants were divided into the two diagnostic groups at 10-year follow-up; schizophrenia spectrum disorder (Schizophrenia, Schizophreniform disorder, Schizoaffective disorder, and “other psychoses” (Delusional disorder, Brief psychotic disorder, and Psychotic disorder not otherwise specified)) or bipolar spectrum disorder with psychosis (Bipolar I disorder, Bipolar II disorder and Bipolar disorder not otherwise specified). See table 1 for number of participants within each diagnostic subgroup. After follow-up assessment, 27 participants were excluded from the present part of the study due to either a revised diagnosis outside of the schizophrenia or psychotic bipolar spectrums, or inadequate information to determine the presence of clinical recovery. Thus, the final sample consisted of 142 participants at 10-year follow-up.
Demographic and Clinical Characteristics in Healthy Controls and Total Sample, and between Schizophrenia and Bipolar Spectrum Groups at 10-year Follow-up.
| . | . | Healthy Controls (n = 117) . | Total Sample (n = 142) . | Chi-square/t-test/Mann Whitney . | . | . | Schizophrenia Spectrum (n = 96) . | Bipolar Spectrum (n = 46) . | Chi-square/t-test/Mann Whitney . | . | . |
|---|---|---|---|---|---|---|---|---|---|---|---|
| . | . | . | . | χ2/t/U . | p . | V/D . | . | . | χ2/t/U . | p . | V/D . |
| Demographic | |||||||||||
| Gender, female | 49 (41.9) | 67 (47.2) | χ2 = 0.73 | .452 | .053 | 40 (41.7) | 27 (58.7) | χ2 = 3.62 | .073 | .160 | |
| Age | M (SD) | 40.3 (7.6) | 37.7 (8.3) | t = −2.61 | .010 | −0.325 | 36.9 (8.3) | 39.2 (8.2) | t = −1.56 | .121 | −0.280 |
| Country of origin | χ2 = 20.1 | .000 | .29 | χ2 = 0.00 | 1.000 | −0.006 | |||||
| Norway | 115 (98.3) | 98 (69.0) | 66 (79.5) | 32 (80.0) | |||||||
| Other | 2 (1.8) | 25 (17.6) | 17 (20.5) | 8 (20.0) | |||||||
| In relationship, current | 90 (76.9) | 65 (45.8) | χ2 = 25.90 | .000 | .316 | 39 (40.6) | 26 (56.5) | χ2 = 3.17 | .105 | .149 | |
| Education, years | M (SD) | 15.2 (2.3) | 13.6 (2.5) | t = −5.16 | .000 | −0.682 | 12.9 (2.5) | 14.8 (2.1) | t = −4.00 | .000 | −0.790 |
| Clinical | |||||||||||
| Diagnosis, 10 years | |||||||||||
| Schizophrenia | 55 (38.7) | 55 (57.2) | - | ||||||||
| Schizophreniform | 1 (0.7) | 1 (1.0) | - | ||||||||
| Schizoaffective | 15 (10.6) | 15 (15.6) | - | ||||||||
| Other Psychosesa | 25 (17.6) | 25 (26.0) | - | ||||||||
| Bipolar 1 Disorder | 42 (29.6) | - | 42 (91.3) | ||||||||
| Bipolar 2 Disorder | 3 (2.1) | - | 3 (6.5) | ||||||||
| Bipolar NOS | 1 (0.7) | - | 1 (2.2) | ||||||||
| Psychotic ep. FUb | Mdn (ran) | 2 (0–40) | 2 (0–10) | 2 (0–40) | U = 1830.50 | .217 | |||||
| Manic ep. FUb | Mdn (ran) | 1 (0–42) | 1 (0–4) | 2 (0–42) | U = 333.00 | .020 | |||||
| Depressive ep. FUb | Mdn (ran) | 2 (0–48) | 2 (0–32) | 3 (0–48) | U = 1199.00 | .206 | |||||
| PANSSc | M (SD) | ||||||||||
| Positive | 7.4 (4.1) | 8.4 (4.4) | 5.4 (2.2) | t = 4.50 | .000 | .806 | |||||
| Negative | 9.4 (5.2) | 10.2 (5.9) | 7.8 (2.8) | t = 2.63 | .009 | .472 | |||||
| Disorganized | 4.2 (2.0) | 4.5 (2.3) | 3.6 (0.9) | t = 2.71 | .008 | .486 | |||||
| Excited | 4.7 (1.4) | 4.9 (1.6) | 4.5 (1.0) | t = 1.55 | .123 | .279 | |||||
| Depressive | 6.4 (3.3) | 6.5 (3.2) | 6.1 (3.5) | t = 0.59 | .559 | .105 | |||||
| CDSSd | M (SD) | 3.1 (4.4) | 3.1 (4.5) | 2.9 (4.1) | t = 0.21 | .835 | .039 | ||||
| YMRSe | M (SD) | 3.3 (4.0) | 3.9 (4.4) | 2.0 (2.7) | t = 2.62 | .010 | .475 | ||||
| GAF-Ff | M (SD) | 60.5 (17.7) | 59.4 (16.5) | 69.1 (17.2) | t = -4.24 | .000 | −0.761 | ||||
| AUDITg | Mdn (ran) | 3 (0–28) | 4 (0–28) | 3 (0–20) | U = 1646.50 | .626 | |||||
| DUDITh | Mdn (ran) | 0 (0–42) | 0 (0–42) | 0 (0–23) | U = 1421.50 | .034 | |||||
| Medicated, psychotropic | 95 (66.9) | 65 (69.1) | 30 (65.2) | χ2 = 0.22 | .701 | .040 |
| . | . | Healthy Controls (n = 117) . | Total Sample (n = 142) . | Chi-square/t-test/Mann Whitney . | . | . | Schizophrenia Spectrum (n = 96) . | Bipolar Spectrum (n = 46) . | Chi-square/t-test/Mann Whitney . | . | . |
|---|---|---|---|---|---|---|---|---|---|---|---|
| . | . | . | . | χ2/t/U . | p . | V/D . | . | . | χ2/t/U . | p . | V/D . |
| Demographic | |||||||||||
| Gender, female | 49 (41.9) | 67 (47.2) | χ2 = 0.73 | .452 | .053 | 40 (41.7) | 27 (58.7) | χ2 = 3.62 | .073 | .160 | |
| Age | M (SD) | 40.3 (7.6) | 37.7 (8.3) | t = −2.61 | .010 | −0.325 | 36.9 (8.3) | 39.2 (8.2) | t = −1.56 | .121 | −0.280 |
| Country of origin | χ2 = 20.1 | .000 | .29 | χ2 = 0.00 | 1.000 | −0.006 | |||||
| Norway | 115 (98.3) | 98 (69.0) | 66 (79.5) | 32 (80.0) | |||||||
| Other | 2 (1.8) | 25 (17.6) | 17 (20.5) | 8 (20.0) | |||||||
| In relationship, current | 90 (76.9) | 65 (45.8) | χ2 = 25.90 | .000 | .316 | 39 (40.6) | 26 (56.5) | χ2 = 3.17 | .105 | .149 | |
| Education, years | M (SD) | 15.2 (2.3) | 13.6 (2.5) | t = −5.16 | .000 | −0.682 | 12.9 (2.5) | 14.8 (2.1) | t = −4.00 | .000 | −0.790 |
| Clinical | |||||||||||
| Diagnosis, 10 years | |||||||||||
| Schizophrenia | 55 (38.7) | 55 (57.2) | - | ||||||||
| Schizophreniform | 1 (0.7) | 1 (1.0) | - | ||||||||
| Schizoaffective | 15 (10.6) | 15 (15.6) | - | ||||||||
| Other Psychosesa | 25 (17.6) | 25 (26.0) | - | ||||||||
| Bipolar 1 Disorder | 42 (29.6) | - | 42 (91.3) | ||||||||
| Bipolar 2 Disorder | 3 (2.1) | - | 3 (6.5) | ||||||||
| Bipolar NOS | 1 (0.7) | - | 1 (2.2) | ||||||||
| Psychotic ep. FUb | Mdn (ran) | 2 (0–40) | 2 (0–10) | 2 (0–40) | U = 1830.50 | .217 | |||||
| Manic ep. FUb | Mdn (ran) | 1 (0–42) | 1 (0–4) | 2 (0–42) | U = 333.00 | .020 | |||||
| Depressive ep. FUb | Mdn (ran) | 2 (0–48) | 2 (0–32) | 3 (0–48) | U = 1199.00 | .206 | |||||
| PANSSc | M (SD) | ||||||||||
| Positive | 7.4 (4.1) | 8.4 (4.4) | 5.4 (2.2) | t = 4.50 | .000 | .806 | |||||
| Negative | 9.4 (5.2) | 10.2 (5.9) | 7.8 (2.8) | t = 2.63 | .009 | .472 | |||||
| Disorganized | 4.2 (2.0) | 4.5 (2.3) | 3.6 (0.9) | t = 2.71 | .008 | .486 | |||||
| Excited | 4.7 (1.4) | 4.9 (1.6) | 4.5 (1.0) | t = 1.55 | .123 | .279 | |||||
| Depressive | 6.4 (3.3) | 6.5 (3.2) | 6.1 (3.5) | t = 0.59 | .559 | .105 | |||||
| CDSSd | M (SD) | 3.1 (4.4) | 3.1 (4.5) | 2.9 (4.1) | t = 0.21 | .835 | .039 | ||||
| YMRSe | M (SD) | 3.3 (4.0) | 3.9 (4.4) | 2.0 (2.7) | t = 2.62 | .010 | .475 | ||||
| GAF-Ff | M (SD) | 60.5 (17.7) | 59.4 (16.5) | 69.1 (17.2) | t = -4.24 | .000 | −0.761 | ||||
| AUDITg | Mdn (ran) | 3 (0–28) | 4 (0–28) | 3 (0–20) | U = 1646.50 | .626 | |||||
| DUDITh | Mdn (ran) | 0 (0–42) | 0 (0–42) | 0 (0–23) | U = 1421.50 | .034 | |||||
| Medicated, psychotropic | 95 (66.9) | 65 (69.1) | 30 (65.2) | χ2 = 0.22 | .701 | .040 |
Note: N (%) is reported unless otherwise specified, M (SD) = Mean (Standard Deviation), Mdn (ran) = Median (range).
Missing: Country of origin, 19; Relationship (healthy controls), 1; Medicated, psychotropic, 2.
a Delusional disorder = 5; brief psychotic disorder = 1; psychotic disorder not otherwise specified = 19.
b Episodes during follow-up period.
c PANSS, Positive and Negative Symptom Scale.
d CDSS, Calgary Depression Scale for Schizophrenia.
e YMRS, Young Mania Rating Scale.
f GAF-F, Global Assessment of Functioning—functioning subscale.
g AUDIT, Alcohol Use Disorders Identification Test.
h DUDIT, Drug Use Disorder Identification Test.
Demographic and Clinical Characteristics in Healthy Controls and Total Sample, and between Schizophrenia and Bipolar Spectrum Groups at 10-year Follow-up.
| . | . | Healthy Controls (n = 117) . | Total Sample (n = 142) . | Chi-square/t-test/Mann Whitney . | . | . | Schizophrenia Spectrum (n = 96) . | Bipolar Spectrum (n = 46) . | Chi-square/t-test/Mann Whitney . | . | . |
|---|---|---|---|---|---|---|---|---|---|---|---|
| . | . | . | . | χ2/t/U . | p . | V/D . | . | . | χ2/t/U . | p . | V/D . |
| Demographic | |||||||||||
| Gender, female | 49 (41.9) | 67 (47.2) | χ2 = 0.73 | .452 | .053 | 40 (41.7) | 27 (58.7) | χ2 = 3.62 | .073 | .160 | |
| Age | M (SD) | 40.3 (7.6) | 37.7 (8.3) | t = −2.61 | .010 | −0.325 | 36.9 (8.3) | 39.2 (8.2) | t = −1.56 | .121 | −0.280 |
| Country of origin | χ2 = 20.1 | .000 | .29 | χ2 = 0.00 | 1.000 | −0.006 | |||||
| Norway | 115 (98.3) | 98 (69.0) | 66 (79.5) | 32 (80.0) | |||||||
| Other | 2 (1.8) | 25 (17.6) | 17 (20.5) | 8 (20.0) | |||||||
| In relationship, current | 90 (76.9) | 65 (45.8) | χ2 = 25.90 | .000 | .316 | 39 (40.6) | 26 (56.5) | χ2 = 3.17 | .105 | .149 | |
| Education, years | M (SD) | 15.2 (2.3) | 13.6 (2.5) | t = −5.16 | .000 | −0.682 | 12.9 (2.5) | 14.8 (2.1) | t = −4.00 | .000 | −0.790 |
| Clinical | |||||||||||
| Diagnosis, 10 years | |||||||||||
| Schizophrenia | 55 (38.7) | 55 (57.2) | - | ||||||||
| Schizophreniform | 1 (0.7) | 1 (1.0) | - | ||||||||
| Schizoaffective | 15 (10.6) | 15 (15.6) | - | ||||||||
| Other Psychosesa | 25 (17.6) | 25 (26.0) | - | ||||||||
| Bipolar 1 Disorder | 42 (29.6) | - | 42 (91.3) | ||||||||
| Bipolar 2 Disorder | 3 (2.1) | - | 3 (6.5) | ||||||||
| Bipolar NOS | 1 (0.7) | - | 1 (2.2) | ||||||||
| Psychotic ep. FUb | Mdn (ran) | 2 (0–40) | 2 (0–10) | 2 (0–40) | U = 1830.50 | .217 | |||||
| Manic ep. FUb | Mdn (ran) | 1 (0–42) | 1 (0–4) | 2 (0–42) | U = 333.00 | .020 | |||||
| Depressive ep. FUb | Mdn (ran) | 2 (0–48) | 2 (0–32) | 3 (0–48) | U = 1199.00 | .206 | |||||
| PANSSc | M (SD) | ||||||||||
| Positive | 7.4 (4.1) | 8.4 (4.4) | 5.4 (2.2) | t = 4.50 | .000 | .806 | |||||
| Negative | 9.4 (5.2) | 10.2 (5.9) | 7.8 (2.8) | t = 2.63 | .009 | .472 | |||||
| Disorganized | 4.2 (2.0) | 4.5 (2.3) | 3.6 (0.9) | t = 2.71 | .008 | .486 | |||||
| Excited | 4.7 (1.4) | 4.9 (1.6) | 4.5 (1.0) | t = 1.55 | .123 | .279 | |||||
| Depressive | 6.4 (3.3) | 6.5 (3.2) | 6.1 (3.5) | t = 0.59 | .559 | .105 | |||||
| CDSSd | M (SD) | 3.1 (4.4) | 3.1 (4.5) | 2.9 (4.1) | t = 0.21 | .835 | .039 | ||||
| YMRSe | M (SD) | 3.3 (4.0) | 3.9 (4.4) | 2.0 (2.7) | t = 2.62 | .010 | .475 | ||||
| GAF-Ff | M (SD) | 60.5 (17.7) | 59.4 (16.5) | 69.1 (17.2) | t = -4.24 | .000 | −0.761 | ||||
| AUDITg | Mdn (ran) | 3 (0–28) | 4 (0–28) | 3 (0–20) | U = 1646.50 | .626 | |||||
| DUDITh | Mdn (ran) | 0 (0–42) | 0 (0–42) | 0 (0–23) | U = 1421.50 | .034 | |||||
| Medicated, psychotropic | 95 (66.9) | 65 (69.1) | 30 (65.2) | χ2 = 0.22 | .701 | .040 |
| . | . | Healthy Controls (n = 117) . | Total Sample (n = 142) . | Chi-square/t-test/Mann Whitney . | . | . | Schizophrenia Spectrum (n = 96) . | Bipolar Spectrum (n = 46) . | Chi-square/t-test/Mann Whitney . | . | . |
|---|---|---|---|---|---|---|---|---|---|---|---|
| . | . | . | . | χ2/t/U . | p . | V/D . | . | . | χ2/t/U . | p . | V/D . |
| Demographic | |||||||||||
| Gender, female | 49 (41.9) | 67 (47.2) | χ2 = 0.73 | .452 | .053 | 40 (41.7) | 27 (58.7) | χ2 = 3.62 | .073 | .160 | |
| Age | M (SD) | 40.3 (7.6) | 37.7 (8.3) | t = −2.61 | .010 | −0.325 | 36.9 (8.3) | 39.2 (8.2) | t = −1.56 | .121 | −0.280 |
| Country of origin | χ2 = 20.1 | .000 | .29 | χ2 = 0.00 | 1.000 | −0.006 | |||||
| Norway | 115 (98.3) | 98 (69.0) | 66 (79.5) | 32 (80.0) | |||||||
| Other | 2 (1.8) | 25 (17.6) | 17 (20.5) | 8 (20.0) | |||||||
| In relationship, current | 90 (76.9) | 65 (45.8) | χ2 = 25.90 | .000 | .316 | 39 (40.6) | 26 (56.5) | χ2 = 3.17 | .105 | .149 | |
| Education, years | M (SD) | 15.2 (2.3) | 13.6 (2.5) | t = −5.16 | .000 | −0.682 | 12.9 (2.5) | 14.8 (2.1) | t = −4.00 | .000 | −0.790 |
| Clinical | |||||||||||
| Diagnosis, 10 years | |||||||||||
| Schizophrenia | 55 (38.7) | 55 (57.2) | - | ||||||||
| Schizophreniform | 1 (0.7) | 1 (1.0) | - | ||||||||
| Schizoaffective | 15 (10.6) | 15 (15.6) | - | ||||||||
| Other Psychosesa | 25 (17.6) | 25 (26.0) | - | ||||||||
| Bipolar 1 Disorder | 42 (29.6) | - | 42 (91.3) | ||||||||
| Bipolar 2 Disorder | 3 (2.1) | - | 3 (6.5) | ||||||||
| Bipolar NOS | 1 (0.7) | - | 1 (2.2) | ||||||||
| Psychotic ep. FUb | Mdn (ran) | 2 (0–40) | 2 (0–10) | 2 (0–40) | U = 1830.50 | .217 | |||||
| Manic ep. FUb | Mdn (ran) | 1 (0–42) | 1 (0–4) | 2 (0–42) | U = 333.00 | .020 | |||||
| Depressive ep. FUb | Mdn (ran) | 2 (0–48) | 2 (0–32) | 3 (0–48) | U = 1199.00 | .206 | |||||
| PANSSc | M (SD) | ||||||||||
| Positive | 7.4 (4.1) | 8.4 (4.4) | 5.4 (2.2) | t = 4.50 | .000 | .806 | |||||
| Negative | 9.4 (5.2) | 10.2 (5.9) | 7.8 (2.8) | t = 2.63 | .009 | .472 | |||||
| Disorganized | 4.2 (2.0) | 4.5 (2.3) | 3.6 (0.9) | t = 2.71 | .008 | .486 | |||||
| Excited | 4.7 (1.4) | 4.9 (1.6) | 4.5 (1.0) | t = 1.55 | .123 | .279 | |||||
| Depressive | 6.4 (3.3) | 6.5 (3.2) | 6.1 (3.5) | t = 0.59 | .559 | .105 | |||||
| CDSSd | M (SD) | 3.1 (4.4) | 3.1 (4.5) | 2.9 (4.1) | t = 0.21 | .835 | .039 | ||||
| YMRSe | M (SD) | 3.3 (4.0) | 3.9 (4.4) | 2.0 (2.7) | t = 2.62 | .010 | .475 | ||||
| GAF-Ff | M (SD) | 60.5 (17.7) | 59.4 (16.5) | 69.1 (17.2) | t = -4.24 | .000 | −0.761 | ||||
| AUDITg | Mdn (ran) | 3 (0–28) | 4 (0–28) | 3 (0–20) | U = 1646.50 | .626 | |||||
| DUDITh | Mdn (ran) | 0 (0–42) | 0 (0–42) | 0 (0–23) | U = 1421.50 | .034 | |||||
| Medicated, psychotropic | 95 (66.9) | 65 (69.1) | 30 (65.2) | χ2 = 0.22 | .701 | .040 |
Note: N (%) is reported unless otherwise specified, M (SD) = Mean (Standard Deviation), Mdn (ran) = Median (range).
Missing: Country of origin, 19; Relationship (healthy controls), 1; Medicated, psychotropic, 2.
a Delusional disorder = 5; brief psychotic disorder = 1; psychotic disorder not otherwise specified = 19.
b Episodes during follow-up period.
c PANSS, Positive and Negative Symptom Scale.
d CDSS, Calgary Depression Scale for Schizophrenia.
e YMRS, Young Mania Rating Scale.
f GAF-F, Global Assessment of Functioning—functioning subscale.
g AUDIT, Alcohol Use Disorders Identification Test.
h DUDIT, Drug Use Disorder Identification Test.
The study was approved by the Regional Committee for Medical Research Ethics and the Norwegian Data Inspectorate. Data were obtained in compliance with the regulations of our institutions. All participants gave written informed consent to partake in the study. Study methodology was pre-registered in the Open Science Framework.
Assessment and Measures
Data on demographic and clinical factors were collected based on a comprehensive clinical interview combined with a review of medical charts. Participants were diagnosed with the Structural Clinical Interview for DSM-IV Axis I disorders (SCID-I) (First et al., 1995)26 at baseline and at follow-up. Psychosis was initially measured with the Positive and Negative Syndrome Scale (PANSS)27 with positive items P1, P3, P5, P6, and G9 equal to or above 4 as a cut-off. The Wallwork five-factor model consisting of a subset of PANSS items constituting positive, negative, disorganized, excited and depressive symptoms28 was used. This model has shown to be appropriate for FEP populations.29 Depressive symptoms were also measured with The Calgary Depression Scale for Schizophrenia (CDSS)30 and Inventory of Depressive Symptoms—Clinician rated (IDS-C).31 Young Mania Rating Scale (YMRS)32 was used to assess manic symptoms. Global functioning was measured with The Global Assessment of Functioning Scale (GAF), split version.33 Alcohol and drug use was measured with The Alcohol Use Disorder Identification Test/Drug Use Disorders Identification Test (AUDIT/DUDIT).34,35 Participants were assessed and diagnosed by licensed clinical psychologists or physicians under weekly supervision by experienced consultant clinical psychologists and psychiatrists. Assessments were discussed until agreement by consensus ratings in weekly meetings with senior clinical scientists and project group members.
The standard clinical recovery definition used in this study required: a duration of 12 months meeting the below criteria for psychotic symptomatic remission11 and adequate functioning.17
Psychotic symptomatic remission was defined according to the RSWG international consensus definition11 with scores equal to or below 3 on the following PANSS items at time of follow-up: positive symptoms (P1-delusions, G9-unusual thought content, P3-hallucinations), disorganized symptoms (P2-conceptual disorganization, G5-mannerisms/posturing), and negative symptoms (N1-blunted affect, N4-social withdrawal, N6-lack of spontaneity). Assessment was based on instruments (SCID-I, PANSS, CDSS), a participant report, and chart review. Discontinuation of medication is not a requirement of symptomatic remission in the consensus definition.11
Affective symptomatic remission was defined as an IDS-C score below 14, CDSS-score below 7 and YMRS-score below 8, as well as not meeting criteria for a current affective episode according to SCID-1 at follow-up.
Adequate functioning was defined in accordance with the TIPS 10-year follow-up17 by the presence of full-time occupational functioning in terms of work, study or other (such as full-time child rearing), social functioning (comparable to meeting a friend in person at least once weekly), and independent living (reside in unsupervised home and maintaining activities of daily living (ADL)).
Altering clinical recovery criteria involved: (1) Shortening or extending the required duration of the period in recovery, to no duration, 6 months, 24 months and 60 months. (2) The inclusion of affective symptom remission in addition to psychotic symptom remission. (3) Loosening the standard adequate functioning criteria by allowing part-time (≥40%) instead of full-time occupational functioning, and by having a close friend/confidant instead of the requirement to meet a friend once weekly for social functioning.
Healthy Controls
Healthy control participants matched in age and gender were randomly selected from the same catchment area. They were screened at baseline and 10-year follow-up with an interview on severe mental illness symptoms and the Primary Care Evaluation of Mental Disorders (PRIME-MD) (Spitzer et al., 1999). They underwent a brief demographic interview and completed self-report measures including level of functioning. Controls were assessed by personnel trained and supervised in cognitive and functioning assessments by a senior clinical researcher. Healthy controls were excluded according to exclusion criteria for participants, if they had experienced substance abuse or dependency in the last 6 months, or if they or any of their close relatives, had a lifetime history of severe psychiatric disorder at baseline. Among the 179 healthy controls assessed at baseline and eligible for follow-up, 120 controls were retained at 10-year follow-up. Three were excluded in the present study due to missing data, leaving 117 participants.
Statistical Analyses
Analyses were completed with IBM SPSS Statistics version 26. The first aim was investigated with descriptive statistics for rate in clinical recovery according to the standard definition. The differences in demographic and clinical characteristics between the healthy controls and total sample, between schizophrenia and bipolar spectrum diagnostic groups, as well as between the groups not in clinical recovery and in recovery, were all investigated with chi-square for categorical independent variables, t-test for continuous independent variables and Mann Whitney U tests for nonnormally distributed continuous variables. Descriptive statistics were also used to calculate the clinical recovery rates with altered criteria. Finally, rate of adequate functioning according to the standard definition in healthy controls was calculated. All tests were two-tailed, with the level of significance set to .05.
Results
Background Characteristics
There were no baseline demographic or clinical differences between participants that completed 10-year follow-up and those that were lost to 10-year follow-up, apart from significantly more men (63.6% vs. 52.7%) (χ 2 (1, N = 444) = 5.229 P < .05) and schizophrenia spectrum participants (66.6% vs. 60.9%) (χ 2 (1, N = 444) = 9.110 P < .05) in the group lost to follow-up.
Background demographic and clinical characteristics for the healthy controls, total sample and schizophrenia and bipolar spectrum groups are presented in Table 1. Significantly more healthy controls were ethnic Norwegians or in a relationship, and they had a higher level of education compared to the total sample. When comparing the two diagnostic groups, the only significant demographic difference was more years of education in the bipolar spectrum group. The significant clinical differences were in line with the diagnostic criteria; with the schizophrenia spectrum group having higher scores for PANSS positive, negative and disorganized symptom scores; moreover, higher YMRS and DUDIT. While the bipolar spectrum group had significantly more manic episodes and better GAF-F scores.
Standard Clinical Recovery Criteria
Presented in Table 2, in the total sample 31.7% were in clinical recovery at 10-year follow-up according to the standard definition. Moreover, 59.9% met criteria for psychotic symptom remission of at least 12 months duration, while 32.4% met the criteria for adequate functioning, mainly because few participants had full-time occupation. The clinical recovery rate was significantly higher among participants with bipolar spectrum diagnosis (50.0%) compared to schizophrenia spectrum diagnosis (22.9%). Within the schizophrenia and bipolar spectrums, the recovery rate varied across diagnostic subgroups with n > 10 (Schizophrenia 10.9%, Schizoaffective disorder 33.3%, Other psychosis 40.0%, Bipolar I 50.0%). Both psychotic symptom remission and adequate functioning was higher in the bipolar than the schizophrenia spectrum group. Social functioning was the only subcriterion that was not significantly higher in the bipolar than the schizophrenia spectrum group.
Clinical Recovery Rates in Healthy Controls and Total Sample, and Between Schizophrenia and Bipolar Spectrum Groups at 10-year Follow-up
| . | Healthy Controls (n = 117) . | Total Sample (n = 142) . | Chi-square/t-test/Mann Whitney . | . | . | Schizophrenia Spectrum (n = 96) . | Bipolar Spectrum (n = 46) . | Chi-square/t-test/Mann Whitney . | . | . |
|---|---|---|---|---|---|---|---|---|---|---|
| . | . | . | χ2/t/U . | p . | V/D . | . | . | χ2/t/U . | p . | V/D . |
| Standard Clinical Recovery Criteria | ||||||||||
| Clinical Recoverya | 45 (31.7) | 22 (22.9) | 23 (50.0) | χ2 = 10.54 | .002 | .272 | ||||
| Psychotic Remissionb | 85 (59.9) | 44 (51.8) | 41 (89.1) | χ2 = 24.26 | .000 | .413 | ||||
| Adequate Functioningc | 95 (81.2) | 46 (32.4) | χ2 = 61.60 | .000 | .488 | 23 (24.0) | 23 (50.0) | χ2 = 9.63 | .004 | .260 |
| Independent Living | 117 (100.0) | 111 (78.2) | χ2 = 29.02 | .000 | .335 | 69 (71.9) | 42 (91.3) | χ2 = 6.88 | .009 | .220 |
| Social Functioning | 101 (86.3) | 79 (55.6) | χ2 = 28.10 | .000 | .330 | 49 (51.0) | 30 (65.2) | χ2 = 2.53 | .149 | .134 |
| Full-time Occupationd (work/study/other) | 111 (94.9) | 48 (33.8) | χ2 = 100.93 | .000 | .624 | 25 (26.0) | 23 (50.0) | χ2 = 7.98 | .008 | .237 |
| Altering Clinical Recovery Criteria | ||||||||||
| Duration | ||||||||||
| Duratione, Present/No Duration | 52 (36.6) | 25 (26.0) | 27 (58.7) | χ2 = 14.29 | .000 | .317 | ||||
| Duratione, 6 months | 50 (35.2) | 24 (25.0) | 26 (56.5) | χ2 = 13.55 | .000 | .309 | ||||
| Duratione, 24 months | 38 (26.8) | 18 (18.8) | 20 (43.5) | χ2 = 9.70 | .003 | .261 | ||||
| Duratione, 60 months | 25 (17.6) | 13 (13.5) | 12 (26.1) | χ2 = 3.37 | .098 | .154 | ||||
| Symptom Remission | ||||||||||
| Psychotic + Affective Remissionf | 38 (26.8) | 17 (17.9) | 21 (45.7) | χ2 = 12.13 | .001 | .293 | ||||
| Affective Remissiong | 83 (58.5) | 56 (58.9) | 27 (58.7) | χ2 = 0.00 | 1.000 | .002 | ||||
| Adequate Functioning | ||||||||||
| Social functioning—Close friendh | 110 (94.0) | 46 (32.4) | χ2 = 101.70 | .000 | .627 | 23 (24.0) | 23 (50.0) | χ2 = 9.63 | .004 | .260 |
| Part-time Occupationi | 97 (82.9) | 52 (36.6) | χ2 = 57.81 | .000 | .473 | 25 (26.0) | 27 (58.7) | χ2 = 14.29 | .000 | .317 |
| Part-time Occupation + Close friendj | 112 (95.7) | 58 (40.8) | χ2 = 85.66 | .000 | .575 | 27(28.1) | 31 (67.4) | χ2 = 19.85 | .000 | .374 |
| Partial function + Affective Remissionk | 45 (31.7) | 21 (21.9) | 24 (52.2) | χ2 = 13.19 | .000 | .305 |
| . | Healthy Controls (n = 117) . | Total Sample (n = 142) . | Chi-square/t-test/Mann Whitney . | . | . | Schizophrenia Spectrum (n = 96) . | Bipolar Spectrum (n = 46) . | Chi-square/t-test/Mann Whitney . | . | . |
|---|---|---|---|---|---|---|---|---|---|---|
| . | . | . | χ2/t/U . | p . | V/D . | . | . | χ2/t/U . | p . | V/D . |
| Standard Clinical Recovery Criteria | ||||||||||
| Clinical Recoverya | 45 (31.7) | 22 (22.9) | 23 (50.0) | χ2 = 10.54 | .002 | .272 | ||||
| Psychotic Remissionb | 85 (59.9) | 44 (51.8) | 41 (89.1) | χ2 = 24.26 | .000 | .413 | ||||
| Adequate Functioningc | 95 (81.2) | 46 (32.4) | χ2 = 61.60 | .000 | .488 | 23 (24.0) | 23 (50.0) | χ2 = 9.63 | .004 | .260 |
| Independent Living | 117 (100.0) | 111 (78.2) | χ2 = 29.02 | .000 | .335 | 69 (71.9) | 42 (91.3) | χ2 = 6.88 | .009 | .220 |
| Social Functioning | 101 (86.3) | 79 (55.6) | χ2 = 28.10 | .000 | .330 | 49 (51.0) | 30 (65.2) | χ2 = 2.53 | .149 | .134 |
| Full-time Occupationd (work/study/other) | 111 (94.9) | 48 (33.8) | χ2 = 100.93 | .000 | .624 | 25 (26.0) | 23 (50.0) | χ2 = 7.98 | .008 | .237 |
| Altering Clinical Recovery Criteria | ||||||||||
| Duration | ||||||||||
| Duratione, Present/No Duration | 52 (36.6) | 25 (26.0) | 27 (58.7) | χ2 = 14.29 | .000 | .317 | ||||
| Duratione, 6 months | 50 (35.2) | 24 (25.0) | 26 (56.5) | χ2 = 13.55 | .000 | .309 | ||||
| Duratione, 24 months | 38 (26.8) | 18 (18.8) | 20 (43.5) | χ2 = 9.70 | .003 | .261 | ||||
| Duratione, 60 months | 25 (17.6) | 13 (13.5) | 12 (26.1) | χ2 = 3.37 | .098 | .154 | ||||
| Symptom Remission | ||||||||||
| Psychotic + Affective Remissionf | 38 (26.8) | 17 (17.9) | 21 (45.7) | χ2 = 12.13 | .001 | .293 | ||||
| Affective Remissiong | 83 (58.5) | 56 (58.9) | 27 (58.7) | χ2 = 0.00 | 1.000 | .002 | ||||
| Adequate Functioning | ||||||||||
| Social functioning—Close friendh | 110 (94.0) | 46 (32.4) | χ2 = 101.70 | .000 | .627 | 23 (24.0) | 23 (50.0) | χ2 = 9.63 | .004 | .260 |
| Part-time Occupationi | 97 (82.9) | 52 (36.6) | χ2 = 57.81 | .000 | .473 | 25 (26.0) | 27 (58.7) | χ2 = 14.29 | .000 | .317 |
| Part-time Occupation + Close friendj | 112 (95.7) | 58 (40.8) | χ2 = 85.66 | .000 | .575 | 27(28.1) | 31 (67.4) | χ2 = 19.85 | .000 | .374 |
| Partial function + Affective Remissionk | 45 (31.7) | 21 (21.9) | 24 (52.2) | χ2 = 13.19 | .000 | .305 |
Note: N (%) is reported for all. Missing: Social Functioning total sample = 1; Affective remission = 1.
aStandard clinical recovery definition: Psychotic symptom remission and adequate functioning, 12 months duration
bRGSW consensus criteria (Andreasen et al., 2005): 12 months duration.
cAdequate functioning: 12 months duration.
dOccupation: work/study/other.
eDuration: required period of psychotic remission and adequate functioning (original criteria)
f Standard recovery criteria with adding affective remission (IDS-C (Inventory of Depressive Symptoms-Clinician Rated) < 14/CDSS < 7/YMRS < 8, no current episode).
gAffective remission (IDS-C (Inventory of Depressive Symptoms-Clinician Rated) < 14/CDSS < 7/YMRS < 8, no current episode) with 12 months duration.
h Standard recovery criteria with altered social functioning criteria to having a close friend/confidant from meeting friend once weekly. For controls, functioning criteria only.
i Standard recovery criteria with altered occupation to part-time instead of full-time.
j Including both part-time occupation and Social functioning-close friend/confidant (h and i).
k Standard recovery criteria and adding both Part-time occupation + Social functioning-close friend (partial function) and affective symptom remission.
Clinical Recovery Rates in Healthy Controls and Total Sample, and Between Schizophrenia and Bipolar Spectrum Groups at 10-year Follow-up
| . | Healthy Controls (n = 117) . | Total Sample (n = 142) . | Chi-square/t-test/Mann Whitney . | . | . | Schizophrenia Spectrum (n = 96) . | Bipolar Spectrum (n = 46) . | Chi-square/t-test/Mann Whitney . | . | . |
|---|---|---|---|---|---|---|---|---|---|---|
| . | . | . | χ2/t/U . | p . | V/D . | . | . | χ2/t/U . | p . | V/D . |
| Standard Clinical Recovery Criteria | ||||||||||
| Clinical Recoverya | 45 (31.7) | 22 (22.9) | 23 (50.0) | χ2 = 10.54 | .002 | .272 | ||||
| Psychotic Remissionb | 85 (59.9) | 44 (51.8) | 41 (89.1) | χ2 = 24.26 | .000 | .413 | ||||
| Adequate Functioningc | 95 (81.2) | 46 (32.4) | χ2 = 61.60 | .000 | .488 | 23 (24.0) | 23 (50.0) | χ2 = 9.63 | .004 | .260 |
| Independent Living | 117 (100.0) | 111 (78.2) | χ2 = 29.02 | .000 | .335 | 69 (71.9) | 42 (91.3) | χ2 = 6.88 | .009 | .220 |
| Social Functioning | 101 (86.3) | 79 (55.6) | χ2 = 28.10 | .000 | .330 | 49 (51.0) | 30 (65.2) | χ2 = 2.53 | .149 | .134 |
| Full-time Occupationd (work/study/other) | 111 (94.9) | 48 (33.8) | χ2 = 100.93 | .000 | .624 | 25 (26.0) | 23 (50.0) | χ2 = 7.98 | .008 | .237 |
| Altering Clinical Recovery Criteria | ||||||||||
| Duration | ||||||||||
| Duratione, Present/No Duration | 52 (36.6) | 25 (26.0) | 27 (58.7) | χ2 = 14.29 | .000 | .317 | ||||
| Duratione, 6 months | 50 (35.2) | 24 (25.0) | 26 (56.5) | χ2 = 13.55 | .000 | .309 | ||||
| Duratione, 24 months | 38 (26.8) | 18 (18.8) | 20 (43.5) | χ2 = 9.70 | .003 | .261 | ||||
| Duratione, 60 months | 25 (17.6) | 13 (13.5) | 12 (26.1) | χ2 = 3.37 | .098 | .154 | ||||
| Symptom Remission | ||||||||||
| Psychotic + Affective Remissionf | 38 (26.8) | 17 (17.9) | 21 (45.7) | χ2 = 12.13 | .001 | .293 | ||||
| Affective Remissiong | 83 (58.5) | 56 (58.9) | 27 (58.7) | χ2 = 0.00 | 1.000 | .002 | ||||
| Adequate Functioning | ||||||||||
| Social functioning—Close friendh | 110 (94.0) | 46 (32.4) | χ2 = 101.70 | .000 | .627 | 23 (24.0) | 23 (50.0) | χ2 = 9.63 | .004 | .260 |
| Part-time Occupationi | 97 (82.9) | 52 (36.6) | χ2 = 57.81 | .000 | .473 | 25 (26.0) | 27 (58.7) | χ2 = 14.29 | .000 | .317 |
| Part-time Occupation + Close friendj | 112 (95.7) | 58 (40.8) | χ2 = 85.66 | .000 | .575 | 27(28.1) | 31 (67.4) | χ2 = 19.85 | .000 | .374 |
| Partial function + Affective Remissionk | 45 (31.7) | 21 (21.9) | 24 (52.2) | χ2 = 13.19 | .000 | .305 |
| . | Healthy Controls (n = 117) . | Total Sample (n = 142) . | Chi-square/t-test/Mann Whitney . | . | . | Schizophrenia Spectrum (n = 96) . | Bipolar Spectrum (n = 46) . | Chi-square/t-test/Mann Whitney . | . | . |
|---|---|---|---|---|---|---|---|---|---|---|
| . | . | . | χ2/t/U . | p . | V/D . | . | . | χ2/t/U . | p . | V/D . |
| Standard Clinical Recovery Criteria | ||||||||||
| Clinical Recoverya | 45 (31.7) | 22 (22.9) | 23 (50.0) | χ2 = 10.54 | .002 | .272 | ||||
| Psychotic Remissionb | 85 (59.9) | 44 (51.8) | 41 (89.1) | χ2 = 24.26 | .000 | .413 | ||||
| Adequate Functioningc | 95 (81.2) | 46 (32.4) | χ2 = 61.60 | .000 | .488 | 23 (24.0) | 23 (50.0) | χ2 = 9.63 | .004 | .260 |
| Independent Living | 117 (100.0) | 111 (78.2) | χ2 = 29.02 | .000 | .335 | 69 (71.9) | 42 (91.3) | χ2 = 6.88 | .009 | .220 |
| Social Functioning | 101 (86.3) | 79 (55.6) | χ2 = 28.10 | .000 | .330 | 49 (51.0) | 30 (65.2) | χ2 = 2.53 | .149 | .134 |
| Full-time Occupationd (work/study/other) | 111 (94.9) | 48 (33.8) | χ2 = 100.93 | .000 | .624 | 25 (26.0) | 23 (50.0) | χ2 = 7.98 | .008 | .237 |
| Altering Clinical Recovery Criteria | ||||||||||
| Duration | ||||||||||
| Duratione, Present/No Duration | 52 (36.6) | 25 (26.0) | 27 (58.7) | χ2 = 14.29 | .000 | .317 | ||||
| Duratione, 6 months | 50 (35.2) | 24 (25.0) | 26 (56.5) | χ2 = 13.55 | .000 | .309 | ||||
| Duratione, 24 months | 38 (26.8) | 18 (18.8) | 20 (43.5) | χ2 = 9.70 | .003 | .261 | ||||
| Duratione, 60 months | 25 (17.6) | 13 (13.5) | 12 (26.1) | χ2 = 3.37 | .098 | .154 | ||||
| Symptom Remission | ||||||||||
| Psychotic + Affective Remissionf | 38 (26.8) | 17 (17.9) | 21 (45.7) | χ2 = 12.13 | .001 | .293 | ||||
| Affective Remissiong | 83 (58.5) | 56 (58.9) | 27 (58.7) | χ2 = 0.00 | 1.000 | .002 | ||||
| Adequate Functioning | ||||||||||
| Social functioning—Close friendh | 110 (94.0) | 46 (32.4) | χ2 = 101.70 | .000 | .627 | 23 (24.0) | 23 (50.0) | χ2 = 9.63 | .004 | .260 |
| Part-time Occupationi | 97 (82.9) | 52 (36.6) | χ2 = 57.81 | .000 | .473 | 25 (26.0) | 27 (58.7) | χ2 = 14.29 | .000 | .317 |
| Part-time Occupation + Close friendj | 112 (95.7) | 58 (40.8) | χ2 = 85.66 | .000 | .575 | 27(28.1) | 31 (67.4) | χ2 = 19.85 | .000 | .374 |
| Partial function + Affective Remissionk | 45 (31.7) | 21 (21.9) | 24 (52.2) | χ2 = 13.19 | .000 | .305 |
Note: N (%) is reported for all. Missing: Social Functioning total sample = 1; Affective remission = 1.
aStandard clinical recovery definition: Psychotic symptom remission and adequate functioning, 12 months duration
bRGSW consensus criteria (Andreasen et al., 2005): 12 months duration.
cAdequate functioning: 12 months duration.
dOccupation: work/study/other.
eDuration: required period of psychotic remission and adequate functioning (original criteria)
f Standard recovery criteria with adding affective remission (IDS-C (Inventory of Depressive Symptoms-Clinician Rated) < 14/CDSS < 7/YMRS < 8, no current episode).
gAffective remission (IDS-C (Inventory of Depressive Symptoms-Clinician Rated) < 14/CDSS < 7/YMRS < 8, no current episode) with 12 months duration.
h Standard recovery criteria with altered social functioning criteria to having a close friend/confidant from meeting friend once weekly. For controls, functioning criteria only.
i Standard recovery criteria with altered occupation to part-time instead of full-time.
j Including both part-time occupation and Social functioning-close friend/confidant (h and i).
k Standard recovery criteria and adding both Part-time occupation + Social functioning-close friend (partial function) and affective symptom remission.
Illustrated in Table 3, the only demographic difference was more years of education in the recovery group than nonrecovery group. The significant clinical differences were in line with the standard clinical recovery definition, with the recovery group having lower psychotic symptom scores and higher functioning, as well as lower affective symptom scores. There were no differences in number of psychotic/affective episodes during follow-up.
Demographic and Clinical Characteristics Between Participants in Clinical Recovery* and not in Clinical Recovery at 10-year Follow-up
| . | . | Nonrecovery (n = 97) . | Recovery (n = 45) . | Chi-square/t-test/ Mann Whitney . | . | . |
|---|---|---|---|---|---|---|
| χ2/t/U | p | V/D | ||||
| Demographic | ||||||
| Gender, female | 42 (43.3) | 25 (55.6) | χ2 = 1.85 | .207 | .114 | |
| Age | M (SD) | 38.3 (8.2) | 36.3 (8.4) | t = 1.32 | .191 | .237 |
| Country of origin | χ2 = 0.12 | .812 | .032 | |||
| Norwegian | 67 (78.8) | 31 (81.6) | ||||
| Other | 18 (21.2) | 7 (18.4) | ||||
| Education, years | M (SD) | 12.8 (2.3) | 15.1 (2.2) | t = −5.10 | .000 | −1.007 |
| Clinical | ||||||
| Diagnosis, 10 years | ||||||
| Schizophrenia spectrum | 74 (76.3) | 22 (48.9) | ||||
| Schizophrenia | 49 | 6 | ||||
| Schizophreniform | 0 | 1 | ||||
| Schizoaffective | 10 | 5 | ||||
| ”Other Psychoses”a | 15 | 10 | ||||
| Bipolar spectrum | 23 (23.7) | 23 (51.1) | ||||
| Bipolar 1 Disorder | 21 | 21 | ||||
| Bipolar 2 Disorder | 1 | 2 | ||||
| Bipolar NOS | 1 | 0 | ||||
| Psychotic ep. FUb | Mdn (ran) | 2 (1–40) | 2 (0–7) | U = 1913.50 | .401 | |
| Manic ep. FUb | Mdn (ran) | 1 (0–42) | 2 (0–9) | U = 487.50 | .726 | |
| Depressive ep. FUb | Mdn (ran) | 2 (0–48) | 2 (0–38) | U = 1133.00 | .198 | |
| PANSSc | M (SD) | |||||
| Positive | 8.7 (4.3) | 4.6 (1.1) | t = 6.25 | .000 | 1.13 | |
| Negative | 10.6 (5.8) | 6.9 (1.7) | t = 4.20 | .000 | .758 | |
| Disorganized | 4.7 (2.3) | 3.3 (0.5) | t = 4.01 | .000 | .723 | |
| Excited | 4.9 (1.6) | 4.3 (0.8) | t = 2.52 | .013 | .454 | |
| Depressive | 7.2 (3.5) | 4.4 (1.9) | t = 5.12 | .000 | .923 | |
| CDSSd | M (SD) | 4.1 (4.9) | .8 (1.6) | t = 4.29 | .000 | .796 |
| YMRSe | M (SD) | 4.4 (4.4) | 1.0 (1.6) | t = 4.98 | .000 | .910 |
| GAF-Ff | M (SD) | 51.1 (12.7) | 80.7 (6.5) | t = -14.70 | .000 | -2.65 |
| AUDITg | Mdn (ran) | 4 (0–28) | 3 (0–20) | U = 1664.00 | .785 | |
| DUDITh | Mdn (ran) | 0 (0–42) | 0 (0–23) | U = 1643.00 | .624 | |
| Medicated, psychotropic | 64 (67.4) | 31 (68.9) | χ2 = 0.03 | 1.000 | .015 |
| . | . | Nonrecovery (n = 97) . | Recovery (n = 45) . | Chi-square/t-test/ Mann Whitney . | . | . |
|---|---|---|---|---|---|---|
| χ2/t/U | p | V/D | ||||
| Demographic | ||||||
| Gender, female | 42 (43.3) | 25 (55.6) | χ2 = 1.85 | .207 | .114 | |
| Age | M (SD) | 38.3 (8.2) | 36.3 (8.4) | t = 1.32 | .191 | .237 |
| Country of origin | χ2 = 0.12 | .812 | .032 | |||
| Norwegian | 67 (78.8) | 31 (81.6) | ||||
| Other | 18 (21.2) | 7 (18.4) | ||||
| Education, years | M (SD) | 12.8 (2.3) | 15.1 (2.2) | t = −5.10 | .000 | −1.007 |
| Clinical | ||||||
| Diagnosis, 10 years | ||||||
| Schizophrenia spectrum | 74 (76.3) | 22 (48.9) | ||||
| Schizophrenia | 49 | 6 | ||||
| Schizophreniform | 0 | 1 | ||||
| Schizoaffective | 10 | 5 | ||||
| ”Other Psychoses”a | 15 | 10 | ||||
| Bipolar spectrum | 23 (23.7) | 23 (51.1) | ||||
| Bipolar 1 Disorder | 21 | 21 | ||||
| Bipolar 2 Disorder | 1 | 2 | ||||
| Bipolar NOS | 1 | 0 | ||||
| Psychotic ep. FUb | Mdn (ran) | 2 (1–40) | 2 (0–7) | U = 1913.50 | .401 | |
| Manic ep. FUb | Mdn (ran) | 1 (0–42) | 2 (0–9) | U = 487.50 | .726 | |
| Depressive ep. FUb | Mdn (ran) | 2 (0–48) | 2 (0–38) | U = 1133.00 | .198 | |
| PANSSc | M (SD) | |||||
| Positive | 8.7 (4.3) | 4.6 (1.1) | t = 6.25 | .000 | 1.13 | |
| Negative | 10.6 (5.8) | 6.9 (1.7) | t = 4.20 | .000 | .758 | |
| Disorganized | 4.7 (2.3) | 3.3 (0.5) | t = 4.01 | .000 | .723 | |
| Excited | 4.9 (1.6) | 4.3 (0.8) | t = 2.52 | .013 | .454 | |
| Depressive | 7.2 (3.5) | 4.4 (1.9) | t = 5.12 | .000 | .923 | |
| CDSSd | M (SD) | 4.1 (4.9) | .8 (1.6) | t = 4.29 | .000 | .796 |
| YMRSe | M (SD) | 4.4 (4.4) | 1.0 (1.6) | t = 4.98 | .000 | .910 |
| GAF-Ff | M (SD) | 51.1 (12.7) | 80.7 (6.5) | t = -14.70 | .000 | -2.65 |
| AUDITg | Mdn (ran) | 4 (0–28) | 3 (0–20) | U = 1664.00 | .785 | |
| DUDITh | Mdn (ran) | 0 (0–42) | 0 (0–23) | U = 1643.00 | .624 | |
| Medicated, psychotropic | 64 (67.4) | 31 (68.9) | χ2 = 0.03 | 1.000 | .015 |
Note: N (%) is reported unless otherwise specified, M (SD) = Mean (Standard Deviation), Mdn (ran) = Median (range).
* Standard clinical recovery definition: Psychotic symptom remission and adequate functioning, 12 months duration.
a Delusional disorder = 5; brief psychotic disorder = 1; psychotic disorder not otherwise specified = 19.
b Episodes during follow-up period.
c PANSS, Positive and Negative Symptom Scale.
d CDSS, Calgary Depression Scale for Schizophrenia.
e YMRS, Young Mania Rating Scale.
f GAF-F, Global Assessment of Functioning—functioning subscale.
g AUDIT, Alcohol Use Disorders Identification Test.
h DUDIT, Drug Use Disorder Identification Test.
Demographic and Clinical Characteristics Between Participants in Clinical Recovery* and not in Clinical Recovery at 10-year Follow-up
| . | . | Nonrecovery (n = 97) . | Recovery (n = 45) . | Chi-square/t-test/ Mann Whitney . | . | . |
|---|---|---|---|---|---|---|
| χ2/t/U | p | V/D | ||||
| Demographic | ||||||
| Gender, female | 42 (43.3) | 25 (55.6) | χ2 = 1.85 | .207 | .114 | |
| Age | M (SD) | 38.3 (8.2) | 36.3 (8.4) | t = 1.32 | .191 | .237 |
| Country of origin | χ2 = 0.12 | .812 | .032 | |||
| Norwegian | 67 (78.8) | 31 (81.6) | ||||
| Other | 18 (21.2) | 7 (18.4) | ||||
| Education, years | M (SD) | 12.8 (2.3) | 15.1 (2.2) | t = −5.10 | .000 | −1.007 |
| Clinical | ||||||
| Diagnosis, 10 years | ||||||
| Schizophrenia spectrum | 74 (76.3) | 22 (48.9) | ||||
| Schizophrenia | 49 | 6 | ||||
| Schizophreniform | 0 | 1 | ||||
| Schizoaffective | 10 | 5 | ||||
| ”Other Psychoses”a | 15 | 10 | ||||
| Bipolar spectrum | 23 (23.7) | 23 (51.1) | ||||
| Bipolar 1 Disorder | 21 | 21 | ||||
| Bipolar 2 Disorder | 1 | 2 | ||||
| Bipolar NOS | 1 | 0 | ||||
| Psychotic ep. FUb | Mdn (ran) | 2 (1–40) | 2 (0–7) | U = 1913.50 | .401 | |
| Manic ep. FUb | Mdn (ran) | 1 (0–42) | 2 (0–9) | U = 487.50 | .726 | |
| Depressive ep. FUb | Mdn (ran) | 2 (0–48) | 2 (0–38) | U = 1133.00 | .198 | |
| PANSSc | M (SD) | |||||
| Positive | 8.7 (4.3) | 4.6 (1.1) | t = 6.25 | .000 | 1.13 | |
| Negative | 10.6 (5.8) | 6.9 (1.7) | t = 4.20 | .000 | .758 | |
| Disorganized | 4.7 (2.3) | 3.3 (0.5) | t = 4.01 | .000 | .723 | |
| Excited | 4.9 (1.6) | 4.3 (0.8) | t = 2.52 | .013 | .454 | |
| Depressive | 7.2 (3.5) | 4.4 (1.9) | t = 5.12 | .000 | .923 | |
| CDSSd | M (SD) | 4.1 (4.9) | .8 (1.6) | t = 4.29 | .000 | .796 |
| YMRSe | M (SD) | 4.4 (4.4) | 1.0 (1.6) | t = 4.98 | .000 | .910 |
| GAF-Ff | M (SD) | 51.1 (12.7) | 80.7 (6.5) | t = -14.70 | .000 | -2.65 |
| AUDITg | Mdn (ran) | 4 (0–28) | 3 (0–20) | U = 1664.00 | .785 | |
| DUDITh | Mdn (ran) | 0 (0–42) | 0 (0–23) | U = 1643.00 | .624 | |
| Medicated, psychotropic | 64 (67.4) | 31 (68.9) | χ2 = 0.03 | 1.000 | .015 |
| . | . | Nonrecovery (n = 97) . | Recovery (n = 45) . | Chi-square/t-test/ Mann Whitney . | . | . |
|---|---|---|---|---|---|---|
| χ2/t/U | p | V/D | ||||
| Demographic | ||||||
| Gender, female | 42 (43.3) | 25 (55.6) | χ2 = 1.85 | .207 | .114 | |
| Age | M (SD) | 38.3 (8.2) | 36.3 (8.4) | t = 1.32 | .191 | .237 |
| Country of origin | χ2 = 0.12 | .812 | .032 | |||
| Norwegian | 67 (78.8) | 31 (81.6) | ||||
| Other | 18 (21.2) | 7 (18.4) | ||||
| Education, years | M (SD) | 12.8 (2.3) | 15.1 (2.2) | t = −5.10 | .000 | −1.007 |
| Clinical | ||||||
| Diagnosis, 10 years | ||||||
| Schizophrenia spectrum | 74 (76.3) | 22 (48.9) | ||||
| Schizophrenia | 49 | 6 | ||||
| Schizophreniform | 0 | 1 | ||||
| Schizoaffective | 10 | 5 | ||||
| ”Other Psychoses”a | 15 | 10 | ||||
| Bipolar spectrum | 23 (23.7) | 23 (51.1) | ||||
| Bipolar 1 Disorder | 21 | 21 | ||||
| Bipolar 2 Disorder | 1 | 2 | ||||
| Bipolar NOS | 1 | 0 | ||||
| Psychotic ep. FUb | Mdn (ran) | 2 (1–40) | 2 (0–7) | U = 1913.50 | .401 | |
| Manic ep. FUb | Mdn (ran) | 1 (0–42) | 2 (0–9) | U = 487.50 | .726 | |
| Depressive ep. FUb | Mdn (ran) | 2 (0–48) | 2 (0–38) | U = 1133.00 | .198 | |
| PANSSc | M (SD) | |||||
| Positive | 8.7 (4.3) | 4.6 (1.1) | t = 6.25 | .000 | 1.13 | |
| Negative | 10.6 (5.8) | 6.9 (1.7) | t = 4.20 | .000 | .758 | |
| Disorganized | 4.7 (2.3) | 3.3 (0.5) | t = 4.01 | .000 | .723 | |
| Excited | 4.9 (1.6) | 4.3 (0.8) | t = 2.52 | .013 | .454 | |
| Depressive | 7.2 (3.5) | 4.4 (1.9) | t = 5.12 | .000 | .923 | |
| CDSSd | M (SD) | 4.1 (4.9) | .8 (1.6) | t = 4.29 | .000 | .796 |
| YMRSe | M (SD) | 4.4 (4.4) | 1.0 (1.6) | t = 4.98 | .000 | .910 |
| GAF-Ff | M (SD) | 51.1 (12.7) | 80.7 (6.5) | t = -14.70 | .000 | -2.65 |
| AUDITg | Mdn (ran) | 4 (0–28) | 3 (0–20) | U = 1664.00 | .785 | |
| DUDITh | Mdn (ran) | 0 (0–42) | 0 (0–23) | U = 1643.00 | .624 | |
| Medicated, psychotropic | 64 (67.4) | 31 (68.9) | χ2 = 0.03 | 1.000 | .015 |
Note: N (%) is reported unless otherwise specified, M (SD) = Mean (Standard Deviation), Mdn (ran) = Median (range).
* Standard clinical recovery definition: Psychotic symptom remission and adequate functioning, 12 months duration.
a Delusional disorder = 5; brief psychotic disorder = 1; psychotic disorder not otherwise specified = 19.
b Episodes during follow-up period.
c PANSS, Positive and Negative Symptom Scale.
d CDSS, Calgary Depression Scale for Schizophrenia.
e YMRS, Young Mania Rating Scale.
f GAF-F, Global Assessment of Functioning—functioning subscale.
g AUDIT, Alcohol Use Disorders Identification Test.
h DUDIT, Drug Use Disorder Identification Test.
Altering Clinical Recovery Criteria
Presented in Table 2, we observed progressively lower recovery rates for the total sample as adjustments were made to increase the duration. With a 5-year duration requirement, the recovery rate was halved from the standard duration criteria, and although the recovery rate was still double in the bipolar compared to the schizophrenia spectrum group, it was no longer significantly different.
When adding affective symptom remission as a prerequisite in addition to psychotic symptom remission, the recovery rate decreased to 26.8% for the total sample. In the schizophrenia and bipolar spectrum groups 58.9% and 58.7% respectively, were in affective symptom remission irrespective of psychotic symptom remission or not. The addition of the affective symptom remission requirement did not affect the relative differences in recovery rates between the schizophrenia and bipolar spectrum diagnostic groups, as they decreased with 8.1% and 4.3%, respectively.
Finally, the recovery rate in the total sample increased to 40.8% with less strict criteria for adequate functioning (part-time instead of full-time work/study/other and having a close friend or confidant instead of weekly contact). Recovery rates increased in both diagnostic groups with looser functioning criteria.
Adequate Functioning in Healthy Controls
Compared to the total sample, significantly more controls met the standard and altered criteria for adequate functioning. Yet, as illustrated in Table 2, 18.8% of healthy controls did not meet the standard criteria for adequate functioning, mainly based on restricted social functioning. The rate of healthy controls not fulfilling adequate functioning decreased to 4.3% when using looser functioning criteria.
Discussion
The main findings include that at 10-year follow-up 31.7% of FEP participants were in clinical recovery according to a standard definition, the recovery rate was twice as high in the bipolar (50.0%) compared to schizophrenia spectrum group (22.9%). Altering the criteria affected the recovery rate, it decreased equally for both diagnostic groups with a longer recovery duration and when adding affective remission to the criteria; and increased with less strict criteria for adequate functioning. Finally, 18.8% of healthy controls did not meet the standard criteria for adequate functioning, suggesting that these criteria are too strict.
According to our first aim, the 31.7% clinical recovery rate is in line with previous FEP studies including both nonaffective and affective psychotic disorders.13,17,19 Also in line with the previous studies, psychotic remission was more common than adequate functioning, with not gaining full-time occupational functioning being the largest barrier to meeting the standard criteria for clinical recovery in both diagnostic groups.13,17 As longitudinal research on first-episode psychotic bipolar disorder is limited, the 50.0% recovery rate of this group was positive, suggesting that many in this population are not affected by symptoms and functional impairment 10 years after start of treatment. The lower recovery rate for participants in the schizophrenia spectrum was expected based on previous research,12 although it is worth noticing that the diagnostic subgroups schizoaffective and “other psychoses” fared better than schizophrenia. This is also in line with previous research, and suggestions to replace the “schizophrenia spectrum” with the “psychosis spectrum”.36
More years of education in the bipolar spectrum and clinical recovery groups may partially explain the higher rates of full-time occupation in these two groups. Higher psychotic symptom scores in the schizophrenia spectrum group was anticipated, as they are primary psychotic disorders. However, as found by previous studies,37,38 the schizophrenia spectrum participants demonstrated equal levels of depressive symptoms as the bipolar spectrum participants. This suggests that depression is relevant for both diagnostic groups and supports the dimensional character of these disorders. The higher score on the mania measure for the schizophrenia group is likely explained by an item measuring delusional content.
According to our second aim, we found as expected, that recovery rates decreased with longer duration requirements, especially with a 5-year duration as half of those in recovery with 1-year duration had relapsed during that time. Although the recovery rate was still twice as high in the bipolar compared to the schizophrenia spectrum group when using 5-year duration criteria, the difference in recovery between the diagnostic groups was no longer significant. This suggests proportionally more instability in the bipolar group. Nearly 60% were in affective remission and adding this to the clinical recovery criteria reduced the overall rate equally with around 5% in both diagnostic groups, consistent with the relatively high level of depression in the schizophrenia group. Unsurprisingly, the recovery rate increased with less strict functioning criteria,13 from 31.7% to 40.8% when allowing both less strict criteria for social functioning and part-time occupation.
According to our third aim, we found that many healthy controls met the standard criteria for adequate functioning, as expected due to their high education level and selection based on no familial history of mental illness. However, 18.8% did not meet the full adequate functioning criteria in the standard definition, suggesting that they are too stringent. Not meeting requirements for social functioning was what most hindered healthy controls from meeting the standard adequate functioning criteria, while for FEP participants it was full-time occupation. Perhaps the controls’ demanding schedule with full-time employment in combination with family life hindered them in meeting the strict requirement of weekly social activity.
A consensus definition of clinical recovery for psychotic disorders is required for reliable and valid measurement of outcome in research and treatment of psychosis, in addition to the important personal recovery perspective.10 Some clinical recovery definitions are stringent on purpose to avoid excessively lenient criteria contributing to low expectations and stigmatization.39 Based on our findings, we propose the following criteria for a potential future consensus definition of clinical recovery in psychotic disorders:
Stability is a core criterion for clinical recovery,24 but the required duration might depend on the study purpose. The duration in the RSWG definition of symptom remission is 6 months,11 which has been found suitable for early clinical recovery research.40 Other studies might investigate long-term stability, although a longer duration might fail to capture the episodic nature of these diagnoses.41 We did not find a large difference in recovery rate between one- and two-year duration, nor a difference in number of psychotic episodes during follow-up between participants in recovery and not in recovery. Therefore, a one-year duration seems an appropriate criterion for most longitudinal FEP-studies investigating clinical recovery.
In line with the RSWG consensus definition,11 recovery definitions are restricted to psychotic symptom remission. However, as affective symptoms are primary in affective psychotic disorders and equally common in our schizophrenia spectrum group, including affective symptom remission among the criteria for clinical recovery in FEP, appears more clinically meaningful.
Among the adequate functioning criteria, the majority of our participants fulfilled the standard independent living requirement,24 we, therefore, suggest that it remains a criterion. Requirements for occupational functioning commonly involve employment or study,24 although many studies only require part-time participation.15,16,40 In fact, part-time employment is common in the general population for a range of reasons beyond mental health problems,18,42,43 including 25% of the employed Norwegian general population.44 Accordingly, several of our healthy controls worked part-time due to child-rearing, job market, or somatic disability/sick-leave. Another important issue is that individuals with psychotic disorders face systemic barriers to employment, including mental health stigma and discrimination.42,43 In Norway, lack of adequate work-placement programs and problems transitioning from disability benefits to employment have also been identified.45 Participants in our study may have been subject to systemic barriers, because many, especially with schizophrenia, were not employed even part-time at follow-up. Another important consideration is whether individuals are unable to work or study due to symptoms or functional impairments, or whether they choose part-time work because it is more suitable for their life situation or preferences, in line with the personal recovery perspective. Based on the above discussion of part-time employment in the general population, systemic barriers, and individual preferences, part-time rather than full-time occupational functioning appears a more reasonable criterion for clinical recovery in FEP.
Because social functioning varies across cultures and individual preferences, it is difficult to operationalize, evidenced by definitions ranging from romantic relationship18 to GAF-scores.16 As social withdrawal and anhedonia are common negative symptoms in psychotic disorders, some regular observer-rated social activity is generally suggested.24 Nevertheless, as discussed above, the standard criteria of weekly socializing might be challenging to meet even for high-functioning individuals, as we found in 13.7% of our healthy controls. As it appears too stringent we determined that in the altered criteria having a close friend/confidant would suffice. Because 95.7% of our healthy controls met the altered, looser, functioning criteria, we suggest that they are a more reasonable basis for comparison and thus a better norm of adequate functioning for FEP. Nevertheless, observer-rated social functioning does not measure the individual’s satisfaction with their social life, and might not be culturally sensitive.46 An alternative is to assess social functioning by self-report in addition to observer-rating, although this requires further research.
The present findings have several clinical implications. First, they confirm significant rates of clinical recovery in FEP, especially for individuals with bipolar spectrum disorders. Clinicians must communicate this to service users receiving a psychosis diagnosis as it can contribute to increased hope of recovery and reduced pessimism and stigma, ultimately promoting chances of recovery. Second, the increase in recovery rates from 31.7% to 40.8% with looser criteria, illustrates how recovery rates are partially dependent on how they are defined. This knowledge allows for meaningful conversations with service-users about the many forms that recovery can take. Third, as most of our participants were in psychotic symptom remission, psychosis appears well managed for most. Therefore, regaining functioning and employment early should be of equal focus to symptom management in treatment of psychotic disorders.15
The main strength of our study is the 10-year longitudinal investigation of clinical recovery across a large sample of first-episode psychotic bipolar and schizophrenia spectrum disorders, plus the inclusion of healthy controls. Moreover, we investigated the suitability of existing definitions and alternative criteria. The main limitation is our high attrition rate, perhaps explained by lengthy and extensive baseline and 1-year assessments. Alternatively, follow-up of incident cases may be more challenging than of participants from specific intervention or inpatient settings. However, there were no differences between the group lost to follow-up and completers, except for more men and schizophrenia spectrum disorders in the former group.
To conclude, our findings suggest that half of people with bipolar spectrum disorders and a quarter with schizophrenia spectrum disorders will clinically recover 10 years after treatment start. Additionally, that a more meaningful consensus definition of clinical recovery, suitable also for affective psychosis and more in line with the general population, would benefit from inclusion of affective remission and less stringent criteria for adequate functioning. Ultimately, we highly welcome a debate regarding a future consensus definition of clinical recovery in psychotic disorders.
Funding
This work was supported by grants from the Norwegian Council for Mental Health and the Dam foundation (Rådet for psykisk helse/Stiftelsen Dam) (2020/FO293105); the Regional Health Authority of Eastern Norway (Helse Sør-Øst) (2014/102, 2015/088, 2018/093); and from the Norwegian Research Council (Norges forskningsråd) (181831, 213974, 287714).
Acknowledgments
Study methodology was altered slightly relative to preregistration in the Open Science Framework due to coronavirus delays.
Conflict of Interest
The authors have declared that there are no conflicts of interest in relation to the subject of this study.